Sports cardiology is a growing area in which there are various controversial issues, including the need for guidelines to standardize the assessment of individuals with cardiovascular disease (CVD) and the eligibility criteria for sports participation. The 2020 European Society of Cardiology (ESC) guidelines on sports cardiology and exercise in patients with CVD1 were received with great enthusiasm and expectation, since they contribute to better risk stratification and exercise prescription in the presence of CVD and help minimize the risk of adverse events.
The aim of this study was to analyze the classes of recommendation and levels of evidence (LoE) underlying the 2020 ESC guidelines on sports cardiology and to compare them with other recent ESC guidelines on non-ST elevation myocardial infarction (NSTEMI) (2020), CVD prevention (2021), atrial fibrillation (AF) (2020), valvular heart disease (VHD) (2021), and heart failure (HF) (2021).
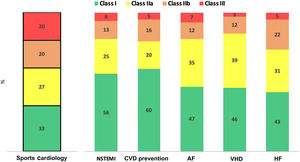
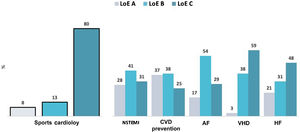
The ESC guidelines on sports cardiology propose a total of 158 recommendations: 52 class I (recommended/indicated) (33%); 43 class IIa (should be considered) (27%); 32 class IIb (may be considered) (20%); and 31 class III (not recommended) (20%). Compared to the other ESC guidelines, the sports cardiology guidelines have fewer class I and more class IIb or III recommendations (Figure 1). For example, the mean frequency in the ESC guidelines on NSTEMI, CVD prevention, AF, VHD and HF are 50% for class I, 30% for class IIa, 13% for class IIb and 6% for class III. The majority of the recommendations on sports cardiology (80%) are based on LoE C (consensus experts’ opinion and/or small studies, retrospective studies or registries), 13% on LoE B (single randomized clinical trial or large non-randomized studies), and only 8% on LoE A (multiple randomized clinical trials or meta-analysis). These results differ from the other ESC guidelines analyzed, in which the mean frequencies are LoE A 21%, LoE B 40%, and LoE C 38% (Figure 2).
Distribution of classes of recommendations in the 2020 European Society of Cardiology (ESC) guidelines on sports cardiology, compared with other ESC clinical guidelines (non-ST elevation myocardial infarction (NSTEMI) (2020), cardiovascular disease (CVD) prevention (2021), atrial fibrillation (AF) (2020), valvular heart disease (VHD) (2021), and heart failure (HF) (2021).
Distribution of level of evidence (LoE) (A, B and C) in the 2020 European Society of Cardiology (ESC) guidelines on sports cardiology, compared with other ESC clinical guidelines (non-ST elevation myocardial infarction (NSTEMI) (2020), cardiovascular disease (CVD) prevention (2021), atrial fibrillation (AF) (2020), valvular heart disease (VHD) (2021), and heart failure (HF) (2021).
These results confirm the current scarcity of evidence in sports cardiology compared to other areas in cardiology, especially in terms of randomized clinical trials, most evidence being based on expert opinion, small studies, retrospective studies or registries. However, previous data showed that even in other areas, only a small proportion of the recommendations in major cardiovascular society guidelines were supported by evidence from randomized clinical trials, a pattern that appears to persist over time.2–4
The fact that sports cardiology is an emerging subspecialty and these ESC guidelines are the first in this field worsens their limitations, as a result of the lack of evidence on the natural history of CVD and the risk of sudden cardiac death during intensive exercise and competitive sport. In this setting, it is difficult to formulate specific recommendations for heterogeneous scenarios, populations and clinical presentations. These guidelines should therefore not be treated simply as a static legal document, but should encourage physicians to integrate the recommendations with their clinical experience and skills in sports cardiology. Given the range of topics that remain to be clarified, the ESC guidelines on sports cardiology emphasize sharing the decision-making process with the athlete/patient, their family, and other health and exercise professionals. This approach is mainly proposed in more controversial cases and should take into consideration the autonomy and preferences of each individual, who should provide clear informed consent.
A call to action on research in sports cardiology is needed to overcome the multiple gaps in evidence, narrow the gray zone and subjectivity in this area, improve the quality of evidence and support future recommendations.
Conflicts of interestThe author has no conflicts of interest to declare.