Although there is evidence that a significant proportion of veteran athletes have coronary atherosclerotic disease (CAD), its prevalence in recreational athletes with low to intermediate cardiovascular (CV) risk is not established. This study aimed to characterize the coronary atherosclerotic burden in veteran male recreational athletes with low to intermediate CV risk.
MethodsAsymptomatic male athletes aged ≥40 years with low to intermediate risk, who exercised >4 hours/week for >5 years, underwent cardiac computed tomography (CT) for coronary artery calcium (CAC) scoring and CT angiography. High coronary atherosclerotic burden was defined as at least one of the following: CAC score >100; CAC score ≥75th percentile; obstructive CAD; disease involving the left main, three vessels or two vessels including the proximal left anterior descending artery; segment involvement score >5; or CT Leaman score ≥5. Athletes were categorized by tertiles of exercise volume, calculated by metabolic equivalent of task (MET) scores.
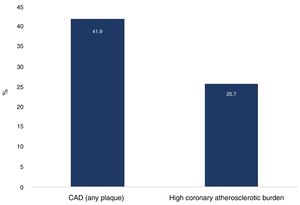
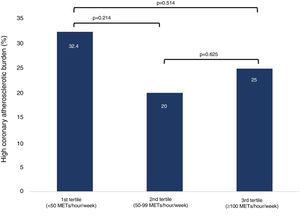
ResultsA total of 105 athletes were included, all with SCORE <4%, mainly engaged in high-dynamic sports. Median exercise volume was 66 (44-103) METs/hour/week, with 8±5 hours training/week and 17±10 years of exercise. A high coronary atherosclerotic burden was present in 27 (25.7%) athletes. Ten (9.5%) athletes had CAC score >100, 13 (12.4%) had CAC score ≥75th percentile and six (5.7%) had obstructive lesions. The extent and severity of coronary plaques did not differ according to exercise volume.
ConclusionsThe prevalence of subclinical CAD detected by cardiac CT in veteran male recreational athletes with low to intermediate CV risk was high. Up to a quarter of our cohort had a high coronary atherosclerotic burden.
Apesar de estar descrita uma proporção significativa de atletas veteranos com doença arterial coronária aterosclerótica (DAC), a sua prevalência em atletas de nível recreativo com risco cardiovascular (CV) baixo-intermédio não está esclarecida. O objetivo deste estudo foi caracterizar a carga aterosclerótica coronária em atletas veteranos do género masculino de nível recreativo com risco CV baixo-intermédio.
MétodosAtletas assintomáticos do género masculino com ≥40 anos com risco baixo-intermédio, praticantes de >4horas/semana de exercício durante >5 anos, realizaram tomografia computorizada cardíaca com determinação do score de cálcio (ScCa) e angiografia coronária (Angio-TC). Definiu-se elevada carga aterosclerótica coronária a presença de pelo menos uma das seguintes características: ScCa >100; ScCa≥p75 (percentil); DAC obstrutiva; doença envolvendo tronco comum, 3-vasos ou 2-vasos incluindo a artéria descendente anterior proximal; segment involvement score >5; CT-adapted Leaman score ≥5. Os atletas foram categorizados em tercis de volume de exercício, calculado por Metabolic Equivalent Task (MET) scores.
ResultadosForam incluídos 105 atletas, todos com score <4%, principalmente envolvidos em desportos de elevada componente dinâmica. A mediana de volume de exercício foi 66 [44; 103] METs/h/semana, com 8±5 horas-treino/semana e 17±10 anos de exercício. Uma elevada carga aterosclerótica coronária foi detetada em 27 (25,7%) atletas. Dez (9,5%) atletas tinham ScCa>100, 13 (12,4%) ≥p75 e 6 (5,7%) lesões obstrutivas. A extensão e a gravidade das placas coronárias não diferiram de acordo com o volume de exercício.
ConclusõesA prevalência de DAC subclínica detetada por Angio-TC cardíaca em atletas veteranos do género masculino de nível recreativo com risco CV baixo-intermédio foi elevada. Um quarto da nossa amostra apresentou uma elevada carga aterosclerótica coronária.
The cardiovascular (CV) benefits of physical activity and exercise training are established.1,2 Participation in organized sports activities at recreational and competitive level has increased among middle-aged individuals in the last decade. Additionally, the number of veteran athletes engaging in lifelong high-dynamic sports is increasing.3
There is emerging evidence that veteran athletes (>40 years old) with a low atherosclerotic risk profile have a higher coronary artery calcium (CAC) score than comparatively sedentary counterparts of similar age and atherosclerotic risk profile.4
Additionally, recent studies report a positive relationship between the prevalence of atherosclerotic coronary artery disease (CAD) and exercise intensity. These studies have focused largely on competitive athletes, many of whom have achieved national or international recognition, but most deaths in sport occur in recreational male athletes in the fifth decade of life, and up to 80% are due to CAD.5–8 The prevalence of CAD in veteran recreational athletes with a low to intermediate risk profile has not been characterized, but the CAC score in individuals with an intermediate atherosclerotic risk has a significant prognostic value compared with conventional clinical risk factors.9–15
This study aimed to characterize the coronary atherosclerotic burden in veteran athletes with low to intermediate CV risk by cardiac computed tomography (CT).
MethodsStudy design and populationVeteran male athletes (≥40 years old) who had participated in regular recreational exercise for at least four hours a week for a minimum of five years were enrolled in this observational study performed in two centers. Athletes with symptoms, diabetes, Systematic Coronary Risk Estimation (SCORE) ≥5%, renal impairment or previous allergy to iodinated contrast agents were excluded. The initial assessment regarding eligibility to participate was performed in a sports cardiology clinic, with physical examination and documentation of demographic and anthropometric characteristics, atherosclerotic risk factors, family history and sports history. The CV risk factors included were family history of premature CV disease (first-degree relatives aged <50 years), smoking (current if smoking in the last year), hypertension (≥140/90 mmHg or treatment with antihypertensive medications), and dyslipidemia (low-density lipoprotein cholesterol ≥115 mg/dl or treatment with lipid-lowering medications). These characteristics were assessed and applied in the SCORE charts.16 All athletes underwent blood tests, 12-lead resting electrocardiogram, transthoracic echocardiogram and exercise testing. The study was approved by the relevant ethics committees and all individuals gave their informed consent for participation.
Exercise assessmentExercise volume was assessed by the metabolic equivalent of task (MET) score (METs/hour/week), calculated as the product of intensity, frequency and duration of exercise. Exercise intensity was established by the METs for each reported sport according to the Compendium of Physical Activities.17 Exercise frequency was defined as the number of training sessions per week, and duration was defined by the number of hours spent in each workout. Exercise volume was classified by tertile. Sports disciplines were grouped according to the Mitchell classification,18 with particular attention being paid to sports characterized by high-dynamic (class C) and high-static (class III) components. We also recorded participation in organized competitions and the number of years of continuous exercise training, specifically identifying athletes with more than 20 years’ activity.
Coronary computed tomography angiographyCoronary atherosclerotic burden was determined by CAC score and coronary CT angiography (CCTA), using multidetector (≥64-slice) CT scanners (SOMATOM Force and SOMATOM Perspective, Siemens Healthcare Inc.), in order to minimize radiation and contrast doses. Except when contraindicated, sublingual nitroglycerin (0.5 mg) was administered, and beta-blockers were used when appropriate (heart rate >65 bpm). A cardiologist and a radiologist with level III-equivalent experience analyzed all scans, which were processed on a workstation (syngo.via, Siemens Healthcare Inc.). Abnormal findings were reviewed by consensus.
CAC scores were determined in absolute terms and also expressed as percentiles, according to nomograms adjusted for age, gender and ethnicity.19 The presence of coronary plaque, plaque morphology, plaque distribution (Society of Cardiovascular Computed Tomography classification20) and degree of stenosis were ascertained with CCTA to calculate the segment involvement score (SIS) and CT Leaman score (CT-LeSc).21–23 The SIS is a semi-quantitative measure of atherosclerotic burden, representing the number of coronary segments with plaques; it is considered significant if more than five segments are involved. As previously described, the CT-LeSc is calculated from three sets of weighting factors provided by CCTA: (1) location of plaques in the coronary tree, taking dominance into account; (2) type of plaque; (3) degree of stenosis.22 CT-LeSc ≥5 was defined as significant. To identify athletes with a higher atherosclerotic burden, a variable was created that combined the presence of at least one of the following characteristics: CAC score >100 Agatston units (AU); CAC score >75th percentile; obstructive CAD (≥50% luminal stenosis); presence of plaques in the left main (LM), three vessels or two vessels involving the proximal left anterior descending artery (LAD); SIS >5; or CT-LeSc ≥5.
Statistical analysisAll analyses were performed using IBM SPSS for Mac version 23.0 (IBM SPSS, Inc., Chicago, IL). Normality was tested with the Kolmogorov-Smirnov test. Continuous variables with normal distribution were expressed as means and standard deviation and non-normal variables as median (interquartile range). Categorical variables were expressed as frequencies and percentages. Statistical comparisons were performed using the chi-square test or Fisher's exact test, when appropriate, for categorical variables, and the Mann-Whitney or Kruskal-Wallis test for continuous variables. A p-value <0.05 was considered statistically significant.
ResultsDemographics and clinical and exercise historyA total of 105 athletes were studied (Table 1). Almost all (98.1%) were white. Their mean age was 48±6 (41-61) years, 60% aged between 40 and 50 years, and 40.0% over 50 years. Most (n=56; 53.3%) had low CV risk (SCORE=0), while the remainder had intermediate risk (SCORE 1-3%; SCORE=1 in 73%). Forty-nine (46.7%) athletes had at least one CV risk factor, most often dyslipidemia, which was present in 43 (41.0%). Most were engaged in sports modalities characterized by high-dynamic exercise (n=88; 83.8%), especially running (n=67; nine short, 41 middle and 17 long distance), cycling (n=11) and weight-lifting (n=10); approximately a quarter (n=26; 24.8%) participated occasionally in organized sports events. Median exercise volume was 66 (44-103) METs/hour/week, with a mean of 8±5 hours training/week (16.2%>10 hours) and a mean of 17±10 years (31.4% with continuous training >20 years).
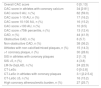
Baseline and exercise-related characteristics (n=105).
| Demographic and clinical characteristics | |
| Caucasians, n (%) | 103 (98.1) |
| Age, years | 48±6 |
| Height, cm | 176±6 |
| Weight, kg | 76±9 |
| BSA, m2 | 1.9 [1.8; 2.0] |
| SBP, mmHg | 125±11 |
| DBP, mmHg | 78±8 |
| Heart rate, bpm | 57±8 |
| CV risk factors | |
| Family history of premature CV disease, n (%) | 3 (2.9) |
| Current smoking, n (%) | 8 (7.6) |
| Former smoking, n (%) | 10 (9.5) |
| Hypertension, n (%) | 9 (8.6) |
| Dyslipidemia, n (%) | 43 (41.0) |
| LDL cholesterol, mg/dl | 124±31 |
| Lipid-lowering medication, n (%) | 7 (6.7%) |
| ≥1 CV risk factor, n (%) | 49 (46.7) |
| Low risk (SCORE <1%), n (%) | 56 (53.3) |
| Exercise-related characteristics | |
| High dynamic sport (class C), n (%) | 88 (83.8) |
| High static sport (class III), n (%) | 32 (30.5) |
| Hours of training/week | 8±5 |
| >10 hours of training/week, n (%) | 17 (16.2) |
| Volume of exercise, METs/hours/week | 66 [44-103] |
| Years of continuous exercise | 17±10 |
| >20 years of continuous exercise, n (%) | 33 (31.4) |
CV: cardiovascular; BSA: body surface area; DBP: diastolic blood pressure; LDL: low-density lipoprotein; SBP: systolic blood pressure.
The total mean radiation and contrast doses were 2.7±1.8 mSv and 110±19 ml, respectively. There were no major adverse reactions during CCTA. Cardiac CT results are shown in Table 2. Sixty-two (59.0%) athletes had zero CAC score. Ten (9.5%) had a CAC score >100 AU and 13 (12.4%) had a CAC score exceeding the 75th percentile. Forty-four (41.9%) athletes had coronary plaques, of whom six (5.7%) had obstructive lesions. Among athletes with CAD, 10 (22.7%) had LM disease (seven with concomitant lesions in other arteries), four (9.1%) had three-vessel disease, 10 (22.7%) had two-vessel disease and 20 (45.5%) had single-vessel disease. Twenty-four (22.9%) athletes had lesions in the LM, three vessels, or two vessels involving the proximal LAD.
Cardiac computed tomography results (n=105).
| Overall CAC score | 0 [0; 13] |
| CAC score in athletes with coronary calcium | 34 [2-81] |
| CAC score 0 AU, n (%) | 62 (59.0) |
| CAC score 1-10 AU, n (%) | 17 (16.2) |
| CAC score 10-100 AU, n (%) | 16 (15.2) |
| CAC score >100 AU, n (%) | 10 (9.5) |
| CAC score >75th percentile, n (%) | 13 (12.4) |
| CAD, n (%) | 44 (41.9) |
| Obstructive CAD, n (%) | 6 (5.7) |
| Non-obstructive CAD, n (%) | 38 (36.2) |
| Athletes with non-calcified/mixed plaques, n (%) | 15 (14.3) |
| >1 coronary plaque, n (%) | 30 (28.6) |
| SIS in athletes with coronary plaques | 2 [1; 3] |
| SIS >5, n (%) | 4 (3.8) |
| LM-3v-2vpLAD, n (%) | 24 (22.9) |
| CT-LeSc | 0 [0-2.8] |
| CT-LeSc in athletes with coronary plaques | 3.1 [2.2-5.4] |
| CT-LeSc ≥5, n (%) | 16 (15.2) |
| High coronary atherosclerotic burden, n (%) | 27 (25.7) |
AU: Agatston units; CAD: coronary artery disease; CAC: coronary artery calcium; CT-LeSc: computed tomography Leaman score; LM-3v-2vpLAD: disease of left main, three vessels or two vessels involving the proximal anterior descending artery; SIS: segment involvement score.
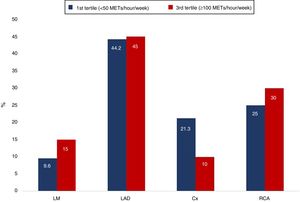
A total of 107 plaques were distributed throughout the coronary tree, 51 (47.7%) in the LAD, 26 (24.3%) in the right coronary artery, 20 (18.7%) in the circumflex and 10 (9.3%) in the LM. The majority of these plaques were calcified (73.8%), while 23.4% were of mixed morphology and 2.8% were non-calcified. The median SIS was 2 and median CT-LeSc was 3.1 (2.2-5.4); four (3.8%) athletes had SIS>5 and 16 (15.2%) had CT-LeSc ≥5.
Overall, a high coronary atherosclerotic burden was present in 27 (25.7%) athletes (Figure 1). Among those with this high burden, 11 (40.7%) had at least one CV risk factor and only six (22.2%) had significant abnormal findings on exercise testing, of whom three (11.3%) were positive for myocardial ischemia.
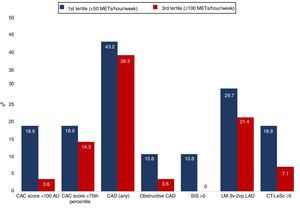
Although not statistically significant, a high coronary atherosclerotic burden was more frequent in the first and third tertiles of exercise volume (first tertile <50 METs/hour/week, second tertile 50-99 METs/hour/week and third tertile ≥100 METs/hour/week) (Figure 2). The distribution of plaques in the coronary tree (Figure 3) and the various cardiac CT-derived indices (Figure 4) were not significantly different according to whether the exercise volume was low (first tertile) or high (third tertile).
Distribution of cardiac computed tomography-derived indices according to exercise volume (first and third tertiles; all p>0.05). AU: Agatston units; CAC: coronary artery calcium; CAD: coronary artery disease; CT-LeSc: computed tomography Leaman score; LM-3v-2vpLAD: disease of left main, three vessels or two vessels including proximal left anterior descending artery; SIS: segment involvement score.
CCTA detected anomalous coronary artery origin in two athletes (right coronary artery with origin in the left ostia and interarterial course; circumflex artery originating in the right ostia with shared ostium) and myocardial bridging in three athletes, all located in the mid segment of the LAD.
Athletes with higher than expected coronary atherosclerotic burden were given lifestyle recommendations and advised to contact their general practitioner. Thirteen athletes were started on a statin. Participants with obstructive lesions underwent myocardial perfusion scintigraphy; no myocardial ischemia was detected. In general, athletes in whom significant CAD was found were not discouraged from continuing to exercise, but were advised to refrain from vigorous exercise. The athlete with a malignant coronary artery origin had no documented ischemia and was advised to limit exercise training to sports with low intensities.
DiscussionIn the present study of predominantly recreational veteran male athletes with a low to intermediate atherosclerotic risk profile, the prevalence of subclinical CAD detected by cardiac CT was relatively high. A quarter of the population had high coronary atherosclerotic burden.
Prevalence of coronary artery disease in veteran athletesThis paradoxical high prevalence of CAD in athletes has also been reported in previous studies. The Marathon Study4 conducted in 108 marathon runners showed higher CAC scores than in non-runners when matched for Framingham risk score. In this study, a significant proportion of athletes had established risk factors for CAD.
Among 50 male marathon runners studied by Tsiflikas et al.,5 half had CAD, 8% had moderate to significant disease and 10% had CAC score >100 AU, which is similar to our results. Since athletes completing only one marathon were also included in this study, the results may be more applicable to real-life situations, as individuals with no or minimal long-distance running experience constitute an important group of participants in endurance events. In our study, we assessed recreational athletes involved in regular exercise training, frequently with high volumes. However, there were significant differences in the baseline characteristics of their population that limit comparisons, with older athletes (>45 years) and a higher prevalence of CV risk factors, such as smoking and family history of CV disease, than in our study.
Of 318 asymptomatic sportsmen included in the MARC study,6 16.4% had CAC score ≥100 AU and 63.2% had atherosclerosis on CCTA (5.3% with ≥50% stenosis). Overall, significant CAD (CAC score ≥100 AU or ≥50% luminal stenosis) was present in almost one in five individuals. The higher prevalence of CAD in this population may be related to their older age (55±6 years) and higher risk profile. Although the majority of participants had SCORE <5%, patients with diabetes were not excluded and the frequency of other risk factors, particularly a family history of CV disease and former smoking, was considerably higher than in our study and the others discussed above.
Merghani et al.7 studied 152 master athletes without CV risk factors (aged 54±9 years, 70% male), mainly runners with lifelong exposure to exercise. Among male athletes, 19% had a CAC score ≥100 AU, while on CCTA 42% were identified with CAD (any plaque), 22% multivessel disease and 7.5% obstructive CAD. Similarly to our findings, most coronary plaques were calcified and located in the LAD. The results of this study performed in high-level athletes without CV risk factors suggest that the higher atherosclerotic burden in previous studies may reflect a higher atherosclerotic risk profile rather than a potential deleterious exercise effect. Recently, a study by Aengevaeren et al.8 in 283 veteran athletes (aged 55±7 years) also showed a high atherosclerotic burden, with coronary artery calcification present in 53% of them.
The differences in the populations included and the methodologies adopted for assessment of exercise and atherosclerotic burden limit direct comparisons and extrapolations. Our study is the only one in which several prognostically validated cardiac CT-derived indices were applied to carry out a detailed characterization of coronary atherosclerotic burden.21,23 This more detailed assessment may offer advantages in risk stratification and early identification of athletes with accelerated atherosclerosis, who may be more prone to have acute coronary events.
Relationship between exercise-related characteristics and coronary artery diseaseSome authors have described a U-shaped curve for the relationship between exercise volume and the development of various clinical conditions, including CAD.9,24–26 To date, this hypothesis has not been rigorously tested, and the causal mechanisms remain unknown, with several limitations and inconsistencies between studies. In the Copenhagen City Heart Study,27 moderate-volume jogging was associated with lower mortality than a sedentary lifestyle or higher-volume jogging. By contrast, analysis of a subgroup of the FIT Project study28 showed a significant reduction in all-cause mortality in middle-aged individuals with higher exercise capacity compared with those exercising at lower workloads, which is conventionally associated with maximum benefit. In a meta-analysis including more than 650 000 individuals with a median age of 62 years, exercising up to 10 times the recommended levels was not associated with increased mortality.29
A previous study revealed significantly higher CAC scores in athletes than in controls after adjustment for the Framingham risk score, but did not show a significant relationship between CAD and measures of physical activity.4 In the study by Merghani et al.,7 the number of years of training was an independent predictor of significant CAD in male athletes, but there was no significant relationship between exercise volume and coronary atherosclerosis. Our study revealed a higher frequency of high coronary atherosclerotic burden in the first and third tertiles of exercise volume, but we were also unable to demonstrate significant differences.
As in two previous studies,7,9 we also demonstrated that most of our athletes with significant CAD had calcified plaques, which may indicate that different pathophysiological mechanisms may be responsible for plaque formation in athletes versus sedentary individuals. The stable nature of the plaques could mitigate the risk of plaque rupture, explaining the increased longevity of athletes despite the high proportion of coronary plaques in the most active.
Role of cardiac computed tomography in pre-participation assessmentThe main objective of assessment of veteran athletes is CV risk stratification, focusing on early detection of CAD, the leading cause of sudden cardiac death in this population. Risk stratification based on clinical characteristics has limitations, and more objective markers have been proposed to improve the detection of individuals with higher risk.9,10 In our study, the presence of risk factors and positive exercise testing for myocardial ischemia had a low discriminative value to identify individuals with higher atherosclerotic burden. Regarding cardiac CT, CCTA showed incremental value over the CAC score for identifying individuals with subclinical CAD. Our results show a high coronary atherosclerotic burden in a significant proportion of athletes with low to intermediate CV risk, giving new insights into the assessment and characterization of coronary atherosclerotic burden by applying several cardiac CT-derived indices previously validated in other populations.
The prognostic impact of CAC scoring in predicting CV events is well known, being independent of and additional to conventional risk factors.12,13 In the MESA study,15 CAC scores showed a higher predictive power than other markers in defining and reclassifying CV risk in intermediate-risk individuals. Additionally, the CAC score promotes the adoption of preventive measures, leading to better control of various risk factors. Beyond detection of obstructive CAD, CCTA provides additional information with prognostic impact, such as non-obstructive plaques, as shown in the landmark CONFIRM Registry, and markers of atherosclerotic burden such as the SIS and CT-LeSc.21,23,30 Clustering information such as location, type of plaque, degree of luminal stenosis and number of plaques in these atherosclerotic burden scores, as performed in the present study, can identify athletes who may potentially be at higher risk of CV events.22
LimitationsOur study has several limitations. We did not include controls or female athletes. We focused predominantly on dynamic sports. Although we performed a more detailed and objective characterization of exercise volume than in previous studies, this assessment was based on athlete recall. The size of our cohort may have been underpowered to test the relationship between exercise volume and the prevalence or severity of CAD. It is also possible that the higher CAD burden in some of our athletes may have been due to previous risk factors for atherosclerosis which improved with exercise training. This study was cross-sectional and cannot be used to infer that the increased atherosclerotic risk burden equates to an increased risk of adverse cardiac events. Finally, we did not test for the use of performance-enhancing agents that may have contributed to our findings.
ConclusionsIn the present study of middle-aged male recreational athletes with a low to intermediate atherosclerotic risk profile, the prevalence of subclinical CAD detected by cardiac CT was high. A quarter of the population had a high coronary atherosclerotic burden. The extent and severity of CAD were not associated with exercise duration or intensity.
Conflicts of interestThe authors have no conflicts of interest to declare.