A 64-year-old woman was admitted for non-ST elevation myocardial infarction. The coronary angiogram showed a severe stenosis in the left anterior descending artery (LAD) ostium. A 3.5 mm×18 mm everolimus-eluting stent was directly deployed in the left main and proximal LAD, with significant jailing of the circumflex (Cx) ostium. A 3.25 mm×11 mm everolimus-eluting stent was therefore deployed in the Cx using the T-stenting and small protrusion technique. One year later, the patient was readmitted for non-ST elevation myocardial infarction, and the coronary angiogram showed ostial restenosis of the Cx stent. Optical coherence tomography imaging confirmed the severity of ostial restenosis. Percutaneous coronary intervention by a radial approach was performed using a sheathless guide catheter.
Uma mulher de 64 anos foi admitida por enfarte do miocárdio sem elevação do segmento ST. A angiografia coronária mostrou uma estenose grave no óstio da artéria descendente anterior esquerda. Foi implantado um stent com 3,5 mm×1,8 mm revestido com everolimus diretamente no tronco comum e na artéria descendente anterior proximal com uma limitação significativa de óstio na artéria circunflexa (Cx). Portanto, foi implantado um stent revestido com everolimus na Cx utilizando a técnica de T-stenting e de pequena protrusão. Um ano mais tarde, o doente foi readmitido por enfarte do miocárdio sem elevação do segmento ST, tendo a angiografia coronária revelado reestenose no óstio do stent na Cx. A tomografia de coerência ótica confirmou a gravidade da reestenose do óstio. Foi realizada uma intervenção coronária percutânea através de abordagem radial, utilizando um cateter sem bainha.
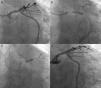
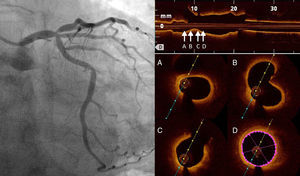
A 64-year-old woman was admitted for non-ST elevation myocardial infarction. The coronary angiogram showed a severe stenosis in the left anterior descending artery (LAD) ostium (Figure 1, left); the left main (LM), circumflex (Cx) and ramus intermedius formed a trifurcation together with the LAD, and were apparently free from disease. Ad hoc percutaneous coronary intervention (PCI) was initiated by a left radial approach using a Judkins Left 4 6F guide catheter and placing one BMW guidewire in the LAD and another in the Cx. Optical coherence tomography (OCT) was performed to evaluate the Cx ostium before LAD stenting; no significant disease was present in the ostium or proximal segment of this artery (Figure 1, right). A 3.5 mm×18 mm everolimus-eluting stent was directly deployed in the LM and proximal LAD, with significant jailing of the Cx ostium but without flow impairment (Figure 2A). Given the size of the jailed vessel, we decided to optimize the result; the Cx was then rewired and dilatation with a 2 mm×10 mm balloon was performed, but no improvement in Cx jailing was achieved. A 3.25 mm×11 mm everolimus-eluting stent was therefore deployed in the Cx using the T-stenting and small protrusion (TAP) technique1 (Figure 2B). In an attempt to optimize the bifurcation result, we attempted to postdilate the LM-LAD stent, but only a 1.5 mm balloon would cross. We then changed the guide catheter to an Amplatzer Left 1 to enhance backup and a BMW guidewire was advanced to the distal LAD, allowing postdilatation with a 4 mm wide balloon (Figure 2C). Final kissing balloon (FKB) inflation could not be performed due to the inability to advance a guidewire to the Cx. The final angiographic result was considered optimal (Figure 2D).
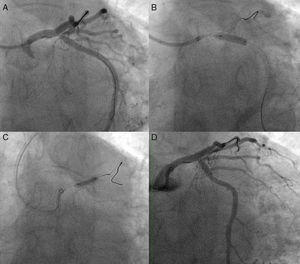
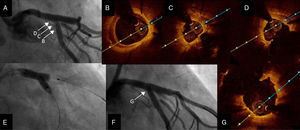
One year later, the patient was readmitted for non-ST elevation myocardial infarction, and the coronary angiogram showed ostial restenosis of the Cx stent (Figure 3A). OCT was performed to better characterize the severity of restenosis and to plan the appropriate revascularization strategy. This technique showed an area of severe restenosis and underexpansion of the Cx ostial stent (Figure 3B-D). In the LM the stent was well apposed and expanded, with only an area of non-significant neointimal growth evident in the proximal stent segment. It was decided to perform percutaneous treatment using a left radial approach and a 7.5F sheathless PB 3.5 Eaucath® (Asahi Intecc) guide catheter. Two guidewires were advanced (LAD and Cx) and the Cx ostium was dilated with a 2 mm×15 mm balloon and a 3.5 mm×15 mm paclitaxel-eluting balloon. The procedure was successfully completed by kissing dilatation with 3.5 mm×15 mm balloons in the LAD and Cx (Figure 3E). The angiographic and OCT result was optimal (Figure 3F and G). At 12-month follow-up, the patient remained asymptomatic.
Second procedure. (A) Angiography showing ostial restenosis of circumflex stent; (B-D) optical coherence tomography (OCT) imaging assessing severity of restenosis, showing underexpansion as the underlying mechanism; (B) proximal circumflex, (C) ostial circumflex, (D) ostial circumflex and bifurcation with left anterior descending artery; (E) kissing balloon inflation; (F and G) final angiography and OCT imaging showing good result.
The present case illustrates the usefulness of a sheathless guide catheter when performing complex PCI by a radial approach. The wider lumen of this catheter facilitated the treatment of underexpansion and restenosis of the ostial Cx in the setting of previous LM bifurcation stenting. Unlike the first PCI, in which a 6F guide was used, the second procedure using a 7.5F sheathless catheter allowed kissing balloon inflation, obtaining an optimal angiographic result.
Even in non-complex bifurcation PCI it is mandatory to assure that the guide catheter has sufficient diameter and back-up strength to avoid technical problems during the procedure. The radial approach may limit two these essential points when choosing the guide, and crossover to femoral access is frequent in complex settings. Sheathless guide catheters remove the need for an introducer sheath, thus providing a wider guide lumen with a smaller outer diameter than the conventional introducer and guide approach. This characteristic makes them a valuable tool to improve success in complex PCI performed by radial access. Some series have shown high procedural success with this kind of catheter, including in 43 cases of bifurcation PCI (33 of them with LM disease) reported by Li et al., with a good safety profile.2–4
This case illustrates a pure LAD ostial stenosis with no involvement of the LM or ostial Cx (0:1:0 on the Medina classification). When dealing with this kind of lesion, accurate ostial stent placement is challenging, and frequently not feasible if the angle differs from 90°, when the proximal end of the stent can protrude into the LM or stay too far inside the side branch, thus leaving part of the ostium uncovered. In the present case, given that the LM and LAD diameters were similar and the Cx ostium was free from disease, we chose to stent from the LM to the proximal LAD to assure complete lesion coverage. Provisional stenting is the preferred choice for the treatment of this kind of bifurcation, as it is associated with better outcomes. Predictors of side branch compromise such as stenosis of bifurcation core, high bifurcation angle, side branch ostial disease or high main branch/side branch diameter ratio, were absent in this case.6 However, severe Cx jailing was observed after stenting. In this setting, this compromise is probably related to carina shift rather than plaque shift,7 which may be avoided by guiding the choice of stent diameter with the distal vessel diameter and using a proximal optimization technique, followed if necessary by side branch dilatation and FKB.5 In our case, we switched to a two-stent strategy due to persistent angiographic jailing despite side branch dilatation. We think TAP was an appropriate choice in this case, but angiography showed excessive proximal protrusion of the Cx stent into the LM, and deformation of the LM-LAD stent (Figure 2B). Given this metal excess in the bifurcation it would be advisable to perform FKB, however in the initial procedure it was not even possible to change to a stiff guidewire; it is noteworthy that FKB cannot be achieved in 9-36% of cases depending on the series.5,8 By contrast, in the second procedure, the use of a wider sheathless catheter that increases back-up and support enabled successful PCI using the radial approach. It should be noted that several other factors may have contributed to the success of this second procedure, and other techniques may enhance PCI success by a transradial approach, but undoubtedly the use of this sheathless guide provided important advantages in this case.
ConclusionSheathless guide catheters provide a wider lumen with a smaller outer diameter, thus offsetting some of the limitations of the radial approach, and enhancing the chances of success in complex PCI procedures such as those including LM disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.