Coronary chronic total occlusions (CTOs) of the right coronary artery (RCA) are a relatively common finding in the context of coronary angiography. However, the benefit of revascularization remains controversial.
MethodsA single-center retrospective cohort analysis prospectively collected outcomes of CTO patients undergoing percutaneous coronary intervention (PCI) in 2019 and 2020. Patients were divided into two groups according to the CTO vessel treated (left coronary artery [LCA]-CTO or RCA-CTO). The primary outcome was defined as the recurrence of angina and/or heart failure (HF) symptoms and secondary outcomes were myocardial infarction (MI) and all-cause mortality.
ResultsA total of 177 patients (82.5% male) were included in the analysis, with a mean age of 65±11 years. The primary outcome occurred in 28 (16.6%) patients and was significantly more frequent in RCA-CTO patients (19, 24.7%, p=0.010) in a mean follow-up of 18 months. This was mainly driven by recurrence of HF symptoms (12, 15.6%, p=0.013). Treated RCA-CTO was an independent predictor of the primary outcome (p=0.019, HR 2.66, 95% CI 1.17–6.05). MI and mortality rates were no different between groups (RCA-CTO with 1.3%, p=0.361 and 2.6%, p=0.673, respectively, on survival analysis). Left ventricular ejection fraction was an independent predictor of mortality (p=0.041, HR 0.93, 95% CI 0.87–0.99).
ConclusionsRevascularization of CTO lesions by PCI was associated with low rates of symptom recurrence, and clinical outcomes showed no differences regardless of which artery was treated. Recanalization of RCA-CTO was less beneficial in reducing the recurrence of HF symptoms.
As oclusões totais crónicas (CTO) da artéria coronária direita (RCA) são um achado relativamente comum no contexto da angiografia coronária, porém o benefício da sua revascularização por intervenção coronária percutânea (PCI) permanece controverso. O nosso objetivo foi tentar responder a esta questão.
MétodosEstudo de coorte retrospetivo realizado em doentes com CTO submetidos a PCI entre 2019-2020. Formados dois grupos (artéria coronária esquerda (LCA)-CTO e RCA-CTO). O outcome primário foi definido como a recorrência de sintomas (angor e/ou insuficiência cardíaca [IC]) e como outcomes secundários a ocorrência de enfarte do miocárdio (MI) e mortalidade por todas as causas.
ResultadosAnálise com 177 doentes, idade média de 65±11 anos e 82,5% do sexo masculino. O outcome primário ocorreu em 28 (16,6%) doentes, mais frequente no grupo RCA-CTO (19, 24,7%, p=0,010), nomeadamente sintomas de IC (12, 15,6%, p=0,013), durante um seguimento médio de 18 meses. O tratamento da RCA-CTO foi um preditor independente do outcome primário (p=0,019, HR 2,66, 95% CI 1,17 a 6,05). A ocorrência MI e mortalidade não mostrou diferenças entre os grupos (RCA-CTO 1,3%, p=0.361 e 2,6%, p=0,673, respetivamente - análise de sobrevivência). A função ventricular esquerda foi um preditor independente de mortalidade (p=0,041, HR 0,93, 95% CI 0,87 a 0,99).
ConclusõesA revascularização percutânea de CTO foi associada a uma reduzida taxa de recorrência de sintomas e os outcomes clínicos não evidenciaram diferenças independentemente da artéria tratada. Porém, o benefício na recorrência de sintomas de IC parece ser menor no grupo CRA-CTO.
Coronary chronic total occlusions (CTOs) are relatively common in patients undergoing coronary angiography (CA), but reports of ideal treatment strategies and their clinical benefits have been inconsistent.1–4 Medical therapy is often the first treatment option for patients with single-vessel coronary artery disease (CAD) classified as a CTO. For patients with multivessel CAD including a CTO, revascularization of significant non-CTO lesions is added to medical therapy as the usual standard of care.1,4–6
Ongoing advances in technology allied to increased experience of dedicated teams have contributed to the success of CTO revascularization through percutaneous coronary intervention (PCI). However, CTO recanalization represents less than 5% of PCI in clinical practice, which is probably related to higher rates of complications and greater procedural complexity.2,7–9
Recent data have shown improvements in quality of life and CAD-related symptoms in CTO patients undergoing PCI. Although survival results in the literature are not statistically significant, CTO lesions have been found to be a strong independent predictor of incomplete revascularization in patients undergoing PCI.2,4,10–12
The right coronary artery (RCA) is one of the arteries most affected by CTO lesions treated by PCI. The clinical benefits of recanalization have been demonstrated in a small, randomized controlled trial (RCT) and in patients with isolated RCA-CTO, although with no improvement in survival.13 The lack of larger trials and data from observational studies, especially in patients with multivessel CAD, has influenced the treatment of RCA-CTO lesions, which remains controversial.
ObjectivesThe aim of this study was to analyze the effect on clinical outcomes and symptom recurrence in CTO patients undergoing percutaneous revascularization of the RCA. Additionally, it aimed to identify independent predictors of symptom recurrence and clinical outcomes in this population.
MethodsThis was a single-center retrospective cohort study of CTO patients undergoing PCI in 2019 and 2020.
Patient selectionPatients were eligible for the study if they were aged 18 years or over and reported symptoms suggestive of ischemic heart disease in which a significant atherosclerotic vessel lesion was identified and CA and classified as CTO, i.e. a coronary lesion with Thrombolysis In Myocardial Infarction (TIMI) anterograde flow score of 0 with chronic characteristics thought to have been present for at least three months. Patients who only underwent a diagnostic study, despite having a CTO vessel, or had an unsuccessful procedure were excluded from the analysis. A previously published hybrid algorithm for CTO PCI was used for revascularization, and patients were divided into two groups according to the CTO vessel: left coronary artery (LCA)-CTO or RCA-CTO.7,14 Left ventricular ejection fraction (LVEF) was estimated by the modified Simpson's biplane method. Obesity was defined as a body mass index ≥30 kg/m2, and chronic renal failure was defined as creatinine clearance <60 ml/m2 (Cockcroft–Gault formula). The use of at least one antianginal drug, an angiotensin-converting enzyme inhibitor/angiotensin receptor blocker/angiotensin receptor-neprilysin inhibitor, aspirin (or anticoagulation in atrial fibrillation), dual antiplatelet therapy or dual antithrombotic therapy for at least six months, and a lipid-lowering drug (statin and/or ezetimibe) were defined as optimal medical therapy (OMT). Baseline patient demographic data, cardiovascular risk factors, and clinical, laboratory, echocardiographic and angiographic data were also recorded.
The study was conducted according to the ethical principles stated in the 1975 Helsinki Declaration and was approved by the local hospital ethics committee.
OutcomesThe primary outcome was recurrence of angina and/or heart failure (HF) symptoms (total symptom recurrence) in a two-year follow-up. HF symptoms were defined as dyspnea and/or fatigue presumed to be secondary to an underlying heart condition. Secondary outcomes were defined as myocardial infarction (MI) and all-cause mortality, as well the individual components of the primary outcome.
Statistical analysisComparisons between groups were performed using the chi-square test, Student's t test or Mann–Whitney test, as appropriate. Univariate and multivariate analysis were performed using Cox regression to identify predictors significantly associated with the outcomes. A p-value <0.05 was taken to indicate statistical significance. The statistical analysis was performed using IBM SPSS Statistics, version 21.0 (IBM SPSS, Chicago, IL, USA).
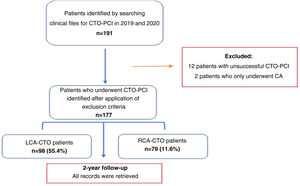
ResultsBaseline patient characteristics and medical historyA total of 191 patients were recruited, with 14 patients being excluded from the study: 12 patients had an unsuccessful procedure (six with RCA-CTO and six with LCA-CTO) and two only underwent CA (LCA-CTO) (Figure 1).
A total of 177 patients (82.5% male) were therefore included in the study, which took place in 2019 and 2020. The sample characteristics are summarized in Table 1. The two groups were composed of 98 patients (55.4%) with LCA-CTO and 79 (44.6%) with RCA-CTO, with an overall mean age of 64.5±11.4 years. Medical history was positive for hypertension in 74.6% of patients, dyslipidemia in 72.9%, obesity in 18.2% and HF in 15.3%. RCA-CTO patients were younger, with a mean age of 63.6±10.3 years (p=0.047). The most common clinical presentation was non-ST-elevation MI (32.2%), followed by stable angina (26%) and heart failure symptoms (22%), with no statistical differences between groups (p=0.072). The majority of patients were on OMT (83.1%, p=0.172) and antianginal drugs (98.3%, p=0.691), with no difference regarding the CTO vessel treated.
Baseline characteristics of patients undergoing percutaneous coronary intervention for chronic total occlusions, compared by vessel treated.
| CTO vessel treated | Total (n=177) | p | ||
|---|---|---|---|---|
| LCA-CTO (n=98, 55.4%) | RCA-CTO (n=79, 44.6%) | |||
| Gender, n (%) | ||||
| Male | 80.0 (81.2) | 66.0 (83.5) | 146 (82.5) | |
| Female | 18.0 (18.4) | 13.0 (16.5) | 31.0 (17.5) | 0.739 |
| Age, years, mean±SD | 66.9±11.6 | 63.6±10.3 | 64.5±11.4 | 0.047 |
| Hypertension, n (%) | 73.0 (74.5) | 59.0 (74.7) | 132 (74.6) | 0.977 |
| T2DM, n (%) | 38.0 (38.8) | 32.0 (40.5) | 70.0 (39.5) | 0.815 |
| Dyslipidemia, n (%) | 73.0 (74.5) | 56.0 (70.1) | 129 (72.9) | 0.592 |
| Smoking, n (%) | 23.0 (23.5) | 26.0 (32.9) | 49.0 (27.7) | 0.287 |
| Obesity, n (%) | 19.0 (28.9) | 13.0 (26.8) | 32.0 (18.2) | 0.592 |
| Heart failure history, n (%) | 14.0 (14.3) | 13.0 (16.7) | 27.0 (15.3) | 0.690 |
| Previous stroke, n (%) | 4.00 (4.08) | 4.00 (5.06) | 8.00 (4.50) | 0.755 |
| Atrial fibrillation, n (%) | 11.0 (11.2) | 21.0 (26.6) | 22.0 (12.4) | 0.588 |
| Chronic renal disease, n (%) | 10.0 (10.2) | 4.00 (5.06) | 14.0 (7.90) | 0.208 |
| Ischemic heart disease, n (%) | 52.0 (53.1) | 46.0 (58.2) | 98.0 (55.3) | 0.397 |
| Chronic lung disease, n (%) | 3.00 (3.06) | 7.00 (8.86) | 10.0 (5.60) | 0.097 |
| Clinical indication, n (%) | ||||
| ACS | 45.0 (45.9) | 47.0 (59.5) | 92.0 (52.0) | 0.072 |
| STEMI | 18.0 (18.4) | 17.0 (21.5) | 35.0 (19.8) | |
| NSTE-ACS | 27.0 (27.6) | 30.0 (38.0) | 57.0 (32.2) | |
| CCS | 53.0 (54.1) | 32.0 (40.5) | 85.0 (48.0) | 0.072 |
| Stable angina | 33.0 (33.7) | 13.0 (16.5) | 46.0 (26.0) | |
| Heart failure | 20.0 (20.4) | 19.0 (24.0) | 39.0 (22.0) | |
| CCS score, n (%) | ||||
| I and II | 74.0 (75.5) | 59.0 (74.7) | 133 (75.1) | |
| III and IV | 24.0 (24.5) | 20.0 (25.3) | 44.0 (24.9) | 0.899 |
| OMT, n (%) | 78.0 (79.6) | 69.0 (87.3) | 147 (83.1) | 0.172 |
| Antianginal | 96.0 (98.0) | 78.0 (98.7) | 174 (98.3) | 0.691 |
| Aspirin or OAC | 98.0 (100) | 79.0 (100) | 177 (100) | 0.956 |
| DAPT-DAT 6 months | 94.0 (95.9) | 76.0 (96.2) | 170 (96.0) | 0.923 |
ACS: acute coronary syndrome; CCS: Canadian Cardiovascular Society; CCS: chronic coronary syndrome; CTO: chronic total occlusion; DAPT: dual antiplatelet therapy; DAT: dual antithrombotic therapy; HF: heart failure; NSTE-ACS: non-ST-elevation acute coronary syndrome; OAC: oral anticoagulant therapy; OMT: optimal medical therapy; PCI: percutaneous coronary intervention; RCA: right coronary artery; SD: standard deviation; STEMI: ST-elevation acute coronary syndrome; T2DM: type 2 diabetes mellitus.
From a procedural point of view, RCA was the most frequent CTO artery (44.6%), followed by the left circumflex artery (29.4%). The procedures were mostly performed in a scheduled regime rather than a clinical emergent (ad-hoc) setting (32.2%, p=0.140). An anterograde approach was most commonly employed (88.7%, p=0.052), and contralateral access was preferred in RCA-CTO patients (62%, p<0.001). Multivessel disease was found in 152 (85.9%, p=0.217) patients, and complete revascularization at the time of CTO PCI was observed in 98 (55.4%), more frequently in the LCA-CTO group but without statistical significance (p=0.405). Mean SYNTAX and Multicenter CTO Registry of Japan (J-CTO) scores were 35.6±15.1 and 0.79±0.73, respectively. Ischemia or myocardial viability testing was performed in 43 (24.3%, p=0.322) patients, mainly stress echocardiography (10.7%, p=0.815). RCA-CTO patients presented with higher creatinine clearance levels (80.8±24.9 ml/min, p=0.038). There were no differences between groups with regards to radiation dose measured by air kerma (1784 mGy) or kerma area product (113 Gy cm2), contrast volume used (254±94.3 ml) or procedure time (132±56 min). The rate of periprocedural complications was 5.1%, of which vessel perforation was the most common (2.26%). Although LVEF was mildly reduced at baseline, ventricular function improved in both groups after intervention in a mean follow-up of 18 months (p<0.001) (Table 2).
Angiographic characteristics of chronic total occlusion patients undergoing percutaneous coronary intervention, compared by vessel treated.
| CTO vessel treated | Total (n=177) | p | ||
|---|---|---|---|---|
| LCA-CTO (n=98, 55.4%) | RCA-CTO (n=79, 44.6%) | |||
| Contralateral access, n (%) | 27.0 (27.6) | 49.0 (62.0) | 76.0 (42.9) | <0.001 |
| CTO vessel, n (%) | ||||
| LCA | 98.0 (100) | 0.00 (0.00) | 98.0 (55.4) | |
| LAD | 46.0 (46.9) | 0.00 (0.00) | 46.0 (26.0) | |
| LCx | 52.0 (53.1) | 0.00 (0.00) | 52.0 (29.4) | |
| RCA | 0.00 (0.00) | 79.0 (100) | 79.0 (44.6) | <0.001 |
| Multivessel disease, n (%) | 87.0 (88.8) | 65.0 (82.3) | 152 (85.9) | 0.217 |
| Complete revascularization, n (%) | 57.0 (58.2) | 41.0 (51.9) | 98.0 (55.4) | 0.405 |
| J-CTO score, mean±SD | 0.70±0.68 | 0.89±0.78 | 0.79±0.73 | 0.099 |
| Syntax score, mean±SD | 36.0±13.7 | 34.9±16.7 | 35.6±15.1 | 0.649 |
| Ischemia/viability study, n (%) | 21.0 (21.4) | 22.0 (27.8) | 43.0 (24.3) | 0.322 |
| Stress echocardiogram, n (%) | 11.0 (11.2) | 8.00 (10.1) | 19.0 (10.7) | 0.815 |
| SPECT-MPI, n (%) | 3.00 (3.10) | 3.00 (3.80) | 6.00 (3.40) | 0.788 |
| Cardiac MRI, n (%) | 7.00 (7.10) | 11.0 (13.9) | 18.0 (10.2) | 0.138 |
| Ad-hoc procedure, n (%) | 27.0 (27.6) | 30.0 (38.0) | 57.0 (32.2) | 0.140 |
| Approach, n (%) | ||||
| Antegrade | 91.0 (92.9) | 66.0 (83.5) | 157 (88.7) | |
| Retrograde | 7.00 (7.14) | 13.0 (16.5) | 20.0 (11.3) | 0.052 |
| Radiation dose | ||||
| Air kerma, mGy, median (IQR) | 1808 (1982) | 2228 (1734) | 2043 (1784) | 0.561 |
| Kerma area product, Gy cm2, median (IQR) | 109 (120) | 130 (105) | 120 (113) | 0.363 |
| LVEF at baseline, %, mean±SD | 48.2±9.08 | 45.4±10.8 | 47.1±10.5 | 0.066 |
| LVEF after PCI, %, mean±SD | 51.3±8.91 | 51.1±10.4 | 51.2±9.73 | 0.928 |
| p<0.001 | p<0.001 | |||
| Creatinine clearance, ml/min, mean±SD | 72.3±27.2 | 80.8±24.9 | 77.1±26.6 | 0.038 |
| PCI time, min, mean±SD | 268±3.00 | 141±59.8 | 132±56.0 | 0.153 |
| Contrast volume, ml, mean±SD | 269±90.9 | 241±86.3 | 254±94.3 | 0.520 |
| Periprocedural complications, n (%) | ||||
| Total, n (%) | 4.00 (4.08) | 5.00 (6.33) | 9.00 (5.10) | |
| Dissection | 1.00 (1.02) | 2.00 (2.53) | 3.00 (1.69) | |
| Perfuration | 2.00 (2.04) | 2.00 (2.53) | 4.00 (2.26) | |
| Pericardial effusion | 1.00 (1.02) | 0.00 (0.00) | 1.00 (0.56) | |
| Stroke/MI | 0.00 (0.00) | 1.00 (1.26) | 1.00 (0.56) | 0.522 |
Ad-hoc: unplanned procedure; CTO: chronic total occlusion; IQR: interquartile range; J-CTO: Multicenter CTO Registry of Japan; LAD: left anterior descending artery; LCA: left coronary artery; LCx: left circumflex artery; LVEF: left ventricular ejection fraction; MI: myocardial infarction; MRI: magnetic resonance imaging; PCI: percutaneous coronary intervention; RCA: right coronary artery; SD: standard deviation; SPECT-MPI: single-photon emission computed tomography myocardial perfusion imaging.
The primary outcome occurred in 28 (16.6%) patients and was significantly more frequent in RCA-CTO patients (19, 24.7%, p=0.010) in two-year follow-up (mean follow-up of 18 months). This was mainly driven by recurrence of HF symptoms (12, 15.6%, p=0.013) (Table 3).
Primary and secondary outcomes in two-year follow-up, compared by chronic total occlusion vessel treated.
| CTO vessel treated | Total (n=177) | p | ||
|---|---|---|---|---|
| LCA-CTO (n=98, 55.4%) | RCA-CTO (n=79, 44.6%) | |||
| Primary outcome, n (%) | 9.00 (9.80) | 19.0 (24.7) | 28.0 (16.6) | 0.010 |
| Total | ||||
| Individual components, n (%) | ||||
| Angina | 7.00 (7.60) | 9.00 (11.7) | 16.0 (9.50) | 0.367 |
| HF symptoms, n (%) | 4.00 (4.30) | 12.0 (15.6) | 16.0 (9.50) | 0.013 |
| Secondary outcomes, n (%) | ||||
| MI | 2.00 (2.20) | 1.00 (1.30) | 3.00 (1.80) | 0.668 |
| All-cause mortality | 4.00 (4.30) | 2.00 (2.60) | 6.00 (3.60) | 0.540 |
CTO: chronic total occlusion; HF: heart failure; LCA: left coronary artery; MI: myocardial infarction; RCA: right coronary artery.
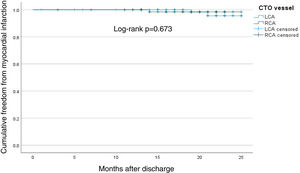
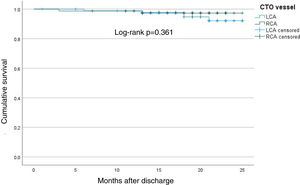
Rates of MI and all-cause mortality were similar between groups (RCA-CTO 1.3%, p=0.361 and 2.6%, p=0.673, respectively, on survival analysis) (Figures 2 and 3).
Kaplan–Meier curve showing time until myocardial infarction (mean follow-up of 18 months) in chronic total occlusion patients undergoing percutaneous coronary intervention, compared by vessel treated. CTO: chronic total occlusion; LCA: left coronary artery; PCI: percutaneous coronary intervention; RCA: right coronary artery.
Kaplan–Meier curve showing time until death (mean follow-up of 18 months) in chronic total occlusion patients undergoing percutaneous coronary intervention, compared by vessel treated. CTO: chronic total occlusion; LCA: left coronary artery; PCI: percutaneous coronary intervention; RCA: right coronary artery.
Revascularized RCA-CTO showed an association with and was an independent predictor of the primary outcome (p=0.016, hazard ratio [HR] 2.77, 95% confidence interval [CI] 1.21–6.32), although LVEF was not (p=0.482, HR 0.99, 95% CI 0.95–1.02). Multivessel disease was associated with the primary outcome but was not an independent predictor in multivariate analysis (p=0.968, HR 3.72, 95% CI 0.42–6.32). Complete revascularization was not associated with the primary outcome in univariate or multivariate analysis (Table 4).
Univariate and multivariate analysis (Cox regression) for the primary outcome.
| UnivariateHR (95% CI) | p | MultivariateHR (95% CI) | p | |
|---|---|---|---|---|
| Age | 1.01 (0.97–1.04) | 0.803 | 1.01 (0.97–1.04) | 0.711 |
| Gender | 1.42 (0.45–4.43) | 0.544 | 1.39 (0.45–4.34) | 0.565 |
| Multivessel disease | 1.24 (1.14–1.34) | 0.016 | 3.72 (0.42–6.32) | 0.968 |
| Complete revascularization | 0.78 (0.34–1.76) | 0.558 | 1.33 (0.62–2.87) | 0.464 |
| CTO vessel (RCA) | 3.02 (1.27–7.14) | 0.010 | 2.77 (1.21–6.32) | 0.016 |
| LVEF | 0.98 (0.95–1.02) | 0.366 | 0.99 (0.95–1.02) | 0.482 |
CI: confidence interval; CTO: chronic total occlusion; HR: hazard ratio; LVEF: left ventricular ejection fraction; RCA: right coronary artery.
For multivariate analysis all variables listed were included in the model.
LVEF was found to be an independent predictor of all-cause mortality (p=0.023, HR 0.92, 95% CI 0.85–0.98), although recanalized RCA-CTO was not (p=0.291, HR 0.40, 95% CI 0.07–2.17).
DiscussionThe present analysis showed that revascularization of CTO lesions by PCI was associated with low rates of symptom recurrence. In addition, treatment of RCA-CTO lesions was less beneficial in alleviating recurrence of HF symptoms compared to LCA-CTO. In terms of clinical outcomes, the benefit was independent of which CTO vessel was treated.
Baseline sample characteristics were similar to those of recently published European RCTs and international registries, i.e. almost three quarters of patients had a medical history of hypertension and dyslipidemia and 40% had been diagnosed with diabetes. The mean LVEF observed in our study was mildly reduced, in contrast to preserved ventricular function in those studies.2,5,15
From a procedural point of view, contrast volume and patient radiation doses were similar to those reported in the above trials, but the current study reported a longer procedure duration.
CTO affecting the RCA was the most prevalent and an anterograde approach was most commonly used, as in the above studies.2,4,5,16 The rate of periprocedural complications was lower than that reported in the literature.5,13,15
To the best of our knowledge, the IMPACTOR trial was the only RCT powered to investigate the impact of PCI of RCA-CTO (isolated CTO) on inducible ischemia burden, functional status and quality of life. The trial showed benefits in all three variables.13 In the present study, after a mean follow-up of 18 months, RCA-CTO patients presented with more symptom recurrence, mainly driven by HF symptoms, than LCA-CTO patients. Although the rate of symptom recurrence (16.6%) was low in the overall sample (most patients were on OMT, which probably contributed to this low rate), RCA-CTO was an independent predictor of recurrence. This was probably related to three factors. First is the high burden of multivessel disease (86%) and CAD complexity (mean SYNTAX score 35.6±15.1) in the present study, associated with a lower rate of complete revascularization in the RCA-CTO group (51.9%), although this was not statistically significant. The DECISION-CTO4 and EUROCTO2 trials reported high rates of multivessel disease and differing results in their quality-of-life outcomes. While the former showed no difference, the latter suggested that CTO PCI was more favorable compared to OMT. This difference may be due to the fact that randomization was performed before non-CTO PCI in DECISION-CTO. Second, the presence of a greater number of patients with HF and diabetes in the RCA-CTO group associated with HF clinical presentation may have contributed to recurrence of HF symptoms. Third, the smaller territory of myocardial mass supplied by the RCA, compared to the LCA, may also impact on the recurrence of symptoms, although LVEF was not an independent predictor of symptom recurrence.
LVEF was, instead, an independent predictor for all-cause mortality, which has been reported in observational studies of diabetic patients.17,18 Similarly, patients with LVEF ≤55% were found to have higher rates of improvement in symptoms.19 In this study, improvement in LVEF (from mildly reduced to preserved) was also observed, regardless of the artery treated.
To date, only the IMPACTOR trial has reported that successful RCA-CTO PCI was beneficial in patient functional status and quality of life, compared to OMT.13 The present study shows that symptom recurrence was low regardless of which CTO artery was treated, even though it is suggested that the benefit in HF symptom recurrence was less evident in RCA-CTO patients. Further and larger studies are needed to address this issue.
LimitationsSome limitations should be acknowledged. This was an observational study, and so the data collected are limited to medical records. Patient symptoms were not assessed by scales or questionnaires, which could thus increase ambiguity. Our study included only successful CTO PCI; failed CTO PCI was not addressed, which may limit the validity of the conclusions. Finally, the data in our study are from only one CTO PCI center, so our conclusions may not be generalizable to other cardiac centers.
ConclusionsRevascularization of CTO lesions by PCI was associated with low rates of symptom recurrence, and clinical outcomes showed no differences with regard to the CTO artery treated. However, recanalization of RCA-CTO was less beneficial in alleviating the recurrence of HF symptoms.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to express their gratitude to all colleagues who cooperated in providing data for the current analysis.