The aim of this study was to assess prevalence, clinical characteristics, and prognosis in elderly patients with heart failure with preserved ejection fraction (HFPEF) compared to patients with heart failure with reduced ejection fraction (HFREF) who were followed in an internal medicine unit.
MethodsIn this retrospective observational study, the sample consisted of 301 patients followed in an internal medicine referral unit between January 2007 and December 2010. All patients were checked to determine their vital status on 31 December 2012. Survival was analyzed using Kaplan-Meier curves, and compared using the log-rank test.
ResultsOf the 301 patients, 165 (54.8%) were women. In the 263 cases (87.4%) who underwent echocardiographic assessment, 190 (72.2%) had HFPEF and 73 (27.8%) had HFREF. Mean age was similar in the two groups (80.1 and 79.9 years; p=0.905), with a predominance of women in the HFPEF group (60.5% women, 42.5% men; p=0.025). The main etiology was hypertensive heart disease in the HFPEF group. Regarding treatment, more beta-blockers were administered in the HFREF group. No statistically significant differences were observed between the groups in terms of cardiovascular risk factors, comorbidities, NYHA functional class, or mortality.
ConclusionClinical characteristics were similar for both HFPEF and HFREF patients. Women were predominant in the HFPEF group, as was hypertensive etiology. No significant differences in mortality were observed between the groups.
O objetivo do estudo é analisar a prevalência, as características clínicas e o prognóstico dum grupo de doentes idosos com diagnóstico de insuficiência cardíaca com fração de ejeção preservada (IC/FEP) seguidos numa consulta especializada e compará-los com os doentes que apresentam fração de ejeção dimuída (IC/FED).
Materiais e métodosEstudo retrospetivo observacional incluindo 301 doentes, seguidos numa consulta especializada de Medicina Interna, no período entre janeiro de 2007 e dezembro de 2010 cujo status vital foi determinado a 31 de dezembro de 2012. Para a análise de sobrevivência foram utilizadas as curvas de Kaplan-Meier e na comparação foi utilizado o teste de Log-rank.
Resultados301 doentes foram estudados, sendo 165 (54,8%) do sexo feminino. Nos 263 (87,4%) casos nos quais foi realizado o estudo ecocardiográfico, 190 (72,2%) correspondiam a doentes com diagnóstico de IC/FEP e 73 (27,8%) de IC/FED. A idade média foi similar nos dois grupos (80,3 e 79,9 anos, p 0,905), sendo maior a percentagem de mulheres (60,5% face a 42,5%, p 0,025) e com predomínio de etiologia hipertensiva no grupo com IC/FEP. Quanto ao tratamento, o uso de betabloqueantes foi maior no grupo com IC/FED. Não foram encontradas diferenças significativas entre ambos os grupos relativamente a fatores de risco cardiovascular, comorbilidades, classe funcional ou mortalidade.
ConclusãoAs caraterísticas clínicas dos doentes com IC/FEP e com IC/FED são similares. No grupo de IC/FEP predominam os doentes do sexo feminino e a etiologia hipertensiva. Não foram observadas diferenças na mortalidade entre ambos os grupos.
Heart failure (HF) continues to be a major burden on public health systems, with high morbidity and mortality and spiraling costs, which account for 1–2% of the annual health budget of most developed nations.1 In Spain, it is the third leading cause of death from cardiovascular disease; ischemic heart disease and cerebrovascular disease are the leading causes, with estimated mortality of 4.2% and 4.4% for the years 2010 and 2011, respectively. Moreover, HF is the primary cause of hospitalization in patients aged 65 or over, accounting for 2–2.5% of the total number of annual hospital admissions.2 Furthermore, the readmission rate following a first hospitalization for HF is high, increasing from 38% in the first month3 to 43% at 6–12 months.4
The prevalence of HF is on the rise due not only to the improved prognosis of patients with ischemic heart disease (IHD) or hypertension, but also to the progressive aging of the population. The census for the Spanish population for the last two decades showed an increase of nearly 50% in life expectancy of 1–2 years in the population aged from 77 to 87 years.2 Moreover, the prevalence of HF is estimated at 6.8% in people aged 45 years or older, and 16.1% in people older than 75,5 and it is precisely in the latter population that the incidence and prevalence of heart failure with preserved ejection fraction (HFPEF) rises.6
Though the survival of HF patients has improved in recent years, prognosis continues to be poor, with 50% mortality five years after diagnosis.7 Most clinical trials are on patients with heart failure with reduced ejection fraction (HFREF), and it is in this population that current therapies have shown to improve life expectancy.8 In contrast, the findings on HFPEF remain inconclusive, which underscores the need for further studies on these patients, who are the most prevalent among elderly populations, as most internal medicine departments can attest.9
Few studies have compared the clinical characteristics of elderly patients with HFREF in comparison to those with HFPEF. The aim of this study was to assess prevalence, clinical characteristics, and medium-term prognosis of a group of elderly HFPEF patients in comparison to elderly HFREF patients who were followed in an internal medicine unit.
MethodsThis was a retrospective observational study of a cohort of 301 patients who were followed in an internal medicine unit HF unit in a tertiary referral hospital in north-eastern Spain with an estimated catchment population of 400 000.10 Patients were consecutively included for study between January 1, 2007 and December 31, 2010, and their vital status was checked to determine whether they were alive on December 31, 2012. Patients were referred from primary health care, emergency departments, and cardiology and internal medicine wards.
Only patients aged 18 years or older were included in the study. HF was diagnosed according to the clinical practice guidelines of the European Cardiology Society11 and the American College of Cardiology/American Heart Association,12 based on the presence of HF symptoms and signs.
At the time of inclusion and during follow-up, data were collected on sociodemographic, clinical, laboratory, electrocardiographic, and echocardiographic variables, New York Heart Association (NYHA) functional class, and treatment.
Left ventricular ejection fraction (LVEF) was measured using the Teichholz formula and the subjective scoring of the echocardiographer. Patients were assigned to one of two groups: preserved ejection fraction with LVEF ≥50%, or reduced ejection fraction with LVEF <50%.
Hypertension was defined as blood pressure >140/90 mmHg or less if under directed treatment, anemia as hemoglobin <12 g/dl for women and <13 g/dl for men,13 and chronic renal disease as a glomerular filtration rate <60 ml/min/m2 using the 4-variable Modification of Diet in Renal Disease formula.
The etiology of HF was determined on the basis of the following criteria: ischemic, when the patient was diagnosed with IHD; valvular, when there was moderate valvulopathy with no IHD; hypertensive, when there was known hypertension but no evidence of other significant heart disease; dilated cardiomyopathy, as defined by LVEF <50% with no other known cardiac cause (including heavy drinking, idiopathic etiology, etc.); cor pulmonale, right heart failure without left ventricular dysfunction.
Statistical analysisQualitative variables were expressed as absolute frequencies and percentages and quantitative variables were expressed as mean ± standard deviation. The statistical analysis was performed using SPSS for Windows, version 15. Descriptive statistical analysis was based on frequency tables of categorical variables using the chi-square test to compare the significance of association between qualitative variables. The Student's t test for independent samples was used to compare quantitative variables. A value of p<0.05 (two-sided) was used as the nominal level of statistical significance. Survival curves between the HFREF and HFPEF patient groups were constructed using the Kaplan-Meier method and compared using the log-rank test.
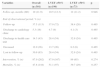
ResultsA total of 301 patients were assessed, of whom 165 (54.8%) were women. For various reasons (including non-compliance with follow-up and unfavorable clinical conditions), LVEF was not assessed echocardiographically in 38 patients (12.7%). Of the 263 (87.4%) patients in whom LVEF was assessed echocardiographically, 190 (72.2%) had HFPEF and 73 (27.8%) had HFREF. The characteristics of the two groups are shown in Table 1.
Clinical characteristics of patients according to left ventricular ejection fraction.
| Overall (n=301) | LVEF ≥50% (n=190) | LVEF <50% (n=73) | p | |
|---|---|---|---|---|
| Women, % (n) | 54.8 (165) | 60.5 (115) | 42.5 (31) | 0.025 |
| Age, years (P25;75) | 80.3 (75.2;84.3) | 80.1 (74.6;84.3) | 79.9 (74.0;84.2) | 0.905 |
| COPD, % (n) | 30.2 (91) | 31.6 (60) | 28.8 (21) | 0.773 |
| Diabetes, % (n) | 32.2 (97) | 33.2 (63) | 30.1 (22) | 0.892 |
| Hypertension, % (n) | 81.4 (245) | 84.2 (160) | 76.7 (56) | 0.259 |
| Anemia, % (n) | 46.8 (141) | 45.3 (85) | 47.9 (35) | 0.692 |
| Renal failure, % (n) | 58.8 (177) | 57.4 (109) | 58.9 (43) | 0.629 |
| NYHA class, % (n) | ||||
| I | 27.8 (83) | 26.5 (50) | 30.1 (22) | 0.792 |
| II | 42.5 (127) | 41.8 (79) | 46.6 (34) | 0.792 |
| III | 29.1 (87) | 30.7 (58) | 23.3 (17) | 0.792 |
| IV | 0.7 (2) | 1.1 (2) | 0.0 | 0.792 |
| Atrial fibrillation, % (n) | 55.1 (66) | 55.8 (106) | 56.2 (41) | 0.791 |
| Etiology, % (n) | ||||
| Hypertensive | 67.8 (198) | 70.5 (129) | 57.5 (42) | 0.003 |
| Ischemic | 12.0 (35) | 10.4 (19) | 17.8 (13) | 0.003 |
| Valvular | 8.6 (25) | 9.8 (18) | 5.5 (4) | 0.003 |
| DCM | 4.5 (13) | 1.1 (2) | 12.3 (9) | 0.003 |
| Cor pulmonale | 5.1 (15) | 7.1 (13) | 2.7 (2) | 0.003 |
| Other | 2.1 (6) | 1.1 (2) | 4.1 (3) | 0.003 |
COPD: chronic obstructive pulmonary disease; DCM: dilated cardiomyopathy; LVEF: left ventricular ejection fraction; NYHA: New York Heart Association.
Patients’ mean age was similar in the two groups (80.1 and 79.9 years; p=0.905), with a predominance of women in the HFPEF group (60.5% women, 42.5% men). Analysis of cardiovascular risk factors such as hypertension and diabetes, other comorbidities including chronic obstructive pulmonary disease, anemia, atrial fibrillation, and chronic renal disease, and NYHA functional class revealed no statistically significant differences.
Regarding etiology, hypertensive heart disease was the main cause in the HFPEF group, whereas IHD and dilated cardiomyopathy were the main causes in the HFREF group.
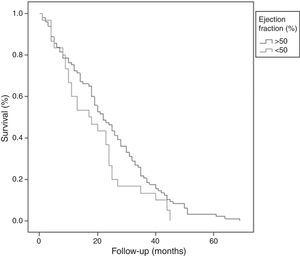
Data on patient referral source, pharmacological treatment for LVEF, and follow-up are shown in Tables 2–4, respectively.Most referrals from internal medicine wards had HFPEF, whereas most referrals from cardiology wards had HFREF (Table 2). Comparison of treatments during follow-up showed no significant differences in the use of angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and aldosterone antagonists (AA). HFREF patients were prescribed more beta-blockers than HFPEF patients (Table 3). The mean follow-up was 10 months. No statistically significant differences in survival rates, follow-up or causes of ending of the observation period were found between the groups according to LVEF (Figure 1).
Source of patient referrals.
| Overall (n=301) | LVEF ≥50% (n=190) | LVEF <50% (n=73) | p | |
|---|---|---|---|---|
| Source of referral % (n) | ||||
| Primary care | 1.0 (3) | 0.5 (1) | 2.8 (2) | 0.032 |
| Emergency | 22.7 (68) | 19.6 (37) | 23.6 (17) | 0.032 |
| Cardiology | 3.3 (10) | 3.2 (6) | 5.6 (4) | 0.032 |
| Internal medicine | 68.9 (206) | 73 (138) | 66.7 (48) | 0.032 |
| Other | 4.0 (12) | 3.7 (7) | 1.4 (1) | 0.032 |
LVEF: left ventricular ejection fraction.
Pharmacological treatment according to left ventricular ejection fraction.
| Overall (n=301) | LVEF ≥50% (n=190) | LVEF <50% (n=73) | p | |
|---|---|---|---|---|
| Treatment, % (n) | ||||
| ACE inhibitors | 32.1 (84) | 32.9 (55) | 29.2 (19) | 0.910 |
| ARBs | 46.6 (122) | 46.1 (77) | 50.8 (27) | 0.256 |
| Spironolactone | 24.8 (65) | 22.8 (38) | 32.3 (21) | 0.570 |
| Beta-blockers | 53.5 (139) | 48.2 (80) | 67.2 (43) | 0.028 |
ACE: angiotensin-converting enzyme; ARBs: angiotensin receptor blockers.
Follow-up and mortality.
| Variables | Overall (n=301) | LVEF ≥50% (n=190) | LVEF <50% (n=73) | p |
|---|---|---|---|---|
| Follow-up, months (SD) | 10 (11.9) | 10.5 (12.3) | 12 (11.2) | 0.946 |
| End of observational period, % (n) | ||||
| Follow-up | 37.5 (113) | 37.9 (72) | 38.4 (28) | 0.465 |
| Discharge to cardiology clinic | 5.3 (16) | 4.7 (9) | 4.1 (3) | 0.465 |
| Discharge to health care unit | 14.3 (43) | 28.4 (54) | 32.9 (24) | 0.465 |
| Deceased | 12.0 (36) | 13.7 (26) | 8.2 (6) | 0.465 |
| Lost to follow-up | 30.9 (93) | 28.4 (54) | 32.9 (24) | 0.465 |
| Intervention, % (n) | 87.0 (262) | 87.9 (167) | 89 (65) | 0.274 |
| Mortality, % (n) | 47.8 (144) | 51.1 (97) | 39.7 (29) | 0.257 |
LVEF: left ventricular ejection fraction.
This study confirmed that HFPEF is more frequent in elderly patients. In our series 72.2% of HFPEF patients had a mean age >80 years. In other studies, its frequency varies considerably, with 51.8% of cases at a mean age of 72.4 years,9 and 40% at a mean age of 66 years.14 These differences are in all likelihood due to differences in age, as the patients in this study were older than in most series in the recent literature, which would account for the lower percentages of patients with preserved LVEF.14–20 In contrast, other studies including very elderly patients report mean ages similar to those observed in our study, e.g. mean age 80±10 years21 or close to 79 years.22 However, two other Spanish studies, GALICAP17 and INCA,18 which included younger patients than in our study (mean age 76 and 71 years, respectively), found a prevalence of HFPEF similar to that observed in this study: 61.4 and 61.7%, respectively. Likewise, similar results have been obtained in studies undertaken in other countries, such as a prospective study in France, where 61% of the population aged over 80 years had preserved LVEF, falling to 53% below this age group,23 which is similar to the findings of the present study. In contrast, in a Japanese registry of younger patients (mean age 71 years) hospitalized due to HF, only 26% had LVEF >50%,24 a similar prevalence to that recorded in another Japanese registry during the years 2000–2004.25
Though 12.7% of patients were not echocardiographically assessed in our study, this percentage was lower than in other series, even when patients managed by cardiologists were included in the series.26,27 However, other studies have demonstrated that the number of patients without an echocardiogram is relevant in the elderly and in women, since these subgroups present the highest frequency of HFPEF, which suggests that in all probability the true prevalence is underestimated.
As for gender, in this series women predominated in the HFPEF group (60.5% vs. 42.5% men), which is in accordance with most previous studies on these patients.9,28 With respect to etiology, a significant difference was observed between the groups: hypertensive heart disease was the most frequent etiology in the HFPEF group, whereas IHD was the most frequent etiology in the HFREF group, and it is widely acknowledged that the two types of HF differ in their epidemiological characteristics. Thus, HFPEF patients tend to be older and predominantly women, and the main etiology is hypertensive, with less heart disease and atrial fibrillation as concomitant pathologies.28,29 Analysis of NYHA functional class showed no significant differences in cardiovascular risk factors or other comorbidities between the groups.
In terms of drug treatment, 32% of patients received ACE inhibitors, 47% ARBs (ACE inhibitors and ARBs 79%), 25% AA, and 54% beta-blockers (BBs). According to other studies, these drug groups can be considered an optimum complement to HF treatment, since they increase survival in HF patients with reduced LVEF. Thus, in an observational retrospective study on compliance with treatment guidelines in elderly Korean HF patients (mean age 76 years, of whom 64% were older than 75 years) by Kim et al.,30 32% were treated with BBs, 55% with ACE inhibitors or ARBs, and 7% with AA. The type and proportion of drugs administered in our population was similar to other studies.9,15,31
Few studies have assessed the different drug treatments for the two types of HF. As expected, in this study BBs were employed more in HFREF patients, but no significant differences were found between the groups in other treatments. By contrast, a study on 12 000 patients found ACE inhibitors and BBs were employed more in the HFPEF group.9
Despite the lack of evidence for the use of AA in HFPEF, these drugs were prescribed in a high percentage of our patients (22.8%) compared with other studies30 in order to control congestive symptoms.
Though a wide spectrum of drug groups (ACE inhibitors, ARBs, BBs, and AA) are known to reduce morbidity and mortality in HFREF patients, findings on the benefits of certain HFPEF drug treatments remain inconclusive, which would explain the lack of specific treatment guidelines for these patients.32–34With regard to prognosis, there is disagreement in recent reviews in the literature as to whether the prognosis of HFPEF patients is similar, worse or better than in HFREF patients.35–37 Few studies have compared prognosis in the two groups, and fewer still in HFPEF, and the results have been contradictory. While the prognosis of HFPEF patients appears to be better than in HFREF patients,29,38,39 an observational study on 478 HF patients with atrial fibrillation showed similar mortality for both HFPEF and HFREF (50% vs. 48%, p=0.74) at five years.40 Likewise, other studies have reported similar prognosis in the two groups,41,42 as was the case in our series, in which no significant differences were found.
In terms of mortality, it is generally believed that prognosis for HFREF is worse than for HFPEF, independently of other factors such as female gender, age, atrial fibrillation, chronic renal disease, functional class (NYHA III or IV), and pulmonary hypertension.35,43 In the present series, no significant differences were found in terms of prognosis, but mortality was slightly higher in HFPEF patients, which may be due to other factors such as those mentioned above. Moreover, no significant differences were found between the groups in chronic renal disease, functional class, or age. Given that no differences in mortality between the groups were observed, i.e., the factors under assessment were evenly distributed in both groups, it would be plausible to expect mortality also to be similar.
In order to improve prognosis, an integrated approach to elderly HF patients is recommended, ideally in specialized units with multidisciplinary teams, as is the case of our specialized HF unit, in which the characteristics of patients are different from those treated by cardiologists (younger and predominantly with HFREF).
In our catchment area, a heart failure protocol was recently designed,44 with the consensus of different specialists (internists and cardiologists), primary health care, emergency departments, and nursing. The protocol defines the roles of and interaction between the different health care professionals involved in treating and managing HF patients, as well as highlighting the importance of educating patients, health staff, and carers as to treatment compliance and of close and continued follow-up in accordance with the clinical practice guidelines, in order to improve the prognosis and quality of life of these patients.
LimitationsOne of the limitations of this study is that all of the patients included in the sample were followed by the internal medicine department, and patients followed by cardiologists were excluded. This may have led to bias in the selection process, given that these patients were older and had less coronary disease. Nevertheless, it results in greater homogeneity in clinical management and treatment in internal medicine departments and in primary health care, both of which are traditionally involved in the management of elderly patients with more comorbidities.
The follow-up period was quite short (10 months) due to the age of our patients; almost half of our sample (42%) died or dropped out during this period. Nevertheless, we would point out that the follow-up was probably sufficiently long, given the characteristics of our cohort.
A further limitation is the exclusion of the nearly 13% of patients who were not echocardiographically assessed.
ConclusionIn this study, most patients presented HFPEF. The clinical characteristics of this group were similar to those of the HFREF group. As in other studies, women and hypertensive etiology were predominant in the HFPEF group. HFREF patients were more likely to receive BBs, and dilated cardiomyopathy predominated. No significant differences in mortality were observed between the groups. Our experience shows that an integrated multidisciplinary approach enhances the treatment, management, and follow-up of HF patients. However, few studies have focused on HFPEF patients, and even fewer have included patients from internists in specialized HF units, which underscores the need for further prospective studies to explore new improved therapeutic strategies.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.