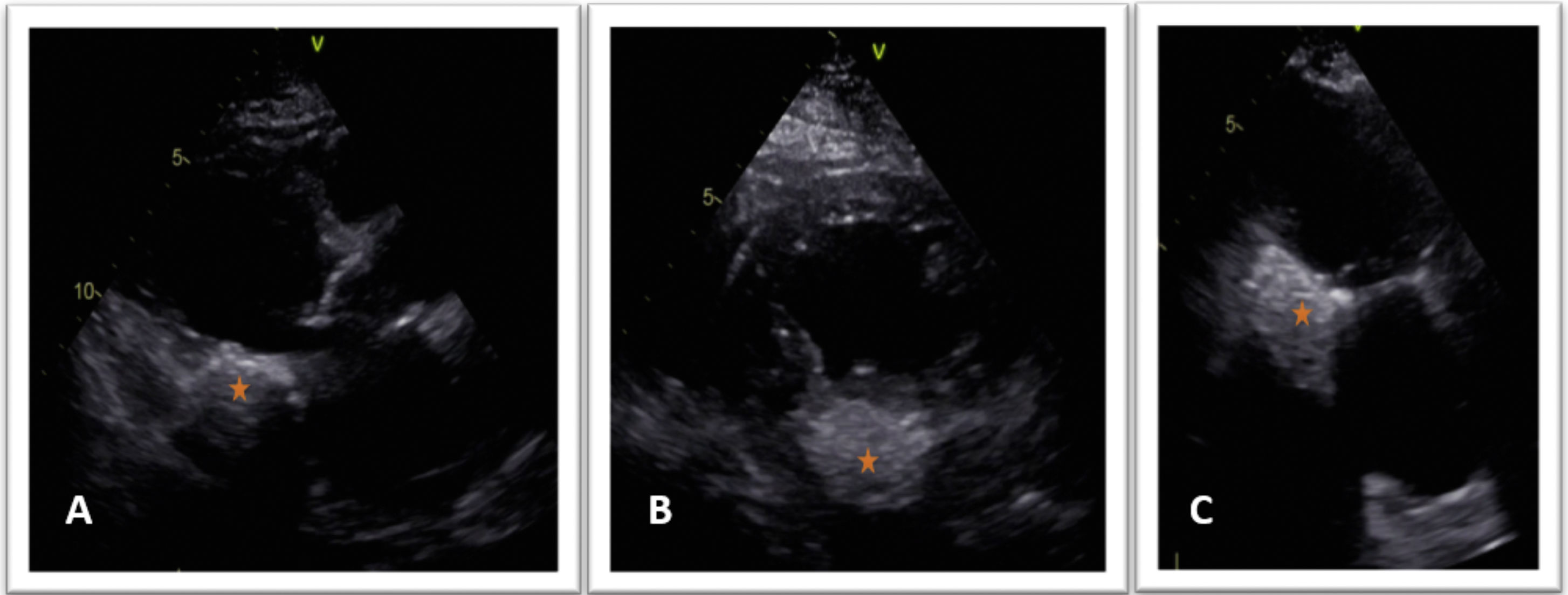
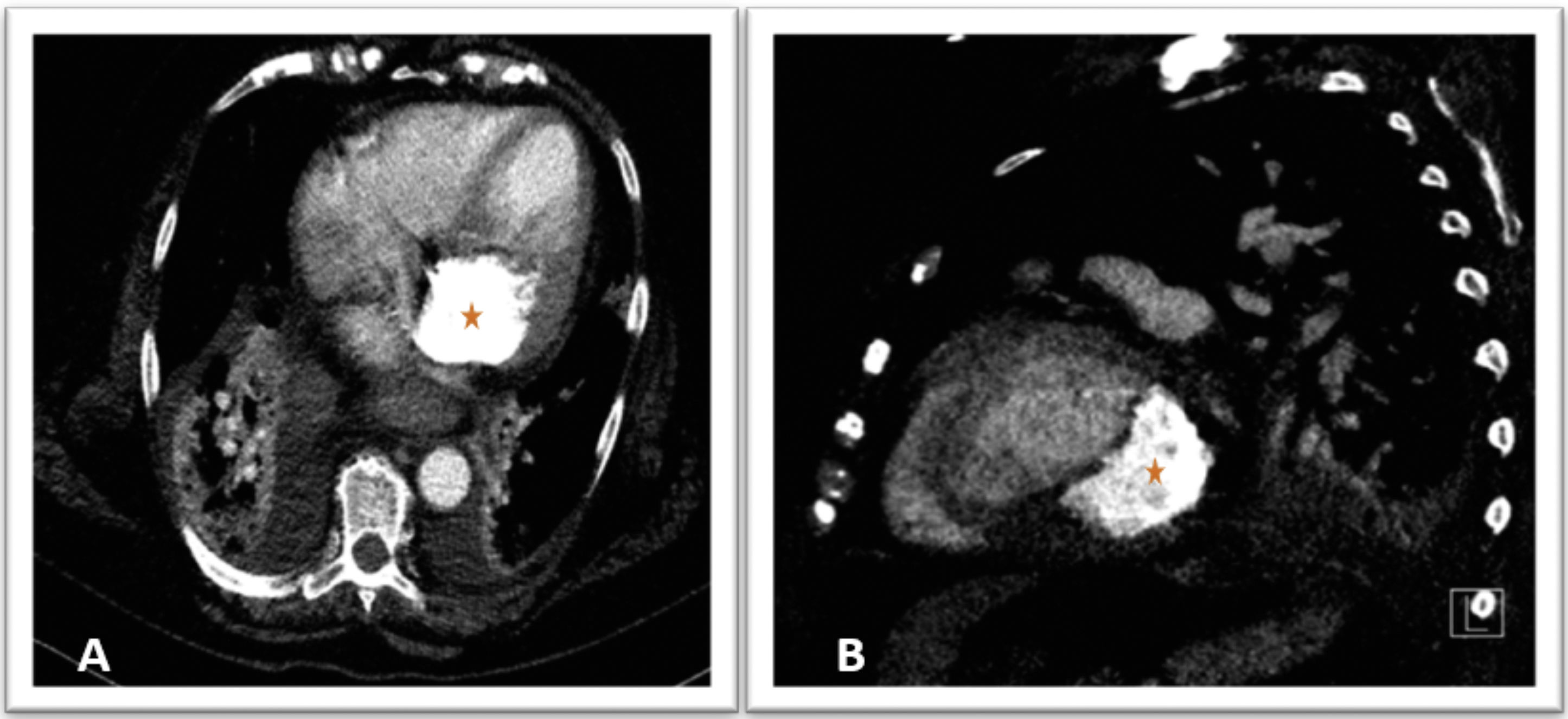
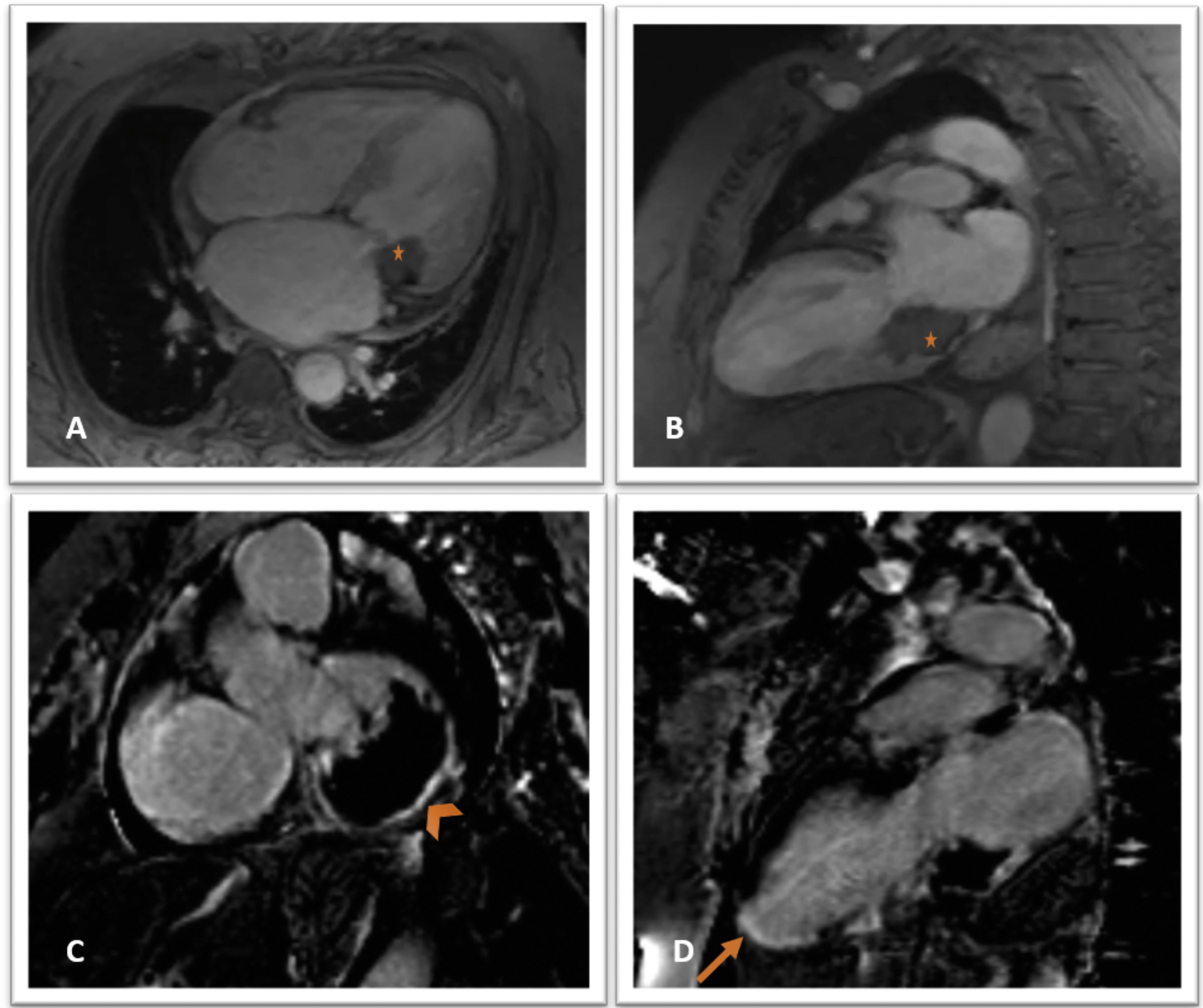
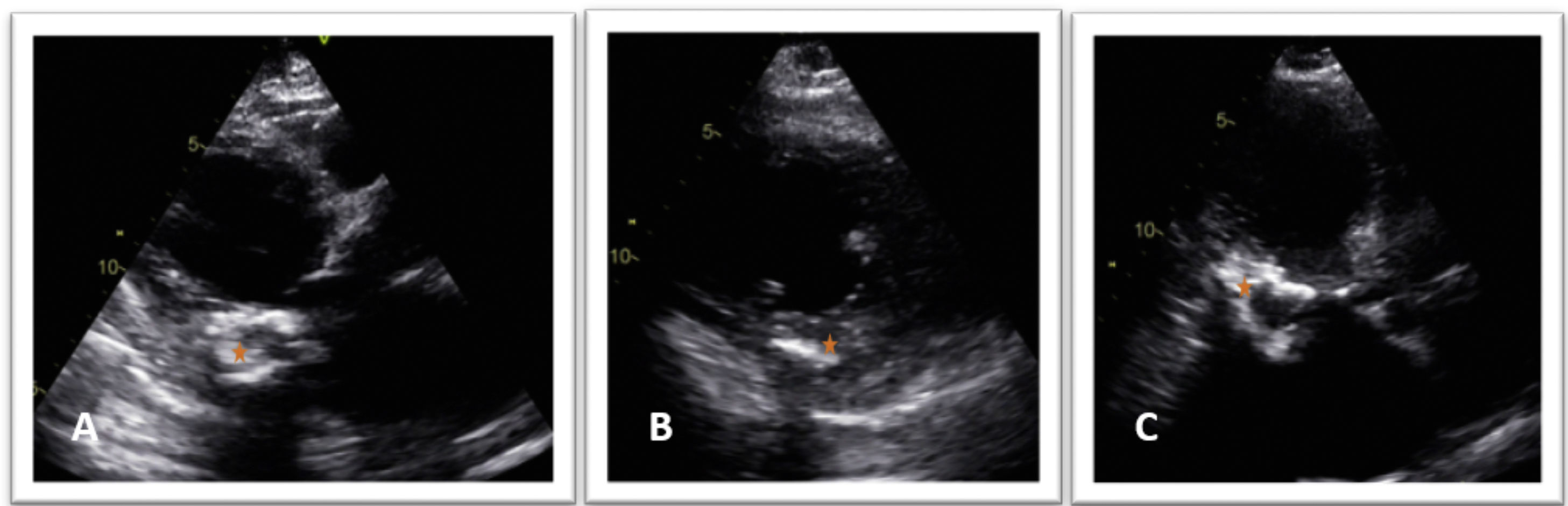
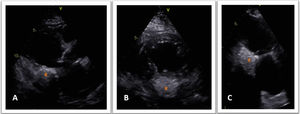
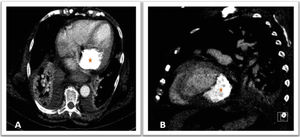
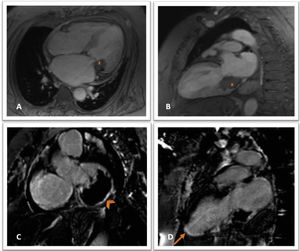
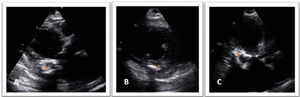
A 72-year-old hypertensive woman was investigated after a cardiac arrest in ventricular fibrillation. The electrocardiogram showed atrial fibrillation and ST-segment elevation in DII, DIII, aVF and V5-6, and emergent cardiac catheterization revealed no significant coronary artery disease. Peak high-sensitivity troponin was 47 676 ng/l. The transthoracic echocardiogram (TTE) identified an oval-shaped, calcified and homogeneously hyperechogenic mass involving the mitral annulus and posterior leaflet, without significant valvular obstruction, and infiltrating the basal segments of the inferior, posterior and lateral walls (Figure 1); severe mitral regurgitation; and a non-dilated left ventricle with normal ejection fraction. Cardiac computed tomography (CT) confirmed the calcific nature of the mass (Figure 2). Further characterization with magnetic resonance imaging (MRI) (Figure 3) demonstrated a mass-like lesion measuring 50 mm×35 mm×45 mm, hypointense in T2-weighted and gradient echo sequences, with peripheral enhancement in postcontrast delayed series, compatible with caseous calcification. Transmural delayed enhancement was also noted in the apex and inferior mid-apical segments compatible with an embolic infarction. Given the features of the mass, it was considered unresectable and a conservative approach was adopted. One month later, at the follow-up visit, TTE revealed hypoechoic areas, possibly due to a greater degree of liquefaction (Figure 4).
Cine gradient echo magnetic resonance imaging sequences in 4-chamber (A) and 2-chamber view (B), showing a hypointense mass (star) in the inferior and lateral region of the mitral annulus, extending to the inferior basal segment; delayed postcontrast images showing late enhancement at the periphery of the lesion (C, arrowhead) and transmural late enhancement in the inferior mid-apical and apex segments (D, arrow).
This case illustrates the complementary role of multimodality imaging in a challenging diagnosis of caseous necrosis of the mitral annulus, in a patient with a cardioembolic infarction. While TTE identified the presence of the mass and its functional significance, CT confirmed its calcified nature and MRI was essential for excluding other potential etiologies as well as to confirm the infarction scar.
Conflicts of interestThe authors have no conflicts of interest to declare.