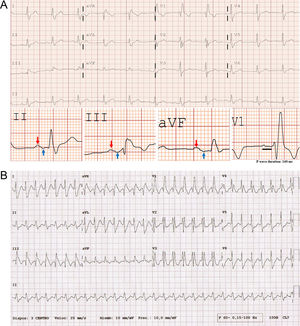
We present the case of a 79-year-old man with hypertension who reported episodes of palpitations without other symptoms and whose cardiopulmonary examination was normal. The ECG (Figure 1A) revealed sinus rhythm at 66 bpm with an advanced interatrial block (A-IAB) and a right bundle branch block.
(A) Sinus rhythm at 66 bpm with a prolonged and +/- biphasic P wave in the inferior leads (red arrow: + component; blue arrow: - component), which meets the criteria of advanced interatrial block and a right bundle branch block. (B) Regular wide QRS complex tachycardia at 171 bpm. The absence of AV dissociation or precordial concordance, RS interval <100 ms and typical right bundle branch block morphology (identical to the baseline ECG) suggests a supraventricular origin. An adenosine test was performed, unmasking atrial flutter (not shown).
One hour later, palpitations recurred. The ECG (Figure 1B) showed regular wide QRS complex tachycardia at 171 bpm. Adenosine administration unmasked a 2:1 atypical atrial flutter. Bayés syndrome (BS) was diagnosed. Electrical cardioversion was performed after ruling out atrial thrombi in a transesophageal echocardiogram.
Bachmann bundle (BB) is the preferential pathway driving sinus impulse from the right to left atrium. When it is blocked, P wave is prolonged >120 ms with a biphasic +/- morphology in the inferior leads (A-IAB pattern). If suspected, we suggest increasing the voltage and the speed of the ECG for better characterization. The anatomic substrate of A-IAB is atrial fibrosis involving BB, which explains why A-IAB is a marker of atriopathy with high specificity for the identification of left atria enlargement. BS is the association between A-IAB and atrial fibrillation/flutter. A-IAB is an easily identifiable and underestimated pattern that may encourage the clinician to look for runs of atrial fibrillation/flutter. A-IAB has been reported to be more prevalent among patients with embolic stroke. As we found atrial flutter in our patient, we began anticoagulation. We have still no evidence to prescribe anticoagulation for patients with A-IAB without atrial fibrillation/flutter and the results of prospective studies will be needed to design a randomized trial to assess the effect of anticoagulation in this population.
Conflicts of interestThe authors have no conflicts of interest to declare.