To characterize patients with atherosclerosis, a disease with a high socioeconomic impact, in the Lisbon and Tagus Valley Health Region.
MethodsA cross-sectional observational study was carried out through the Lisbon and Tagus Valley Regional Health Administration primary health care database, extracting data on the clinical and demographic characteristics and resource use of adult primary health care users with atherosclerosis during 2016. Different criteria were used to define atherosclerosis (presence of clinical manifestations, atherothrombotic risk factors and/or consumption of drugs related to atherosclerosis). Comparisons between different subpopulations were performed using parametric tests.
ResultsA total of 318 692 users were identified, most of whom (n=224 845 users; 71%) had no recorded clinical manifestations. The subpopulation with clinical manifestations were older (72.0±11.5 vs. 71.3±11.0 years), with a higher proportion of men (58.0% vs. 45.9%), recorded hypertension (78.3% vs. 73.5%) and dyslipidemia (55.8% vs. 53.5%), and a lower proportion of recorded obesity (18.2% vs. 20.8%), compared to those without clinical manifestations (p<0.001). Mean blood pressure, LDL-C and glycated hemoglobin values were lower in the subpopulation with manifestations (142/74 vs. 146/76 mmHg, 101 vs. 108 mg/dl, and 6.80 vs. 6.84%, respectively; p<0.001). Each user with atherosclerosis attended 4.1±2.9 face-to-face medical consultations and underwent 8.6±10.0 laboratory test panels, with differences in subpopulations with and without clinical manifestations (4.4±3.2 vs. 4.0±2.8 and 8.3±10.3 vs. 8.7±9.8, respectively; p<0.001).
ConclusionsAbout one in three adult primary health care users with atherosclerosis have clinical manifestations. The results suggest that control of cardiovascular risk factors is suboptimal in patients with atherosclerosis.
Caracterizar os doentes com aterosclerose, uma doença com elevado impacto socioeconómico, na Região de Saúde de Lisboa e Vale do Tejo.
MétodosEstudo observacional transversal, recorrendo ao Sistema de Informação desta Administração Regional de Saúde, com extração de dados clínico-demográficos e de consumo de recursos dos utilizadores adultos com aterosclerose em 2016. A aterosclerose foi definida pela presença de manifestações clínicas, fatores de risco aterotrombóticos e/ou consumo de medicamentos marcadores de aterosclerose. Foram comparados os resultados para a população com e sem manifestações clínicas (testes paramétricos).
ResultadosIdentificámos 318 692 utilizadores, a maioria (n=224 845 doentes; 71%) sem registo de manifestações clínicas. A subpopulação com manifestações clínicas era mais idosa (72,0±11,5 versus 71,3±11,0 anos), com maior proporção de homens (58,0% versus 45,9%), registo de hipertensão arterial (78,3% versus 73,5%), dislipidemia (55,8% versus 53,5%) e menor proporção de registo de obesidade (18,2% versus 20,8%), em comparação com a população sem manifestações clínicas (p<0,001). Os valores médios de pressão arterial sistólica/diastólica, C-C-LDL e hemoglobina glicada foram inferiores na subpopulação com manifestações (142/74 versus 146/76 mmHg, 101 versus 108 mg/dL, 6,80 versus 6,84%, respetivamente; p<0,001). Cada utilizador com aterosclerose realizou 4,1±2,9 consultas médicas presenciais e 8,6±10,0 painéis de análises clínicas, com diferenças nas subpopulações com e sem manifestações clínicas (4,4 ± 3,2 versus 4,0 ± 2,8 e 8,3 ± 10,3 versus 8,7±9,8, respetivamente; p<0,001).
ConclusõesCerca de um em cada três utilizadores adultos de cuidados de saúde primários com aterosclerose têm manifestações clínicas. Os resultados sugerem que o controlo dos factores de risco cardiovascular é sub-óptimo em doentes com aterosclerose.
Atherosclerosis is a chronic arterial disease with a recognized socioeconomic impact due to the mortality and morbidity associated with its clinical manifestations.1 In 2016 in Portugal, the clinical manifestations of atherosclerosis, which include ischemic heart disease (IHD), cerebrovascular disease (CVD) and peripheral arterial disease (PAD), were responsible for 15 123 deaths, around 50% of deaths from diseases of the circulatory system and 14% of overall mortality.2 Besides mortality, these clinical manifestations are associated with considerable disability, resulting not only from the acute event but also from the frequent sequelae.3
The acute event usually results in admission to hospital. In Portugal in 2016, atherosclerosis was responsible for 54 813 episodes of hospitalization.4 During the rest of the disease's natural history – both pre-clinical and symptomatic – patients are treated in outpatient care, in both hospital and primary health care settings.
The main objective of this study was to describe the clinical and demographic characteristics and resource use of adult patients with atherosclerosis, using data on the population of primary health care users in the Lisbon and Tagus Valley Health Region in 2016. The secondary aim was to compare subpopulations with and without clinical manifestations of atherosclerosis and subgroups with different manifestations, concerning clinical and demographic variables and resource use.
MethodsA cross-sectional observational study was carried out through the primary health care database (SIARS) of the Lisbon and Tagus Valley Regional Health Administration (ARS LVT), extracting clinical and demographic data and patterns of resource use of primary health care users with atherosclerosis during 2016 (the latest year for which complete data were available at the time of this study). The study follows the STROBE guidelines5 and was approved by the health ethics committee of ARS LVT (010/CES/INV/2018).
Data sourcesThe data source used was the SIARS. This system is based on a data repository model, fed mainly from the computer systems used in primary health care. Clinical data are recorded by physicians during general practice consultations. For medications, the data are provided by the Control and Monitoring Center of the Portuguese National Health Service and include information on medications that were invoiced (and therefore delivered to users), whatever the origin of the prescription. The process of data extraction was carried out by the ARS LVT using the SIARS in accordance with the research protocol. The extracted data were completely and irreversibly anonymized and were subsequently analyzed by the authors.
PopulationPatients fulfilling the following cumulative inclusion criteria were included: age ≥18 years at enrollment; at least one consultation recorded in the SIARS of LVT ARS between January 1 and December 31, 2016; and at least one criterion of atherosclerosis. Three different criteria were used to identify cases of atherosclerosis and increase diagnosis sensitivity: a record of at least one clinical manifestation of atherosclerosis in any field of the SIARS database (‘manifestations’ criterion); the presence of at least three atherothrombotic risk factors (‘risk factor’ criterion); or prescription of an antiplatelet agent, naftidrofuryl or pentoxifylline (‘medication’ criterion).
The second edition of the International Classification of Primary Care (ICPC-2)6 was used to identify clinical manifestations of atherosclerosis. The ‘manifestations’ definition was thus based on the focal manifestations of atherosclerosis: IHD (ICPC-2 codes K75 [acute myocardial infarction], K74 [ischemic heart disease with angina], and K76 [ischemic heart disease without angina]), CVD (codes K89 [transient cerebral ischemia] and K90 [stroke/cerebrovascular accident]), and PAD (code K92 [atherosclerosis/peripheral vascular disease]).
The ‘risk factors’ definition of atherosclerosis was based on a list of nine atherothrombotic risk factors used in the REduction of Atherothrombosis for Continued Health (REACH) registry,7 one of the most important studies characterizing the population with atherosclerosis worldwide. Of these, a list of six atherothrombotic risk factors was drawn up for which data could be extracted from the SIARS: age ≥65 years in men or ≥70 years in women, smoking status, systolic blood pressure (BP) ≥150 mmHg, microalbuminuria ≥30 μg/ml, prescription of at least one antidiabetic medication, and prescription of lipid-modifying medication. Patients were considered to be smokers if code P17 of the ICPC-2 or the number of cigarettes smoked per day was recorded.
The Anatomical Therapeutic Chemical (ATC) Classification System8 was used to identify medications included in the ‘risk factors’ and ‘medications’ definitions of atherosclerosis, as this system is used in the SIARS.
VariablesAll subjects were characterized in terms of general characteristics (such as gender), cardiometabolic risk factors (such as BP), and comorbidities (such as the presence of other cardiovascular diseases), as well as health resource use (number of consultations by type, number of nursing contacts, complementary diagnostic and therapeutic procedures performed, medications dispensed and their retail price). Only those diagnostic and therapeutic procedures and medications that were directly relevant to atherosclerosis were analyzed.
Variables were characterized for the period January 1 to December 31, 2016. Variables relating to cardiometabolic risk factors included the last assessment available in that year.
The variables were operationalized according to type (nominal or numeric) identifying health problems based on the ICPC-26 (Supplementary Table 1), complementary diagnostic and therapeutic procedures based on the table of these procedures reimbursed by the National Health Service9 (Supplementary Table 2), and pharmacological therapy based on the ATC classification system8 (Supplementary Table 3).
When data on the different variables had been collected, a summary analysis was performed to exclude outliers. For variables relevant to cardiometabolic risk factors, expert opinion was used to define limits of values that were used as a reference for conformity. Values outside these limits were considered clinically implausible (such as negative values for blood pressure, weight or cholesterol) and were excluded from the analysis. The number of observations excluded did not exceed 1% of the total in any of the variables.
Statistical analysisThe statistical analysis was carried out using R software, version 3.6.1 (R Core Team 2019. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria). For the descriptive analysis absolute and relative frequency tables, means and standard deviation, or medians and interquartile range were used, as appropriate. Given the size of the sample,10 parametric tests were used to compare results between the populations with and without clinical manifestations. As this was an observational and exploratory study, a p-value of ≤0.001 was taken to indicate statistical significance.
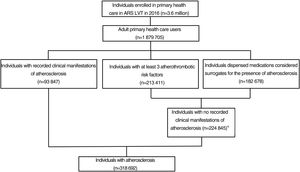
ResultsA total of 318 692 adults who had general practice consultations in the Lisbon and Tagus Valley Health Region and who met at least one of the criteria defining atherosclerosis were identified (Figure 1). About 51% were female (n=161 074). Ages ranged between 18 and 108 years, with a mean of 71.5±11.1 years. The proportion of those aged ≤45 years was 2.3% (n=7396). Hypertension, present in 75% of cases, was the most frequent comorbidity (Table 1).
Clinical and demographic characteristics of the population with atherosclerosis, according to the presence of clinical manifestations.
| Total (n=318 692) | With recorded manifestations (n=93 847) | Without recorded manifestations (n=224 845) | Difference (with vs. without manifestations) | |
|---|---|---|---|---|
| Age, years, mean (SD) | 71.5 (11.1) | 72.0 (11.5) | 71.3 (11.0) | 0.64* |
| Male, % | 49.5 | 58.0 | 45.9 | 12.1* |
| Hypertension, % | 74.9 | 78.3 | 73.5 | 4.8* |
| Dyslipidemia, % | 54.2 | 55.8 | 53.5 | 2.3* |
| Diabetes, % | 40.8 | 37.0 | 42.4 | -5.4* |
| Obesity, % | 20.0 | 18.2 | 20.8 | -2.5* |
| Overweight, % | 16.3 | 16.3 | 16.2 | 0.1 |
| Atrial fibrillation/flutter, % | 5.4 | 8.7 | 4.1 | 4.7* |
| Heart failure, % | 5.1 | 9.6 | 3.3 | 6.3* |
SD: standard deviation.
The subpopulation without recorded clinical manifestations (n=224 845) represented 71% of the total population with atherosclerosis. In this group, 71% fulfilled the ‘risk factors’ criterion, with at least three atherothrombotic risk factors, while the other 29% were selected based on the ‘medications’ criterion.
Of those with recorded clinical manifestations(n=93 847; 29% of the total), 13% (n=12 168) presented manifestations in two vascular beds and 1% (n=1116) in three (coronary, cerebrovascular and peripheral).
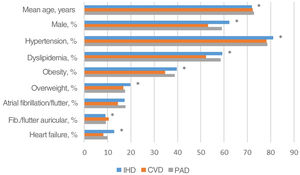
Differences were observed in most clinical and demographic characteristics, both between patients with and without clinical manifestations (Table 1) and in the subgroups with different types of manifestations (Figure 2).
Clinical and demographic characteristics of patients with clinical manifestations of atherosclerosis according to type. CVD: cerebrovascular disease; IHD: ischemic heart disease; PAD: peripheral arterial disease. *: p<0.0001 for the difference between the subpopulations (mutually exclusive) with different clinical manifestations (IHD, CVD, PAD and at least two of these manifestations).
The subpopulation with clinical manifestations was older (72.0±11.5 vs. 71.3±11.0 years) and had a higher proportion of males (58.0% vs. 45.9%), patients with hypertension (78.3% vs. 73.5%), dyslipidemia (55.8% vs. 53.5%), atrial fibrillation/flutter (8.7% vs. 4.1%) and heart failure (9.6% vs. 3.3%), and a lower prevalence of obesity (18.2% vs. 20.8%) compared to the population without clinical manifestations (p<0.001 for all comparisons).
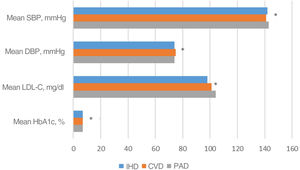
With regard to cardiometabolic risk factors, higher values of systolic BP (SBP) and diastolic BP (DBP), low-density lipoprotein cholesterol (LDL-C) and glycated hemoglobin (HbA1c) were observed in the subpopulation without recorded clinical manifestations (146 mmHg, 76 mmHg, 108 mg/dl and 6.84%, respectively) than in patients with clinical manifestations (142 mmHg, 74 mmHg, 101 mg/dl and 6.80%, respectively; p<0.001 for all comparisons) (Table 2). In the subpopulation with clinical manifestations, differences were also observed according to the type of manifestation (Figure 3).
Indicators of cardiometabolic risk factors in the population with atherosclerosis according to the presence of clinical manifestations.
| Total (n=318 692) | With recorded manifestations (n=93 847) | Without recorded manifestations (n=224 845) | Difference (with vs. without manifestations) | |
|---|---|---|---|---|
| SBP, no. of readings | 261 698 | 75 095 | 186 603 | |
| SBP, mmHg, mean (SD) | 145 (21) | 142 (21) | 146 (20) | -4.0* |
| DBP, no. of readings | 261 648 | 75 087 | 186 561 | |
| DBP, mmHg, mean (SD) | 76 (11) | 74 (11) | 76 (11) | -1.9* |
| LDL-C, no. of readings | 139 432 | 38 126 | 101 306 | |
| LDL-C, mg/dl, mean (SD) | 106 (37) | 101 (36) | 108 (37) | -7.5* |
| HbA1c, no. of readings | 121 491 | 31 854 | 89 637 | |
| HbA1c, %, mean (SD) | 6.8 (1.2) | 6.8 (1.2) | 6.8 (1.2) | -0.04* |
DBP: diastolic blood pressure; HbA1c: glycated hemoglobin; LDL-C: low-density lipoprotein cholesterol; SBP: systolic blood pressure.
Indicators of cardiometabolic risk factors in the population with clinical manifestations of atherosclerosis according to type. CVD: cerebrovascular disease; DBP: diastolic blood pressure; HbA1c: glycated hemoglobin; IHD: ischemic heart disease; LDL-C: low-density lipoprotein cholesterol; PAD: peripheral arterial disease; SBP: systolic blood pressure. *: p<0.0001 for the difference between the subpopulations (mutually exclusive) with different clinical manifestations (IHD, CVD, PAD and at least two of these manifestations).
We also carried out a descriptive and exploratory analysis of the control of cardiometabolic risk factors, focusing on patients with hypertension (n=238 850; 75%) and those with diabetes (n=130 167; 41%), since target values for these two risk factors are well established. The proportion of patients with high BP (SBP ≥140 mmHg and/or DBP ≥90 mmHg) was higher in the subpopulation without clinical manifestations (63.0% vs. 53.4%). Among patients with diabetes, the proportion with HbA1c ≥7% was lower in those without manifestations, although the difference was small (40.2% vs. 41.1%). Similar results were obtained using higher HbA1c target levels.
With regard to medications, almost all patients (n=315 340; 99%) consumed at least one of the drug classes analyzed. Lipid-modifying agents (ATC code C10) were used by the largest number of patients (n=243 120; 76%), with an average of 5.9 packages per year per person.
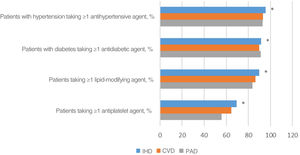
Table 3 summarizes the use of pharmacological therapy according to recorded risk factors for atherosclerosis (hypertension, diabetes and dyslipidemia) and to the use of antiplatelet agents. There were differences between the subpopulations with and without clinical manifestations in the use of antidiabetic and antiplatelet agents. Prescription patterns for all drug classes differed between patients with different types of clinical manifestations (Figure 4).
Use of pharmacological therapy by the population with atherosclerosis according to the presence of clinical manifestations.
| Total (n=318 692) | With recorded manifestations (n=93 847) | Without recorded manifestations (n=224 845) | Difference (with vs. without manifestations) | |
|---|---|---|---|---|
| No. of patients with hypertension | 238 850 | 73 508 | 165 342 | |
| ≥1 antihypertensive drug, % | 94.1 | 94.3 | 94.1 | 0.3 |
| No. of patients with diabetes | 130 167 | 34 739 | 95 428 | |
| ≥1 antidiabetic agent, % | 93.6 | 91.2 | 94.5 | -3.2* |
| No. of patients with dyslipidemia | 172 791 | 52 410 | 120 381 | |
| ≥1 lipid-modifying agent, % | 87.5 | 87.2 | 87.6 | -0.4 |
| Total no. of patients | 318 692 | 93 847 | 224 845 | |
| ≥1 antiplatelet agent, % | 50.5 | 64.0 | 44.9 | 19.1* |
Use of pharmacological therapy by the population with clinical manifestations of atherosclerosis according to type. CVD: cerebrovascular disease; IHD: ischemic heart disease; PAD: peripheral arterial disease. *: p<0.0001 for the difference between the subpopulations (mutually exclusive) with different clinical manifestations (IHD, CVD, PAD and at least two of these manifestations).
With regard to health resource use, during 2016 each patient had an average of 4.1±2.9 face-to-face consultations with a general practitioner and 3.4±9.8 nursing contacts. Around three-quarters of the population underwent at least one of the selected complementary diagnostic and therapeutic procedures. On average, each patient underwent 8.6±10.0 laboratory test panels, 0.5±0.9 cardiology exams and 0.1±0.4 radiology or nuclear medicine exams.
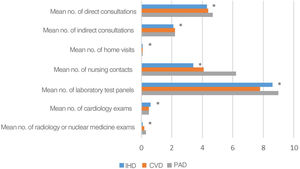
The number of consultations and diagnostic and therapeutic procedures was different between those with and without clinical manifestations (Table 4) as well as between subgroups with different types of manifestations (Figure 5).
Use of health resources (consultations, diagnostic procedures and treatments) by the population with atherosclerosis according to the presence of clinical manifestations.
| Total (n=318 692) | With recorded manifestations (n=93 847) | Without recorded manifestations (n=224 845) | Difference (with vs. without manifestations) | |
|---|---|---|---|---|
| Consultations | ||||
| Direct, mean (SD) | 4.1 (2.9) | 4.4 (3.2) | 4.0 (2.8) | 0.4* |
| Indirect, mean (SD) | 1.8 (2.5) | 2.1 (2.9) | 1.6 (2.4) | 0.5* |
| Home visits, mean (SD) | 0.0 (0.4) | 0.1 (0.5) | 0.0 (0.3) | 0.05* |
| Nursing contacts, mean (SD) | 3.4 (9.8) | 4.1 (11.7) | 3.1 (8.8) | 1.0* |
| Diagnostic procedures | ||||
| Laboratory test panels, mean (SD) | 8.6 (10.0) | 8.3 (10.3) | 8.7 (9.8) | -0.3* |
| Cardiology exams, mean (SD) | 0.5 (0.9) | 0.5 (0.9) | 0.5 (0.8) | 0.02* |
| Radiology/nuclear medicine exams, mean (SD) | 0.1 (0.4) | 0.2 (0.5) | 0.1 (0.4) | 0.1* |
SD: standard deviation.
Use of health care resources (consultations, diagnostic procedures and treatments) by the population with clinical manifestations of atherosclerosis, according to type. CVD: cerebrovascular disease; IHD: ischemic heart disease; PAD: peripheral arterial disease. *: p<0.0001 for the difference between the subpopulations (mutually exclusive) with different clinical manifestations (IHD, CVD, PAD and at least two of these manifestations).
This cross-sectional observational study characterized the population with atherosclerosis among primary health care users in the Lisbon and Tagus Valley Health Region. The differences found in clinical and demographic characteristics between the different subpopulations can be considered clinically plausible. The group with IHD, for example, had the highest proportion of recorded cases of heart failure (probably due to their underlying disease), while patients with CVD had the highest proportion of recorded diagnoses of atrial fibrillation (a known risk factor for ischemic stroke). On the other hand, the higher prevalence of diabetes (and proportion of diabetic patients medicated with antidiabetic agents) in the subpopulation without clinical manifestations may be due to the fact that the use of antidiabetic drugs was considered as an atherothrombotic risk factor. By contrast, no such factor would have caused the higher prevalence of obesity in this subpopulation.
Our results suggest that in the Lisbon and Tagus Valley Health Region, patients with no recorded clinical manifestations of atherosclerosis have worse BP and LDL-C control than those with manifestations. The proportion of hypertensive patients taking antihypertensive medication and patients with dyslipidemia taking lipid-modifying agents were similar in the two groups which suggests less intensive therapy. The proportion of diabetic patients taking antidiabetic medication in the subpopulation with clinical manifestations of atherosclerosis should be interpreted with caution, since this was one of the criteria used to select these individuals. Antiplatelet agents were used more in patients with clinical manifestations, which is to be expected and is in accordance with clinical guidelines.11,12
The population with PAD accounted for greater use of other health resources (consultations and complementary diagnostic and therapeutic procedures), with a higher number of nursing contacts and radiology or nuclear medicine exams. This may be due to the need for care of leg ulcers in nursing consultations and for diagnostic and follow-up exams such as Doppler lower limb echocardiography in patients with PAD, unlike other clinical manifestations.
The results of this observational study should be considered in the context of the health profile of the general population in Portugal, as well as of the results obtained by other authors studying populations with atherosclerosis.
In comparison with the Portuguese population in general, using as a reference the overall population enrolled in the Lisbon and Tagus Valley Health Region and recorded in the SIARS, higher proportions were found of patients with hypertension (74.9% vs. 21.1%), dyslipidemia (54.2% vs. 17.8%), diabetes (40.8% vs. 7.1%) and obesity (20.0% vs. 7.1%), as would be expected.13 If the reference used is the overall population who took part in the first National Health Examination Survey (INSEF 2015), the results are similar; in this survey the prevalence of hypertension was 36.0% and that of diabetes was 9.8%.14 The results of INSEF 2015 are in line with the prevalence estimated by the e_COR study (43.1% and 8.9% for hypertension and diabetes, respectively), and so the conclusions are similar for this comparison.15
Regarding the results obtained by other authors studying populations with atherosclerosis, we used one of the largest international studies on this population, the REACH registry,16 as a reference. This registry included 69 055 patients in 44 countries worldwide, including Portugal, with clinical manifestations and/or at least three atherothrombotic risk factors, including those being treated at the time of enrollment. The registry aimed to characterize risk factors and the incidence of atherothrombotic events in populations with atherosclerosis around the world. Unlike the sample in our study, the REACH registry mainly included patients with clinical manifestations (82% vs. 29%), a difference that may be explained by the fact that general practitioners accounted for only 44% of recruiting physicians in the REACH registry. Nevertheless, in the subpopulation with clinical manifestations, the results of the two studies are similar regarding the recorded prevalence of hypertension (78% vs. 80%) and the prescription of antidiabetic agents (36% vs. 38%) and lipid-modifying drugs (73% vs. 70%). In terms of age (72 vs. 68 years), proportion of males (58% vs. 67%) and presence of obesity (18% vs. 27%), the differences are more pronounced, probably due to the demographic characteristics of health care users in the Lisbon and Tagus Valley Health Region, and, in the case of obesity, may also be related to differences in the way health problems are coded.
In patients with clinical manifestations, the proportions of hypertensive and diabetic patients in our study receiving antihypertensive and antidiabetic medications, respectively, were similar to or higher than those estimated in the REACH registry.16 With regard to control of risk factors, particularly hypertension, the control rate was higher in REACH (50% vs. 40%). However, as pointed out above, most of the population of the REACH registry presented clinical manifestations of atherosclerosis, and so therapeutic targets could have been different, which would explain their better results.
The number of adult users with atherosclerosis in the Lisbon and Tagus Valley Health Region (estimated at 318 692 individuals in 2016) represents about 17% of the overall number of health care users in this Health Region in that year (1 879 705). Of those with atherosclerosis, 29% had symptomatic disease, which was polyvascular in 14% of cases. The subjects included in the present study were identified using different criteria defining atherosclerosis (presence of clinical manifestations, atherothrombotic risk factors and/or consumption of drugs related to atherosclerosis). These criteria enabled patients to be included from the whole spectrum of atherosclerotic disease, both symptomatic and asymptomatic, and simultaneously to address the issue of coding of health problems, which often generates bias in studies of administrative databases.17 Using the ‘risk factors’ and ‘medications’ definitions led to the inclusion of a total of 224 845 individuals without recorded clinical manifestations. However, certain points should be noted. Firstly, we found that the codes used may not have affected all diseases equally. For example, in the case of diabetes, the number of patients with the ICPC-2 codes for diabetes (T89 or T90) was close to that of patients prescribed antidiabetic medications (A10 in the ATC classification) (130 167 vs. 133 728 individuals, respectively). Secondly, 64 164 individuals were included solely on the ‘medications’ definition, 16% of them (n=10 330) because they were taking naftidrofuryl or pentoxifylline and the other 84% (n=53 834) only because they were taking antiplatelet agents. The inclusion of these patients was based on the assumption that these therapies were being prescribed for unrecorded PAD (naftidrofuryl or pentoxifylline) or as primary or secondary prevention of atherothrombotic events (antiplatelets), which may constitute a limitation. Thirdly, although among the selected risk factors, data on smoking status were not presented due to difficulties in interpreting, the data extracted from the SIARS. It was possible to ascertain previous contact with tobacco but not current smoking status. Finally, our study focused on users of primary health care, and so the numbers of patients identified should not be used to estimate the overall prevalence of atherosclerosis in the Lisbon and Tagus Valley Health Region. Even so, characterization of these patients will help to understand the disease and its clinical relevance.
Despite the advantages of very large populations such as ours in studying the clinical and demographic characteristics of patients with atherosclerosis, it is well known that in samples of this size minimal differences may be found with statistical significance, but without clinical relevance.18 Furthermore, the statistical analysis consisted of non-adjusted comparisons, so the statistical tests presented should be interpreted with caution.
The present study highlights the value of analyzing data in the SIARS for research purposes, extending the usefulness of these data beyond the administrative purposes for which the database was initially designed. However, the validity of the coding systems used, in terms of their diagnostic sensitivity and specificity, should be the subject of a separate analysis, which was beyond the scope of the present work.
ConclusionAccording to the results of our study, around one in three adult primary health care users with atherosclerosis in the Lisbon and Tagus Valley Health Region have recorded clinical manifestations. Our findings suggest that control of cardiovascular risk factors is suboptimal in patients with atherosclerosis.
FundingThis study was funded by an unrestricted grant from Bayer Portugal, SA. The funding was not conditional on the nature of the results, which are entirely the responsibility of the authors.
Conflicts of interestAMeS received personal fees and grants/other support from Amgen, Bayer, Daiichi Sankyo, Jaba Recordati, Menarini, Mylan, Novartis, Tecnimede, outside the study. F.A. received grants and personal fees from AstraZeneca, Bayer, Bial, Daiichi Sankyo, Ferrer, Jaba Recordati, Merck Sharp & Dohme, outside the study. V.G. received personal fees and grants/other support from Bayer, AstraZeneca, Daiichi Sankyo, Amgen, Novartis, Boehringer Ingelheim, outside the study.
JC, RA, FL, AVC and MB are members of CEMBE, which has received unrestricted funding from over 20 pharmaceutical companies for other projects, including Bayer Portugal SA.; FF and JA were members of CEMBE at the time of the study; MG has taken part in several pharmacoeconomic research projects that received unrestricted grants from several pharmaceutical companies, including Bayer Portugal SA.
We would like to thank the Lisbon and Tagus Valley Regional Health Administration (ARS LVT) for providing access to the data housed in the region's primary health care database (SIARS).