A 65-year-old male underwent an echocardiogram after a transient ischemic attack which revealed an apparent noncoronary sinus of Valsalva aneurysm (SOVA) with a shunt flow from the aorta into the right atrium.
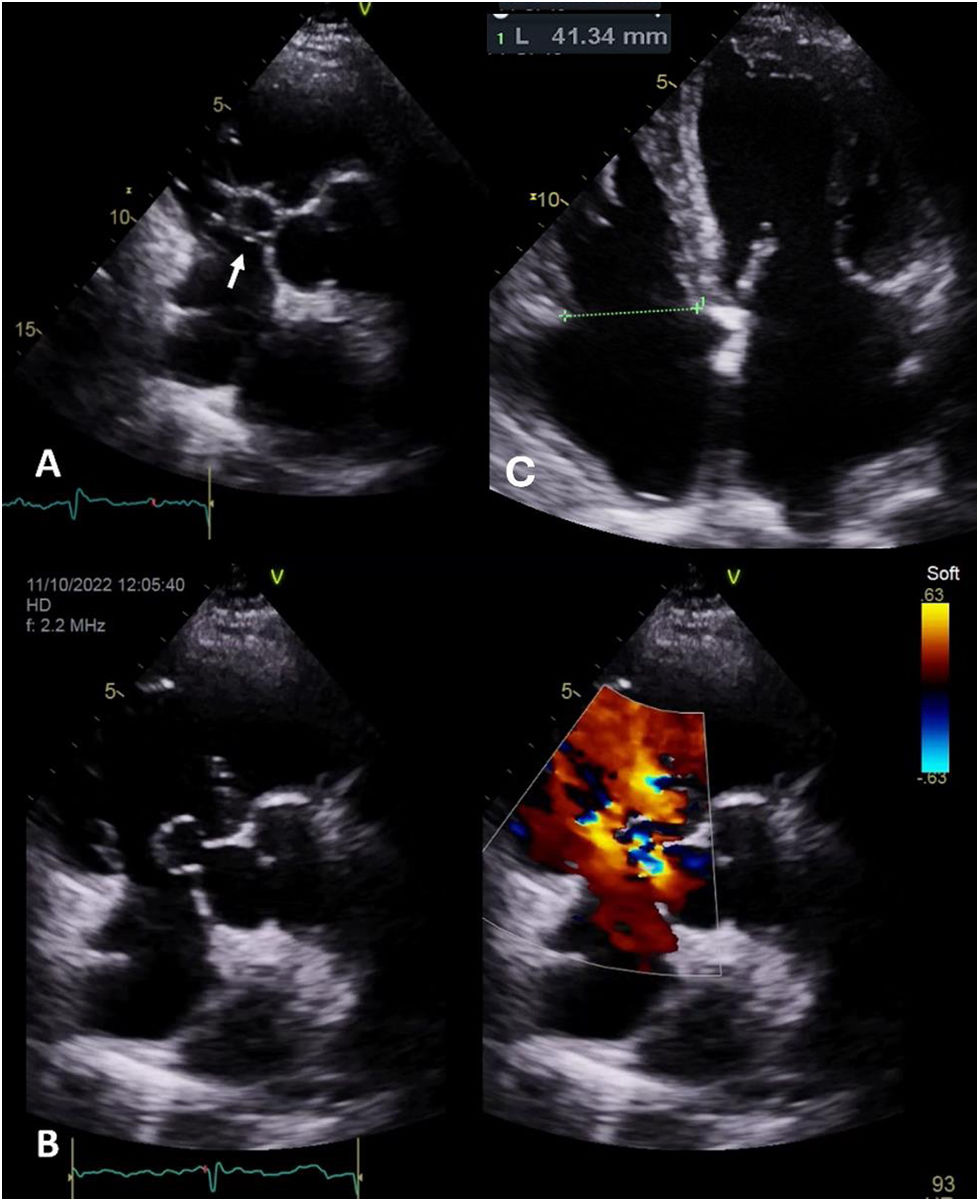
At the first evaluation, the patient was asymptomatic and maintained regular physical activity (used to run 10 km twice a week). The physical examination was unremarkable except for a slight continuous heart murmur. Transthoracic and transesophageal echocardiogram confirmed the existence of an aorto-atrial fistula with left to right cardiac shunt, caused by a rupture SOVA (Figure 1A and B; videos 1–4) with dilatation of the right heart chambers (Figure 1C).
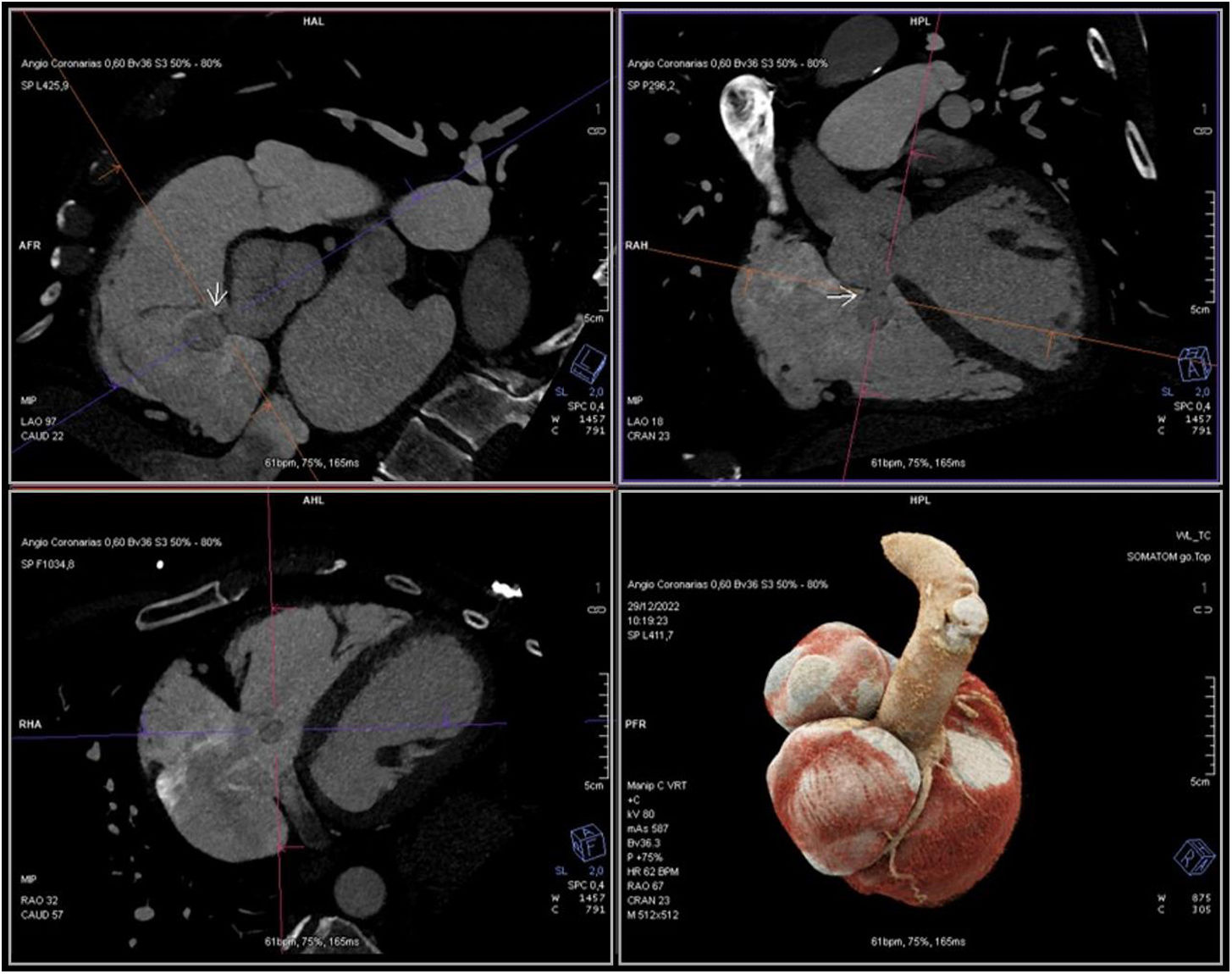
He had undergone no prior aortic surgery nor had he experienced chest trauma. Infections and connective tissue disorders capable of weakening the elastic tissue were excluded. The coronary computed tomography angiography excluded atherosclerotic coronary artery disease and showed the aneurysm again (Figure 2). Postcapillary pulmonary hypertension was confirmed by right heart catheterization and pulmonary–systemic flow ratio (Qp/Qs) was 2.1.
The patient underwent successful surgical repair of the fistula with direct suture.
SOVA is a rare condition among the general population (0.09%). It is a congenital or acquired discontinuity between the aortic valve annulus and the aortic media caused by weakness or degeneration of the elastic connective tissue.
SOVA may be silent and found incidentally, but the rupture of a SOVA is a devastating event that leads to symptoms of heart failure or cardiac tamponade and carries a poor prognosis if left untreated. In this case, the presence of the aorto-atrial fistula along with the evidence of right heart overload reveal signs of some chronicity, making the absence of symptoms unexpected.
Patient consentThe authors confirm that consent for submission and publication of this case has been obtained from the patient.
FundingNone declared.
Conflict of interestThe authors declare that there is no conflict of interest.