Use of invasive physiological assessment in patients with coronary artery disease varies widely and is perceived to be low. We aimed to examine adoption rates as well as patterns and determinants of use in an unselected population undergoing invasive coronary angiography over a long time frame.
MethodsWe retrospectively determined the per-procedure prevalence of physiological assessment in 40821 coronary cases performed between 2007 and 2018 in two large-volume centers. Adoption was examined according to procedure type and patient- and operator-related variables. Its association with relevant scientific landmarks, such as the release of clinical trial results and practice guidelines, was also assessed.
ResultsOverall adoption was low, ranging from 0.6% in patients undergoing invasive coronary angiography due to underlying valve disease, to 6% in the setting of stable coronary artery disease (CAD); it was 3.1% in patients sustaining an acute coronary syndrome. Of scientific landmarks, FAME 1, the long-term results of FAME 2 and the 2014 European myocardial revascularization guidelines were associated with changes in practice. Publication of instantaneous wave-free ratio (iFR) trials had no influence on adoption rates, except for a higher proportion of iFR use. In 42.9% of stable CAD patients undergoing percutaneous coronary intervention there was no objective non-invasive evidence of ischemia, nor was physiological assessment performed. Younger operator age (4.5% vs. 4.0% vs. 0.9% for ages <40, 40-55 and >55 years, respectively; p<0.001) and later time of procedure during the day (2.9% between 6 and 8 p.m. vs. 4.4% at other times) were independent correlates of use of invasive physiology.
ConclusionsOur study confirms the low use of invasive physiology in routine practice. The availability of resting indices did not increase adoption. Strategies are warranted to promote guideline implementation and to improve patient care and clinical outcomes.
A avaliação funcional invasiva da doença coronária varia significativamente na prática clínica e em geral parece ser subutilizada. O objetivo deste estudo foi determinar a sua adoção no mundo real, assim como estudar os padrões e os principais determinantes da sua utilização, numa população não selecionada de doentes submetidos a coronariografia invasiva, ao longo de um período alargado.
MétodosA prevalência da avaliação funcional invasiva foi determinada retrospetivamente, por procedimento, em 40 821 casos realizados entre 2007 e 2018, em dois centros de grande volume. As taxas de adoção foram avaliadas de acordo com variáveis relacionadas com o procedimento, com o doente e com o operador, assim como em relação com marcos científicos relevantes, como a publicação de resultados de ensaios clínicos e de recomendações internacionais.
ResultadosDe acordo com o contexto clinico, a utilização variou entre 0,6% em doentes submetidos a coronariografia no contexto de patologia valvular e 6% em doentes com doença coronária estável (DAC) e foi 3,1% em doentes com síndroma coronária aguda. Dos marcos científicos estudados, a publicação dos resultados do estudo FAME 1, dos resultados a longo prazo do FAME 2 e das Recomendações para a Revascularização da ESC de 2014 associaram-se às taxas de adoção. Para além de um aumento da utilização do iFR, a publicação dos ensaios clínicos consubstanciando clinicamente o seu uso não influenciou a utilização global de fisiologia invasiva. Em 42,9% dos doentes com DAC estável submetidos a angioplastia, não havia referência a isquémia objetivável nem foi utilizada fisiologia invasiva. A idade dos operadores (4,5% versus 4,0% versus 0,9% para idades < 40, 40-55 e > 55 anos, respetivamente; p < 0,001) e a hora de realização do procedimento (2,9% entre as 6-8PM versus 4,4% durante o restante dia) relacionaram-se inversamente com a utilização de fisiologia durante os procedimentos.
ConclusõesEsta análise confirma a baixa de utilização da avaliação funcional invasiva na prática clínica. A disponibilidade de evidência sobre o uso de índices não hiperémicos não aumentou a adoção. São necessárias estratégias dirigidas que potenciem a implantação das recomendações, de forma que o manejo dos doentes com doença coronária e os benefícios clínicos da estratificação invasiva possam ser aprimorados.
Fractional flow reserve (FFR)-guided revascularization has been widely validated and is associated with added net benefits in patient-oriented health outcomes, as compared to angiography alone.1,2 The instantaneous wave free ratio (iFR) has proved to be similar to FFR concerning clinical outcomes,3,4 and additional evidence suggests that other diastolic pressure indices are numerically similar to iFR and may be used interchangeably.5,6 The reasons for the underuse of invasive physiology during diagnostic and interventional procedures in daily practice are not fully clear, despite extensive validation7 and guideline recommendations,8,9 and may also be subject to geographical variations. In addition, there is no consensus on how actual adoption should be calculated. In most reports, the number of percutaneous coronary interventions (PCI) is used as the denominator, which may result in underestimation, as it does not account for procedures in which revascularization may not have been performed consequently to a negative functional interrogation.
The aim of the present study was to describe the prevalence of physiological assessment in a large unselected population undergoing invasive coronary angiography (ICA) in an unbiased setting over a long 12-year time span, and to elucidate its patterns and determinants of use.
MethodsStudy definitions and design and data collectionData on all ICA exams performed for any clinical indication in two large-volume centers in Portugal between January 2007 and December 2018 were analyzed retrospectively. Patient-, angiographic- and procedure-related data were recorded in a dedicated electronic database (Cardiobase®, Infortucano™) at the time of the index procedure by the attending team. Information was extracted separately from each center's database and then merged into a single dataset. To ensure consistency, similar queries were used for data retrieval. All patients provided written informed consent for the procedure and data collection in accordance with local institutional review board guidelines.
Use of invasive functional assessment was assessed per procedure. Diagnostic procedures in which PCI was deferred based on invasive physiology were also considered when determining adoption rates. Functional studies included FFR, resting full-cycle distal-to-aortic pressure ratio (Pd/Pa) and iFR. Attempted percutaneous coronary intervention included all cases in which PCI was decided and attempted, regardless of procedural success.
The adoption of physiological assessment was analyzed over the study period according to scientific landmarks, which included the publication of relevant clinical trials and the European guidelines on the management of stable coronary artery disease (CAD) and myocardial revascularization,9–11 and also according to operator experience, time of the procedure during the workday, availability and type of baseline non-invasive testing prior to ICA, CAD extent and whether or not PCI was subsequently performed.
Study population and definition of the clinical indication for coronary angiographyAll patients undergoing ICA for any clinical indication were included. Indications were classified as stable CAD, ongoing acute coronary syndrome (ACS), recent ACS, valve disease, or miscellaneous indications. Uniform definitions of each clinical indication are provided in the online Supplementary Material.
Statistical analysisContinuous variables are expressed as means and standard deviations and were compared using the unpaired t test or the Mann-Whitney U test, as appropriate. Categorical variables are expressed as proportions and were compared using the chi-square test. Normality was tested with the Kolmogorov-Smirnov test and by visual inspection of Q-Q plots.
Independent predictors of the use of invasive physiology were assessed using binary logistic regression models. To examine the impact of time-varying scientific landmarks, the variable was entered in the model as categorical. Use of a repeated contrast method means that estimations represent the odds between contiguous categories, rather a comparison with any given reference category. Model calibration and discriminative power were assessed with the Hosmer-Lemeshow goodness-of-fit test and the area under the receiver operating characteristic curve, respectively. A two-sided p-value of less than 0.05 was considered to indicate statistical significance. Statistical analysis was performed with IBM® SPSS® Statistics version 23.
ResultsPopulation baseline characteristicsBetween January 2007 and December 2018, 40821 procedures were performed, in which PCI was attempted in 42.1% of cases (n=17183). ACS was the most common indication for ICA (35.5% ongoing ACS and 8% recent ACS cases). Patients’ baseline characteristics and clinical indications for ICA are further detailed in Table 1.
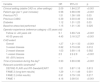
Baseline patient and procedural characteristics in the overall cohort and according to use of invasive physiology in invasive coronary angiography.
| Variable | Overall population (n=40821) | Angiography group (n=39190) | Physiology group (n=1631) | p |
|---|---|---|---|---|
| Demographic | ||||
| Age, years, mean±SD | 66.2±12 | 66.2±12.1 | 65.1±10.9 | <0.001 |
| Male gender | 27239 (66.7%) | 26073 (66.5%) | 1166 (71.5%) | <0.001 |
| Previous clinical history | ||||
| Diabetes | 12686 (31.1%) | 12088 (30.8%) | 598 (36.7%) | <0.001 |
| Hypercholesterolemia | 23483 (57.5%) | 22417 (57.3%) | 1066 (65.5%) | <0.001 |
| Hypertension | 30108 (73.8%) | 28845 (73.7%) | 1263 (77.5%) | 0.001 |
| Smoking history | 15671 (38.4%) | 14989 (38.3%) | 682 (41.8%) | 0.004 |
| Family history of CVD | 3477 (8.5%) | 3308 (8.5%) | 169 (10.4%) | 0.006 |
| Peripheral arterial disease | 2407 (5.9%) | 2311 (5.9%) | 96 (5.9%) | 0.987 |
| Stroke | 3161 (7.7%) | 3049 (7.8%) | 112 (6.9%) | 0.346 |
| Previous myocardial infarction | 9251 (22.7%) | 8430 (21.5%) | 438 (26.9%) | <0.001 |
| Previous PCI | 9733 (23.8%) | 9109 (23.2%) | 558 (34.2%) | <0.001 |
| Previous CABG | 3053 (7.5%) | 2973 (7.6%) | 80 (4.9%) | <0.001 |
| Cardiomyopathy | 144 (0.36%) | 134 (0.3%) | 10 (0.6%) | 0.082 |
| Valve disease (moderate or severe) | 5896 (14%) | 5824 (14.9%) | 72 (4.4%) | <0.001 |
| Heart transplantation | 35 (0.1%) | 35 (0.1%) | 0 | – |
| Clinical setting | <0.001 | |||
| Stable disease | 16223 (39.7%) | 15251 (39.1%) | 972 (59.6%) | |
| Ongoing ACS | 16109 (39.5%) | 15676 (40.2%) | 433 (26.5%) | |
| Recent ACS | 3234 (7.9%) | 3060 (7.8%) | 174 (10.7%) | |
| Valvular heart disease | 4017 (9.8%) | 3993 (10.2%) | 24 (1.5%) | |
| Miscellaneous | 1075 (2.6%) | 1054 (2.7%) | 21 (1.3%) | |
| Not reported | 163 (0.4%) | 156 (0.4%) | 7 (0.4%) | |
| Angiographic findings | <0.001 | |||
| All <50% lesions | 15324 (37.5%) | 14978 (38.2%) | 346 (21.2%) | |
| 1-vessel disease | 9627 (23.6%) | 9107 (23.2%) | 520 (31.9%) | |
| 2-vessel disease | 8315 (20.4%) | 7862 (20.1%) | 453 (27.8%) | |
| 3-vessel disease | 7555 (18.5%) | 7243 (18.5%) | 312 (19.1%) | |
| Coronary intervention | ||||
| PCI performed/attempted | 17183 (42.1%) | 16477 (42%) | 706 (43.3%) | 0.319 |
ACS: acute coronary syndrome; CABG: coronary artery bypass grafting; CVD: cardiovascular disease; PCI: percutaneous coronary intervention; SD: standard deviation.
Over the study period, physiology assessment was used in 1631 procedures (4%). Regarding the main clinical indications, adoption was 6.0% in stable CAD, 2.7% in patients suffering ongoing non-ST elevation ACS, 5.4% in patients with recent ACS (mostly for assessment of residual non-culprit lesions after primary PCI), 0.6% in patients undergoing ICA due to underlying valve disease, and 2.0% in other miscellaneous indications. Adoption was 4.1% considering all attempted PCI procedures as the denominator (n=17183) and 6.4% in stable CAD patients undergoing PCI (Supplementary Figure S10).
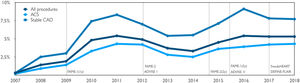
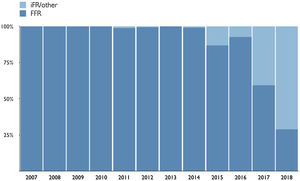
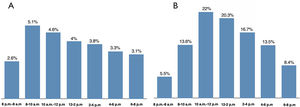
Adoption of invasive physiology according to scientific landmarksRates of invasive physiology over time, as well as their relationship with relevant landmarks, both overall and within the main clinical settings, are represented in Figure 1 and in Supplementary Figure S1A. Adoption increased significantly from 0.9% to 4.0% after the publication of FAME 11 in 2009 and remained stable thereafter, as no major changes were associated with the release of early results from FAME 2.12 Although the absolute annualized adoption rate was higher after 2015 (5% vs. 4% in the previous period; p=0.01), closer analysis demonstrates that it actually started rising in late 2014, temporally coinciding with the publication of the two-year results of the FAME 2 study (Supplementary Figure S1).13 Finally, following the publication of the two iFR outcome trials3,4 in early 2017, no increase was noted in the use of invasive physiology (either overall or in stable CAD), although the proportion of cases using iFR rather than FFR increased (Figure 2). These trends were consistent across the stable CAD and ACS clinical settings, which comprised more than 80% of all procedures.
European guidelines on myocardial revascularization were issued in August 2013,11 September 201410 and August 2018.9 In an analysis restricted to the population undergoing ICA in the setting of stable CAD, a significant 1.67-fold increase (95% confidence interval [CI] 1.28-2.19; p<0.001) in adoption rates (from 4.7% to 8%) was seen in the period following the release of the 2014 guidelines, which also coincided with the publication of the long-term (two-year) results of the FAME 2 study (Supplementary Figure S1B).
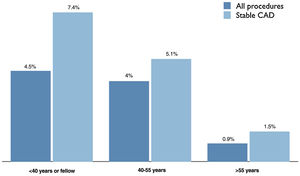
Relationship between physiological assessment and operator experienceThere was a statistically significant and independent association between operator experience and use of invasive physiology. Procedures performed by younger physicians were significantly more likely to include physiological assessment, both overall – 4.5% vs. 4.0% vs. 0.9% (p<0.001) – and in stable CAD – 7.4% vs. 5.1% vs. 1.5% (p<0.001) – for ages <40, 40-55 and >55 years, respectively (Figure 3 and Table 2).
Multivariate predictors of physiological assessment during invasive coronary angiography (n=1631).
| Variable | OR | 95% CI | p |
|---|---|---|---|
| Clinical setting (stable CAD vs. other settings) | 2.09 | 1.84-2.37 | <0.001 |
| Patient age (per 1-year increase) | 0.98 | 0.98-0.99 | <0.001 |
| Previous PCI | 1.51 | 1.36-1.69 | 0.03 |
| Previous CABG | 0.39 | 0.30-0.49 | 0.034 |
| Diabetes | 1.12 | 1.01-1.25 | 0.03 |
| Baseline stress test performed | 1.15 | 1.01-1.30 | 0.025 |
| Operator experience (reference category >55 years old) | |||
| Fellow or <40 years old | 5.1 | 3.69-7.24 | <0.001 |
| 40-55 years old | 4.45 | 3.16-3.27 | <0.001 |
| CAD extent | |||
| Overall | 1.27 | 1.21-1-33 | <0.001 |
| 3-vessel disease | 0.82 | 0.70-0.95 | 0.012 |
| 2-vessel disease | 1.03 | 0.90-1.18 | 0.582 |
| 1-vessel disease | 2.5 | 2.2-2.9 | <0.001 |
| All <50% lesions | – | – | – |
| Time of procedure during the daya | 0.93 | 0.90-0.96 | <0.001 |
| Relevant scientific landmarksb | |||
| DEFINE-FLAIR and iFR-SwedeHEART | 1.01 | 0.87-1.18 | 0.813 |
| FAME 2 (long-term results) | 1.29 | 1.11-1.49 | 0.001 |
| FAME 2 (initial results) | 0.91 | 0.79-1.05 | 0.217 |
| FAME 1 | 4.16 | 3.08-5.6 | <0.001 |
CABG: coronary artery bypass grafting; CAD: coronary artery disease; CI: confidence interval; OR: odds ratio; PCI: percutaneous coronary intervention.
Hosmer-Lemeshow goodness-of-fit test: chi-square=13.2; p=0.13. Area under the curve=0.72 (95% CI 0.71-0.74).
For the purpose of this analysis, considering the average overall prevalence, the threshold for high versus low adoption was set at 5% or more of use of physiological assessment, including all procedures. All operators <40 years-old were classified as high adopters (according to the study criteria), versus none in the age group >55 years. Temporal trends diverged in high versus low adopters. While in the former adoption followed the previously described general pattern, in the latter it was mostly insensitive to scientific landmarks (Supplementary Figure S2). In the low-adopter group, only the FAME 1 landmark was associated with an increase in adoption (adjusted odds ratio [OR] 7.0, relative to the prior time period; 95% CI 2.4-19.9; p<0.001), but still, overall penetration remained less than 3%.
Adoption of physiological assessment according to time of the procedure during the workdayThe proportion of procedures in which physiological assessment was used decreased progressively during the day, from 5.1% during the first two hours (8-10 a.m.) to 3.1% between 6 and 8 p.m. (Figure 4). The majority of cases with invasive measurements (61%) were performed between 10 a.m. and 4 p.m. (Figure 4B).
Association between physiological assessment and baseline non-invasive testing, coronary disease burden and percutaneous coronary interventionThe overall prevalence of non-invasive stress tests was 25.7%, varying widely between clinical settings (from 2% to 53.9%; Supplementary Figure S3). The association between baseline non-invasive tests and use of invasive physiology was highly inconsistent. In stable CAD and recent ACS patients, the availability of functional information prior to ICA was not associated with the use of invasive physiology (5.9% vs. 6.1% for stable CAD and 3.6% vs. 5.6% for recent ACS, in procedures with and without baseline testing, respectively (p=NS; Supplementary Figure S4). However, in ongoing ACS adoption was higher in cases in which a baseline stress test was available (6.7% vs. 2.4%; p<0.001). Among stable CAD cases (n=16223), the prevalence of physiological assessment was highest in multislice computed tomography (MSCT)-based referrals and in those with a negative non-invasive test at baseline (11% and 9.6% respectively; Supplementary Figure S5). In patients undergoing PCI who had no baseline non-invasive test available (either anatomical or functional), physiological assessment was used in only 6% of cases. Adoption was similar in procedures with non-specific positive ECG stress tests and imaging tests (6.8% and 6.3%, respectively), but was almost twice as high (11.9%) in patients in whom a baseline stress test had been performed but without evidence of ischemia (Supplementary Figures S6 and S7). Moreover, in 42.9% of stable CAD patients undergoing PCI, there was no record of inducible ischemia on non-invasive testing (including stress ECG), nor was physiological assessment performed.
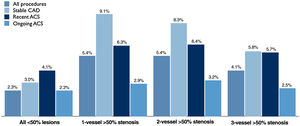
On univariate analysis, there was no consistent association between CAD extent and the pattern of invasive physiology (Figure 5). When all cases are taken together, physiological assessment was more frequently performed in patients with one- or two-vessel disease (5.4% in both) than in three-vessel disease (4.1%) or in cases with less severe disease (2.3%). In stable CAD, adoption actually decreased through the spectrum of increasing CAD severity (9.1% vs. 8.3% vs. 5.8% for one-, two- and three-vessel disease, respectively) and in ongoing ACS it was numerically similar from mild to three-vessel disease (2.3% vs. 2.9% vs. 3.3% vs. 2.5%).
Considering only interventional procedures, cases in which physiological assessment was used had a higher disease burden (1.8±0.9 vs. 1.6±0.9 vessels with >50% stenosis; p<0.001). Overall prevalence of PCI was similar in cases with and without physiological assessment (42% vs. 43.3%; p=0.30; Supplementary Figure S8); however, the ratio of vessels treated by PCI to the number of diseased vessels was marginally lower in invasive physiology-guided cases, suggesting less extensive intervention (Supplementary Figure S9).
Independent predictors of use of coronary physiological assessmentIn a multivariate binary regression model, the stable CAD clinical setting (versus other indications), diabetes, prior PCI and the availability of baseline stress tests were positive independent predictors of the use of invasive physiology. Prior CABG, time of the procedure during the workday and increasing patient age were inversely associated with the likelihood of use of invasive physiology in the index procedure. Also, younger operators – less than 40 and 40-55 years old – were four to five times more likely to use invasive physiology than older interventionists (>55 years old). As pointed out above, the overall association between CAD extent and use of physiology was inconsistent. In the multivariate model, increasing CAD extent (per diseased vessel) was associated with a significant 1.2-fold average greater likelihood of operators performing physiological assessment. However, this was driven by a higher OR in patients with one- and two-vessel disease compared both to milder cases and to three-vessel disease. Adjusted ORs of the independent predictors as well as model characteristics are summarized in Table 2.
DiscussionOur findings, which refer to a large cohort of patients undergoing ICA over a long time frame and encompassing a wide range of clinical scenarios, underscore (1) the low use of invasive physiological assessment of CAD in daily practice, regardless of the clinical setting; (2) that factors unrelated to procedural and patient characteristics significantly influenced penetration; and (3) that the clinical evidence sustaining the use of adenosine-free indices (mainly iFR) did not result in a significant increase in adoption.
Low adoption ratesDespite mounting evidence from randomized trials and large registries14,15 and also strong guideline recommendations,8,9,16 it is known that the use of invasive physiology varies widely and is generally perceived to be lower than expected.17–20 Our results are in line with these observations.
Although trends may be changing worldwide,21 partly due to more effective reimbursement policies, the underuse of invasive physiology-guided management is due to different reasons, ranging from technical and operator-related issues to site-specific and regional determinants. In some settings, factors such as unavailability or lack of funding have been pinpointed as the main reasons for the low uptake.18 Nevertheless, there is evidence that even when all potential external constraints are overcome, visual estimation continues to dominate treatment decisions for intermediate stenoses.22 The extent to which similar factors apply to our sample cannot be accurately quantified. However, considering the wide availability of the technology in Portugal and the virtually unrestricted reimbursement policies, it is unlikely that financial issues have played a significant role.
Clinical correlates of use of invasive physiologyDespite overall low adoption rates, the stable CAD clinical setting was an independent predictor of use of physiological assessment. This may be influenced by current recommendations, which are mostly applicable to stable CAD. Diabetes and previous PCI were also associated with higher adoption. Both subgroups had more extensive CAD, which was itself an independent predictor. The use of FFR and iFR in patients with diabetes has recently been analyzed in large cohorts and both indices have been shown to retain diagnostic and prognostic reliability.23,24 Conversely, prior CABG and increasing patient age were both inversely associated with the use of invasive physiology. It is conceivable that factors such as CAD complexity and comorbidity may have rendered operators less likely to consider additional diagnostic techniques. Also, concerns about microvascular dysfunction and adenosine hyporesponsiveness in elderly patients have been noted, compared to younger patients.13,25
Relationship with non-invasive functional tests, coronary artery disease extent and use of percutaneous coronary interventionOur findings underscore important complexities of patient workup, for which straightforward explanations may not be attainable based on available data alone. Considering the main clinical settings (stable CAD and ACS), no consistent pattern could be detected regarding the association between the availability of stress tests at baseline (including stress ECG) and the use of invasive physiology. Operators could have been expected to perform invasive physiology mostly in the absence of prior non-invasive tests for the detection and/or localization of ischemia. However, this was not the case, except in the subgroup with recent ACS, at least in part because many of these cases were patients with ST-elevation myocardial infarction and bystander disease, in whom the prevalence of stress tests was low (Supplementary Figure S4). Another possible explanation relies on the observation that most functional tests were treadmill ECG stress tests and single-photon emission computed tomography myocardial perfusion imaging, which may lack accuracy in a real-world environment,26,27 leading operators to use invasive physiology to clarify non-invasive findings, as in MSCT, in which no functional information is available at all. Nevertheless, the overall low penetration of physiological assessment renders further conclusions elusive.
The benefits of PCI in stable patients are thought to be linked to the severity of inducible ischemia,28,29 although recent evidence from randomized trials has questioned this approach.30,31 Even if this cannot be extended to other clinical settings, particularly ongoing ACS and valve disease, it is noteworthy that in our large cohort a high proportion of stable patients undergoing PCI had no demonstration of inducible ischemia, nor were invasive measurements performed. Although the ultimate reasons driving PCI in these cases – such as symptom severity, specific angiographic findings or information from intravascular imaging – cannot be definitively ascertained, this suggests that inappropriate revascularization potentially remains a significant problem.21 The perceived safety of current revascularization techniques (notably PCI) may be driving a persistent unwillingness to adopt coadjuvant technologies such as invasive physiological assessment. However, our findings reinforce the need for the implementation of strategies aiming at a wider adoption of physiological assessment, if clinical benefits are to be optimized.32,33
The routine integration of physiological measurements in the management of patients with CAD has moved pressure indices to the center of the diagnostic workflow and risk stratification of patients undergoing ICA.24 The more extensive the assessment and the greater the extent of CAD, the more likely are changes in the patient's management to occur, particularly when lesions are in fact intermediate.14,15 Significant heterogeneity was found in our study concerning the use of invasive physiology according to the extent of CAD (as measured by the number of diseased vessels). Although CAD extent was an overall predictor of adoption across all main clinical settings, lesion assessment was always lower in three-vessel CAD. A higher prevalence of chronic total occlusions and other features of anatomical and clinical complexity may have rendered these patients worse candidates for assessment with pressure wires, which on their own may lack important mechanical characteristics as compared to regular workhorse guidewires. Our data support this observation, as three-vessel CAD patients were older, had lower creatinine clearance, and were more likely to have multiple risk factors, previous CABG and clinically overt vascular disease elsewhere (analysis not shown). Finally, it should be noted that the proportion of patients undergoing PCI was no lower in cases that included physiological assessment than in those that did not. This is in line with prior observations from the POST-IT registry and goes against the common belief that the routine use of physiological assessment will reduce PCI rates, as reclassification between management strategies ultimately allows patients who would not otherwise have been treated to undergo PCI.14
Patient-independent determinants of adoption: impact of operator experience and scientific evidenceFor decades angiography has been the gold standard for guiding revascularization, and studies providing evidence for myocardial revascularization have been mostly based on angiography alone. It may thus not be surprising that older operators, who have been trained for many years in this technique, are less likely to use and rely on pressure gradients to decide on management of obstructive CAD. Unlike in previous reports, in which no difference in FFR use by operator age, practice setting, or case volume was observed,18 in our large dataset we demonstrate that younger interventionists were significantly more likely to use physiological assessment than older operators, regardless of any other significant determinants. This may be due to a variety of reasons, such as increased awareness of the limitations of angiography as a surrogate of lesion severity,34 changes in training patterns, and easier adoption of new technologies. For similar reasons, the penetration of physiological assessment could be expected to be related to the available clinical evidence. To assess this, we assessed its temporal relationship with scientific landmarks. All cases considered, there was a significant association with the publication of FAME 11 and the near-simultaneous release of the two-year results of FAME 213 and the 2014 European myocardial revascularization guidelines10 (Supplementary Figure S1B). Overall adoption appears to have been insensitive to the initial results of the FAME 2 study1 as well as to the publication of the two main randomized trials comparing iFR and FFR in clinical outcomes.3,4 Importantly, trends were similar across the main clinical settings, despite higher absolute penetration in stable CAD. Also, high adopters (all of whom belonged to younger age groups) followed (and possibly were the drivers of) the general trend (Figure 1 and Supplementary Figure S2).
The fact that adoption did not increase with the advent of adenosine-free and non-hyperemic indices (such as contrast FFR and iFR) deserves consideration. Additional reasons that have been implicated in the low use of FFR are adverse effects of hyperemic agents, the costs associated with adenosine, contraindications and patient-related discomfort,20 all of which have contributed to the pursuit of more patient-friendly techniques. In both DEFINE-FLAIR3 and iFR-SWEDEHEART4 the duration of the procedure was shorter and the percentage of patients who developed adverse procedure-related symptoms was lower than with FFR, potentially providing a solution for some of the previously reported barriers. Also, contrast-induced hyperemia has been shown to be an adequate surrogate of standard adenosine for FFR determination.35,36 Still, we provide clear evidence that these well-publicized improvements appeared to have had little, if any, impact on the adoption of invasive physiology. As overall rates remained stable, there was simply a larger proportion of cases using iFR, progressively driving FFR use down to less than 30% of invasive physiology cases toward the end of the study period (Figure 2). Whether or not this observation extends to other countries and practice environments, particularly in Europe, remains to be determined.
Finally, it is noteworthy that the time of day the procedure was performed during the regular workday independently affected the likelihood of pressure indices being incorporated in patient assessment, as it decreased by a significant 7% for every two hours throughout the day (Figure 4). This can be explained mainly by logistical factors, mostly in the cath lab setup and workflow, as well as by the team's own perceptions of potential unwarranted delays and added complexity to the procedures, despite improvements in the technique. Inherent limitations can and should be progressively overcome by increasing operator experience and improving cath labs’ routines and logistics, given that such measures are justified by important factors such as reduced need for further testing14 and possibly unnecessary coronary interventions. Also, it is reasonable to expect that technical improvements in pressure sensor-tipped guidewires, continuous education in coronary physiology, and successful implementation of emerging technologies, such as real-time angiography and non-invasive CCTA-derived FFR and virtual PCI planning, may overcome some of these hurdles and help to change the scenario in the near future.
Strengths and limitationsDespite the high number of procedures, encompassing a wide range of clinical indications, our data were obtained from only two large-volume centers, and it could be argued that these may not be representative of the situation in the entire country. However, based on the Portuguese Registry on Interventional Cardiology, the rate of FFR-guided PCI was in the range of 0.2-0.8% before 2009, rising to 2.6-3.1% in 2010-2012.37 These estimates mirror our results in that same period, which is a reassuring confirmation of the external validity of our data.
The full spectrum of reasons underlying the low adoption of invasive physiology is difficult to ascertain and there is no bullet-proof methodology that could provide unequivocal answers. A prospective inquiry on why invasive physiology may or may not have been used in any given case could induce observation bias and unwarranted changes in usual practice. On the other hand, a retrospective approach, such as the one used in our study, necessarily relies on the quality of registry data, a limitation that is inherent to all observational studies. However, we provide an unbiased analysis based on variables that are easy to collect and report and thus potentially less prone to uncertainty. Accurate identification of the original reasons underlying low adoption rates should prompt the implementation of dedicated strategies, in each specific setting.
ConclusionThis study builds on the evidence concerning the suboptimal use of invasive physiological assessment in routine practice, which is due in part to issues unrelated to patient and procedural characteristics. The availability of adenosine-free pressure indices has not increased adoption. In order to improve patient outcomes, dedicated strategies are needed both to motivate adherence to current guidelines and to increase awareness of the advantages of integrating invasive functional information into management algorithms.
FundingThis analysis has received no funding.
Conflicts of interestDr. Raposo has received grants from Abbott, Volcano, and HeartFlow, has served as a member of advisory boards for Abbott and Boston Scientific, and has received personal fees from Abbott, Boston Scientific, and HeartFlow outside the submitted work.
Dr. Baptista has received grants from Abbott, Volcano, and HeartFlow, has served as a member of advisory boards for Abbott, Boston Scientific and Opsens Medical, and has received personal fees from Abbott, Boston Scientific, and HeartFlow outside the submitted work.
Dr. Teles has received grants from Abbott, and has served as a member of advisory boards for Abbott, Medtronic and Boston Scientific.
The other authors have no conflict of interests to declare.
The authors wish to acknowledge the invaluable contributions of Paulo Leal regarding data acquisition and management, and John Henderson for statistical consultancy.
In the online supplementary material, a detailed description of the uniform criteria used for the definition of each clinical indication is provided. Also, additional figures are available that further address temporal trends, as well as the relationship between adoption and non-invasive baseline testing and coronary artery disease burden.