The GRACE and TIMI scores have been well validated for assessment of prognosis in non-ST-elevation acute coronary syndrome (NSTE-ACS). However, their value in predicting coronary artery disease (CAD) has been little studied. We aimed to assess the relationship between these scores and the extent of coronary disease.
MethodsWe analyzed 238 consecutive patients admitted for NSTE-ACS and undergoing a coronary angiogram during hospitalization. The severity of CAD was assessed using the SYNTAX score. Obstructive CAD was defined as ≥50% stenosis in the left main or ≥70% stenosis in other vessels. Severe CAD was defined as a SYNTAX score >32. The Pearson test was used to assess the correlation between scores.
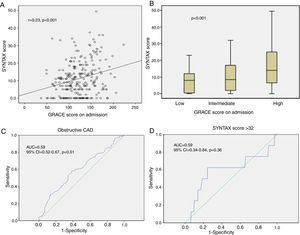
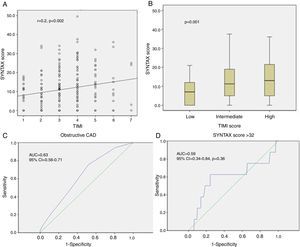
ResultsThe SYNTAX score was higher in patients at high risk (GRACE score: p<0.001 and TIMI score: p=0.001). Moreover, there was a significant positive correlation between the GRACE and SYNTAX scores (r=0.23, p<0.001) as well as between TIMI and SYNTAX (r=0.2, p=0.002). Both clinical scores can predict obstructive CAD moderately well (area under the curve [AUC] for GRACE score: 0.599, p=0.015; TIMI score: AUC 0.639, p=0.001) but not severe disease. A GRACE score of 120 and a TIMI score of 2 were predictive of obstructive CAD with, respectively, a sensitivity of 57% and 75.7% and a specificity of 61.8% and 47.9%.
ConclusionThe GRACE and TIMI scores correlate moderately with the extent of coronary disease assessed by the SYNTAX score. They can predict obstructive CAD but not severe disease.
Os scores GRACE e TIMI foram convenientemente validados na avaliação do prognóstico de síndrome coronária aguda sem elevação do segmento-ST (NSTE-ACS). No entanto, o seu valor na previsão de doença coronária (DC) está mal estudado. O nosso objetivo é avaliar a relação entre esses scores e a extensão da doença coronária.
MétodosForam consecutivamente avaliados 238 doentes admitidos para NSTE-ACS e submetidos a angiografia coronária durante o internamento. A gravidade da DC foi avaliada durante o score Syntax. Definimos DC obstrutiva quando a obstrução da DC é ≥ 50% no tronco comum e ≥ 70% nos outros vasos. Uma DC grave é definida por um score syntax >32. O teste Pearson foi usado para avaliar a correlação entre os scores.
ResultadosO valor do score Syntax foi superior nos doentes de alto risco (escore GRACE: p<0,001 e o score TIMI: p=0,001). Além disso, houve uma correlação significativa positiva entre os scores GRACE e Syntax (r=0,23, p<0,001), assim como entre os scores TIMI e Syntax (r=0,2, p=0,002). Ambos os scores clínicos podem de certo modo prever DC obstrutiva (score GRACE: AUC=0,599 (p=0,015); score TIMI: AUC=0,639 (p=0,001), mas não uma doença grave. Um score GRACE=120 e um score TIMI=2 foram fatores preditores da DC obstrutiva com uma sensibilidade de 57% e de 75,7% respetivamente e uma especificidade de 61,8% e de 47,9%.
ConclusãoOs scores GRACE e TIMI estão ligeiramente correlacionados com a extensão da doença coronária avaliada pelo score Syntax. Podem prever uma DC obstrutiva, mas não uma doença grave.
Given the wide spectrum of risk for death and recurrent events among patients with non-ST-elevation acute coronary syndrome (NSTE-ACS), risk stratification has become the cornerstone of management of this entity. American and European clinical guidelines recommend the use of the Global Registry for Acute Coronary Events (GRACE) or the Thrombolysis in Myocardial Infarction (TIMI) risk scores for risk assessment1–3; however, these scores are not intended to predict the extent and severity of coronary artery disease (CAD). Assessing the coronary anatomy before performing coronary angiography may change the therapeutic decision, including the timing and intensity of interventions, and could even avoid an invasive strategy in patients in whom no obstructive coronary disease is predicted; conversely, if the scores could better identify patients with extensive disease (SYNTAX score >32), it would be possible to avoid the administration of aggressive antiplatelet therapy that would increase the risk of bleeding in the event of emergent surgery. Few studies have analyzed the correlation between prognostic risk scores and coronary anatomy, and their results were disparate. A large number of scoring systems and laboratory parameters are used in this context in clinical practice. The SYNTAX score is a system for determining the extent and severity of CAD but has seldom been used for this purpose.4 Therefore, we sought to determine the accuracy of the GRACE and TIMI scores in predicting angiographic data in patients admitted with NSTE-ACS and to analyze the correlation of clinical risk scores with the angiographic extent and severity of CAD as assessed by the SYNTAX score.
MethodsWe included all patients admitted to our department between January 2014 and December 2014 with a diagnosis of NSTE-ACS. NSTE-ACS was defined as acute chest pain without persistent ST-segment elevation. Electrocardiogram (ECG) changes could include transient ST-segment elevation, persistent or transient ST-segment depression, T-wave inversion, flat T waves or T-wave pseudo-normalization, or the ECG could be normal. The level of conventional troponin could be positive, with a dynamic rise or fall (non-ST-elevation myocardial infarction), or normal (unstable angina).
We excluded patients with ST-elevation myocardial infarction, new left bundle branch block on the ECG, and chest pain of proven non-ischemic etiology (such as takotsubo syndrome or myocarditis), after coronary angiography and magnetic resonance imaging.
Since we aimed to investigate the relationship between clinical risk scores and the extent of native vessel disease, and the SYNTAX score was originally developed for native CAD, we also excluded patients with prior surgical or percutaneous revascularization.
Although this was a retrospective study, for each patient the original GRACE and TIMI scores at admission were recalculated based on their medical records.3 The tertiles of risk categories used were: for in-hospital mortality, low risk for GRACE score ≤108, intermediate risk for GRACE score between 109 and 140, and high risk for GRACE score ≥141. For the TIMI score, the risk is considered low for TIMI score ≤3, intermediate for TIMI score <5 and high for TIMI score ≥5.
All coronary angiograms were visually assessed by two experienced invasive cardiologists who were blinded to all other clinical data; each cardiologist calculated the SYNTAX score for each patient and the mean of the two calculated values was used in the analysis. In categorical terms, obstructive CAD was defined as ≥50% stenosis in the left main or ≥70% stenosis in other vessels. Patients with a SYNTAX score >32 were considered as presenting severe coronary disease.
Statistical analysisData analysis was performed using IBM SPSS version 21. Frequencies and percentages were computed for categorical variables. Qualitative variables were compared using the chi-square test, or Fisher's exact test when the conditions of validity of the chi-square test were not fulfilled.
The normality of distribution of quantitative variables was assessed by calculating kurtosis and skewness coefficients and by the Kolmogorov-Smirnov test. Comparisons were made using the Student's t test for normal distributions, otherwise the Mann-Whitney test was used. Multivariate analysis was performed by binary logistic regression. All variables were assessed with p<0.2.
The correlation between two quantitative variables was assessed using Pearson's correlation test. The correlation coefficient was considered weak if <0.5, moderate if between 0.5 and 0.7 and strong if >0.7.
Receiver operating characteristic (ROC) curves were used to determine the predictive accuracy of the risk scores regarding obstructive and severe (SYNTAX score >32) CAD. Prediction was deemed to be significant when the area under the ROC curve (AUC) was statistically different from 0.5.
A p value <0.05 was considered statistically significant.
ResultsPopulation characteristicsDuring the study, 390 patients were admitted to our department for suspected NST-ACS, but 78 of them had a history of prior revascularization, and another cause of chest pain was determined in 74 patients. Thus, our sample included 238 patients, with a mean age of 61 years and a predominance of male gender (male/female ratio 1.73). Hypertension, smoking and diabetes were found in 62%, 51% and 47% of our patients, respectively.
On admission, 31% of the patients were identified as low-risk according to the TIMI score and 36% according to the GRACE score, 52% were identified as intermediate-risk according to the TIMI score and 35% according to the GRACE score, and 17% were identified as high-risk according to the TIMI score and 29% according to the GRACE score. Only 127 patients (53.3%) were classified in the same risk category according to both scores.
Analysis of coronary angiograms showed that 31% of patients had no obstructive coronary disease. Three-vessel disease was identified in 23.1% of the sample and left main obstructive disease in 30.2% of our patients. The mean SYNTAX score was 11.18±9, with a normal distribution.
The majority of the population had a low SYNTAX score (<22) (85.3%); few patients had a SYNTAX score between 22 and 32 (11.3%) and only 3.4% had a SYNTAX score >32.
Patients with obstructive CAD were more frequently male and were significantly more likely to have diabetes. The percentages of diabetes and troponin elevation and higher TIMI and GRACE scores were significantly greater in patients with obstructive CAD compared to other patients (Table 1). In multivariate analysis, predictors of obstructive CAD were male gender (odds ratio [OR] 3.24, 95% confidence interval [CI] 1.68-6.27, p<0.001), diabetes (OR 3.408, 95% CI 1.73-6.7, p<0.001) and troponin elevation (OR 7.19, 95% CI 3.7-13.9, p<0.001). TIMI and GRACE scores were not included in the multivariate analysis as they are not independent variables.
Univariate analysis of predictors of obstructive coronary disease in patients with non-ST-elevation acute coronary syndrome.
| Non-obstructive CAD (n=73) | Obstructive CAD (n=165) | p | |
|---|---|---|---|
| Gender | |||
| Female (n=87) | 37 (42.5%) | 50 (57.5%) | 0.003 |
| Male (n=151) | 36 (23.8%) | 115 (76.2%) | |
| Mean age (years) | 59.63±11.64 | 61.48±12.26 | 0.277 |
| Age | |||
| <40 years (n=9) | 2 (22.2%) | 7 (77.8%) | 0.575 |
| ≥40 years (n=229) | 71 (31%) | 158 (69%) | |
| Diabetes | |||
| Yes (%) | 27 (23.7%) | 87 (76.3%) | 0.025 |
| No (%) | 46 (37.1%) | 78 (62.9%) | |
| Hypertension | |||
| Yes (%) | 43 (28.3%) | 109 (71.7%) | 0.28 |
| No (%) | 30 (34.9%) | 56 (65.1%) | |
| CRF | |||
| Yes (%) | 2 (15.4%) | 11 (84.6%) | 0.35 |
| No (%) | 71 (31.6%) | 154 (68.4%) | |
| Killip class | |||
| 67 (32.7%) | 138 (67.3%) | 0.1 | |
| ≥II (%) | 6 (18.1%) | 27 (81.9%) | |
| SBP (mmHg) | 133.60±20.56 | 135.54±24.09 | 0.59 |
| HR (bpm) | 77.75±20.34 | 78.16±18.82 | 0.882 |
| ECG | |||
| Normal (%) | 19 (35.8%) | 34 (64.2%) | 0.356 |
| Abnormal (%) | 54 (29.2%) | 131 (70.8%) | |
| Troponin | |||
| Positive (%) | 25 (17.1%) | 121 (82.9%) | 0.001 |
| Negative (%) | 48 (52.2%) | 44 (47.8%) | |
| Prognostic scores | |||
| TIMI | 2.77±1.33 | 3.45±1.35 | 0.001 |
| TIMI ≥5 | 8 (19.5%) | 33 (80.5%) | 0.089 |
| GRACE | 114.22±32.4 | 126.60±34.3 | 0.010 |
| GRACE ≥140 | 13 (19.1%) | 55 (80.9%) | 0.014 |
| CrCl (ml/min) | 92.14±28.94 | 89.30±45.39 | 0.624 |
| Hemoglobin (g/dl) | 12.88±1.46 | 12.90±1.89 | 0.963 |
| Blood glucose (g/dl) | 7.70±4.3 | 9.35±4.89 | 0.013 |
| Troponin (μg/l)a | 1.40±5.77 | 4.88±11.06 | p<0.001 |
| LVEF (%) | 55.82±9.8 | 53.34±10.04 | 0.078 |
bpm: beats per min; CrCl: creatinine clearance; CRF: chronic renal failure; ECG: electrocardiogram; HR: heart rate; LVEF: left ventricular ejection fraction; SBP: systolic blood pressure.
Comparing patients with SYNTAX score >32 vs. ≤32, no significant difference was found with regard to the mean TIMI score, but the GRACE score was significantly higher in the first group (Table 2).
Univariate analysis of predictors of severe coronary disease (SYNTAX score >32) in patients with non-ST-elevation acute coronary syndrome.
| SYNTAX ≤32 (n=230) | SYNTAX >32 (n=8) | p | |
|---|---|---|---|
| Age (years) | 60.90±12.13 | 61.25±11.39 | 0.9 |
| Female gender | 86 (37.4%) | 1 (12.5%) | 0.26 |
| Diabetes (%) | 109 (47.4%) | 5 (62.5%) | 0.63 |
| Hypertension (%) | 147 (63.9%) | 5 (62.5%) | 1 |
| Dyslipidemia (%) | 81 (35.2%) | 1 (12.5%) | 0.26 |
| Smoking | 117 (50.9%) | 6 (75%) | 0.32 |
| CRF | 13 (5.6%) | 0 (0%) | 1 |
| Killip class >II (%) | 7 (3.04%) | 0 (0%) | 1 |
| SBP (mmHg)a | 134.99±23.25 | 133.75±16.85 | 0.95 |
| HR (bpm)a | 78.04±19.09 | 77.75±25.13 | 0.65 |
| ST-segment depression | 84 (36.5%) | 4 (50%) | 0.47 |
| CrCl (ml/min)a | 90.87±41.36 | 70.05±22.32 | 0.08 |
| Hemoglobin (g/dl)a | 12.90±1.77 | 12.70±0.96 | 0.46 |
| Blood glucosea | 8.76±4.7 | 11.41±6.1 | 0.16 |
| Troponina | 3.77±9.9 | 4.89±9.2 | 0.5 |
| LVEF (%)a | 54.37±9.9 | 46.25±9.5 | 0.017 |
| TIMI (mean) | 3.22±1.37 | 3.88±1.55 | 0.23 |
| GRACE (mean) | 122.48±33.86 | 132±43.18 | 0.045 |
bpm: beats per min; CrCl: creatinine clearance; CRF: chronic renal failure; HR: heart rate; LVEF: left ventricular ejection fraction; SBP: systolic blood pressure.
In multivariate analysis, the only predictive factor for severe CAD (SYNTAX score >32) was left ventricular ejection fraction (LVEF) (OR 0.93, 95% CI 0.88-0.99, p=0.032).
Correlation between clinical prognostic scores and coronary artery diseaseGRACE scoreBy Pearson's correlation test, there was a positive correlation between the GRACE and SYNTAX scores, but it was weak (r=0.23, p<0.001) (Figure 1A). Patients at low risk according to the GRACE score were more likely to have non-obstructive CAD (p<0.001), while patients at high risk more frequently had three-vessel disease (p=0.007) (Table 3). SYNTAX score values were significantly different between the tertiles of GRACE scores (p<0.001) (Figure 1B) and were especially high in patients at high risk compared to those at low risk (p<0.001) or at intermediate risk (p<0.001). However, there was no statistical difference between the low-risk and the intermediate-risk groups (p=0.68).
Role of the GRACE score in predicting angiographic data during non-ST-elevation acute coronary syndrome. (A) Small correlation between GRACE score and SYNTAX score (r=0.23; p<0.001); (B) comparison of SYNTAX score values between tertiles of the GRACE score, with statistically significant association (p<0.001); (C) area under the curve of the GRACE score for detecting obstructive coronary artery disease, indicating diagnostic accuracy; (D) area under the curve of the GRACE score for detecting severe coronary artery disease (SYNTAX score >32), showing no diagnostic accuracy. AUC: area under the curve; CAD: coronary artery disease; CI: confidence interval.
Comparison of angiographic data between tertiles of the GRACE score.
| Low GRACE score (n=84) | Intermediate GRACE score (n=86) | High GRACE score (n=68) | p | |
|---|---|---|---|---|
| Non-obstructive CAD (n=73) | 33 (39.28%) | 28 (32.56%) | 12 (17.64%) | 0.014 |
| One-vessel disease (n=64) | 24 (28.57%) | 24 (27.91%) | 16 (23.53%) | 0.759 |
| Two-vessel disease (n=46) | 14 (16.67%) | 18 (20.93%) | 14 (20.58%) | 0.746 |
| Three-vessel disease (n=55) | 13 (15.48%) | 16 (18.60%) | 26 (38.23%) | 0.002 |
| Left main disease (n=72) | 19 (26.4%) | 31 (43.1%) | 22 (30.6%) | 0.14 |
| SYNTAX score | 8.76±7.08 | 9.94±8.49 | 15.74±11.4 | <0.001 |
CAD: coronary artery disease.
Using ROC curves, we showed that the GRACE score is accurate for predicting obstructive CAD (AUC 0.599, 95% CI 0.52-0.67, p=0.015) (Figure 1C). A GRACE score of 120 was identified as the optimal cut-off to predict obstructive CAD, with a sensitivity of 57% and specificity of 61.6%, a positive predictive value (PPV) of 77% and a negative predictive value (NPV) of 38.8% (p=0.008). However, the GRACE score was not accurate for predicting patients with severe CAD, defined as SYNTAX score >32 (AUC 0.594, 95% CI 0.34-0.86, p=0.36) (Figure 1D).
TIMI scoreThere was a positive correlation between TIMI and SYNTAX scores, but it was also weak (r=0.2; p=0.002) (Figure 2A). Patients at low risk according to the TIMI score were more likely to present non-obstructive CAD (p<0.001), while patients at high risk more frequently had three-vessel disease (p=0.007) (Table 4). SYNTAX scores were significantly different between the TIMI score tertiles (p=0.001) (Figure 2B). The SYNTAX score was significantly lower in patients at low risk compared to those at intermediate risk (p=0.005) and to those at high risk (p=0.019); but there were no significant differences between patients at intermediate and at high risk with regard to TIMI score (p=0.93).
Role of the TIMI score in predicting angiographic data during non-ST-elevation acute coronary syndrome. (A) Small correlation between TIMI score and SYNTAX score (r=0.23; p<0.001); (B) comparison of SYNTAX score values between the tertiles of the TIMI score, with statistically significant association (p<0.001); (C) area under the curve of the TIMI score for detecting obstructive coronary artery disease, showing diagnostic accuracy; (D) area under the curve of the TIMI score for detecting severe coronary artery disease (SYNTAX score >32), showing no diagnostic accuracy. AUC: area under the curve; CAD: coronary artery disease; CI: confidence interval.
Comparison of angiographic data between TIMI score tertiles.
| Low TIMI score (n=75) | Intermediate TIMI score (n=122) | High TIMI score (n=41) | p | |
|---|---|---|---|---|
| Non-obstructive disease (n=73) | 36 (48%) | 31 (25.4%) | 6 (14.63%) | p<0.001 |
| One-vessel disease (n=64) | 19 (25.33%) | 33 (27.05%) | 12 (29.27%) | 0.901 |
| Two-vessel disease (n=46) | 11 (14.67%) | 27 (22.15%) | 8 (19.51%) | 0.439 |
| Three-vessel disease (n=55) | 9 (12%) | 31 (25.4%) | 15 (36.59%) | 0.007 |
| Left main disease (n=72) | 16 (22.2%) | 43 (59.7%) | 13 (18.1%) | 0.117 |
| SYNTAX score | 8.08±7.5 | 12.4±10.15 | 13.07±10.2 | 0.001 |
The TIMI score was also validated for predicting obstructive CAD (AUC 0.639, 95% CI 0.56-0.71, p=0.001) (Figure 2C). We identified a TIMI score of 2 as the optimal cut-off for obstructive CAD, with a sensitivity of 75.7% but a low specificity (47.9%), PPV of 76.7% and NPV of 46.67% (p<0.001). Paradoxically, the TIMI score did not predict patients with SYNTAX score >32 (AUC 0.62, 95% CI 0.41-0.82, p=0.25) (Figure 2D).
DiscussionThe TIMI and GRACE scores have been thoroughly validated for assessing prognosis in NSTE-ACS, based on registries and large trials.5–8 The TIMI score was derived from data on 1957 patients with acute coronary syndrome (ACS) participating in two large double-blind, randomized clinical trials: Thrombolysis in Myocardial Infarction (TIMI) 11B 8and Efficacy and Safety of Subcutaneous Enoxaparin in Unstable Angina and Non-Q-Wave MI (ESSENCE).9 This score has been validated in the short term and several studies have established its value in the long term.
The GRACE score is also validated and is more effective for assessing clinical risk. Developed from the multinational Global Registry of Acute Coronary Events (GRACE) registry including 17412 patients from 94 hospitals in 14 countries, it assesses prognosis at admission and at six months.10
These two scores are used to identify patients at high risk of coronary events in the context of NST-ACS. Various studies have shown that angiographic disease is a predictor of coronary events in the short and long term for patients with ACS. We therefore sought correlations between prognostic scores and the extent of angiographic disease, and also set out to determine cut-offs of TIMI and GRACE scores that were predictive of non-obstructive CAD. The aim was to avoid an invasive strategy below this cut-off or, conversely, to consider a more aggressive approach for patients whose prognostic score indicates severe angiographic disease. Previous studies have been limited to demonstrating an association between the TIMI or GRACE scores and the number of arteries affected. In our study we set out to assess the extent of CAD quantitatively using the SYNTAX score.11–15
We showed that diabetes (OR 3.4) and troponin elevation (OR 7.1) are strong predictors of obstructive CAD and that TIMI and GRACE scores are significantly higher in patients with significant coronary lesions. These two scores were not assessed in multivariate analysis because they include many factors which are dependent and hence cannot be included in a logistic regression model. However, it is not surprising to find an association between clinical prognostic scores and obstructive disease, considering that predictors indicating unfavorable coronary anatomy are part of both GRACE and TIMI scores.
In a cohort including 406 patients with NSTE-ACS, Mahmood et al.16 showed that a TIMI score >4 and an admission GRACE score >133 were significantly associated with three-vessel disease and left main disease, while TIMI score ≤4 and GRACE score ≤133 were associated with normal arteries or non-obstructive CAD (p<0.01). The authors used C-statistics to assess the accuracy of both scores for predicting angiographic disease, which gave values between 0.56 and 0.65 for the TIMI score and between 0.57 and 0.72 for the GRACE score for the range of different lesions, showing that the GRACE score had better discriminatory accuracy.
In a study by Khandelwal et al.,17 there was a moderate positive correlation between the GRACE score and the modified Gensini Score (r=0.3), whereas the PURSUIT (r=0.274) and TIMI scores (r=0.166) showed only a weak positive correlation. Barbosa et al.18 also demonstrated a positive but weak correlation between the TIMI and GRACE scores on the one hand and the Gensini score on the other (r<0.3). However, the degree of this association was not sufficient to make these scores accurate predictors of coronary angiography results. The authors explained these findings by the fact that the anatomic extent of CAD is one feature of severe CAD.
The correlation between the Gensini and GRACE scores was also assessed in patients with ST-elevation ACS.19 Gensini score values were significantly different (p=0.006) between low-, intermediate- and high-risk groups according to the GRACE score, but the correlation coefficient between the two scores was weak (r=0.17, p=0.04).
The Gensini score is based on three parameters: number of lesions, proximal or distal location of each lesion, and degree of stenosis. For example, a patient with 70% stenosis of the proximal left anterior descending (LAD) artery would have a Gensini score of 10, but could have suffered myocardial infarction with severe left ventricular dysfunction. Moreover, the Gensini score does not take into consideration the thrombotic features of the lesion.
Bekler et al.20 analyzed the relationship between the GRACE and TIMI scores and severity of CAD as assessed by the SYNTAX score, in patients with ACS (ST-elevation and non-ST-elevation myocardial infarction). They concluded that there was a significant positive correlation between the GRACE and SYNTAX scores, but not between TIMI and SYNTAX, and suggested that some parameters which are not included in the TIMI score, including age, heart rate, and systolic blood pressure, are predictors of the extent and severity of CAD. In addition, in this study there were significant differences in admission glucose levels and the neutrophil/lymphocyte ratio between the GRACE risk groups, but not between the TIMI risk groups; these factors have recently been demonstrated to be predictive of poor prognosis and severe angiographic disease in patients with ACS.21,22
In our study, we chose to use the SYNTAX score, which is more detailed than the Gensini score and takes into consideration many features, including thrombus, calcification, tortuosity, and others. We found that patients at high risk, according to either GRACE or TIMI, have a higher SYNTAX score, but the correlations between the clinical scores and SYNTAX score are weak (r=0.23 for GRACE, and r=0.2 for TIMI). Nevertheless, the accuracy of the clinical scores for predicting obstructive CAD was demonstrated by the ROC curves. We also determined predictive thresholds of obstructive CAD for the TIMI and GRACE scores, with an acceptable positive predictive value for both scores (PPV >75%), but with a low NPV.
This result can be explained by the fact that some factors which emerged as predictive of obstructive CAD in our study are not included in the clinical scores (male gender and elevated blood glucose for both scores, troponin elevation for the TIMI score), and if these parameters are added to the scores, this will certainly improve their PPV. Conversely, many parameters included in these scores were not predictors of obstructive CAD in our study, and this reduced the discriminatory power of these scores in our population.
The second objective of our work was to assess the discriminatory value of clinical scores for predicting severe CAD. Beigel et al.23 aimed to identify predictors of the angiographic extent and severity of CAD in patients with NSTE-ACS undergoing early angiography, defining high-risk coronary anatomy (HRCA) as left main disease >50%, proximal LAD lesion >70%, or two- or three-vessel disease involving the LAD. In their study, peripheral vascular disease (OR 1.88, 95% CI 1.62-5.80, p<0.001) and a GRACE score of >140 (OR 1.88, 95% CI 1.29-2.75, p<0.001) were the strongest predictors of HRCA. These patients fared worse compared with those with low-risk anatomy. Finally, the authors suggested that predictors of HRCA should be included in the risk stratification of patients with NSTE-ACS.
Barbosa et al.18 found a weak association between the Gensini and GRACE (r=0.23, p=0.017) and TIMI scores (r=0.27, p=0.02). The GRACE score predicted neither obstructive CAD (AUC 0.57; 95% CI 0.46-0.69) nor severe CAD (AUC 0.59; 95% CI 0.48-0.70). Surprisingly, the TIMI score proved to be a modest predictor of CAD (AUC 0.65; 95% CI 0.55-0.76) and of severe CAD (AUC 0.66; 95% CI 0.56-0.76). The authors concluded that the correlation of the GRACE and TIMI scores with the Gensini score is not sufficient to make these scores accurate predictors of coronary angiography results.
Cakar et al.11 demonstrated that the GRACE score has significant value for assessing the severity and extent of coronary artery stenosis as assessed by the Gensini score (r=0.189, p=0.03). They also showed that GRACE has discriminatory value in predicting left main disease (AUC 0.65; 95% CI 54-76, p=0.012) as well as in predicting multivessel disease (AUC 0.72; 95% CI 64-80, p=0.001).
In our study, patients at high risk more frequently had multivessel disease, but the GRACE and TIMI scores were not validated to predict severe CAD (SYNTAX score >32). In fact, the only predictor of a SYNTAX score >32 was LVEF, but this parameter is not included in either score.
ConclusionOur study shows a modest correlation between clinical scores (TIMI and GRACE) and the angiographic SYNTAX score. Other trials have instead demonstrated a correlation with the Gensini score or were limited to correlations with the number of diseased vessel. We demonstrated that the GRACE and TIMI scores are moderately correlated with the extent of CAD as assessed by the SYNTAX score. They are accurate for predicting obstructive CAD but not severe disease.
Conflicts of interestThe authors have no conflicts of interest to declare.