Concerns surrounding the consequences of ionizing radiation (IR) have increased in interventional cardiology (IC). Despite this, the ever-growing complexity of diseases as well as procedures can lead to greater exposure to radiation. The aim of this survey, led by Portuguese Association of Interventional Cardiology (APIC), was to evaluate the level of awareness and current practices on IR protection among its members.
MethodsAn online survey was emailed to all APIC members, between August and November 2021. The questionnaire consisted of 50 questions focusing on knowledge and measures of IR protection in the catheterization laboratory. Results were analyzed using descriptive statistics.
ResultsFrom a response rate of 46.9%, the study obtained a total sample of 159 responses (156 selected for analysis). Most survey respondents (66.0%) were unaware of the radiation exposure category, and only 60.4% reported systematically using a dosimeter. A large majority (90.4%) employed techniques to minimize exposure to radiation. All participants used personal protective equipment, despite eyewear protection only being used frequently by 49.2% of main operators. Ceiling suspended shields and table protectors were often used. Only two-thirds were familiar with the legally established limit on radiation doses for workers or the dose that should trigger patient follow-up. Most of the survey respondents had a non-certified training in IR procedures and only 32.0% had attended their yearly occupational health consultation.
ConclusionsSafety methods and protective equipment are largely adopted among interventional cardiologists, who have shown some IR awareness. Despite this, there is room for improvement, especially concerning the use of eyewear protection, monitoring, and certification.
A preocupação com as consequências da radiação ionizante tem vindo a crescer na cardiologia de intervenção. O objetivo da Associação Portuguesa de Cardiologia Interventiva (APIC) foi avaliar o nível de sensibilização e práticas atuais na proteção contra a radiação ionizante.
MétodosUm inquérito voluntário foi enviado por e-mail aos membros da APIC, entre Agosto-Novembro de 2021, que consistiu em 50 questões relativas ao conhecimento e medidas de proteção contra a radiação. Posteriormente foi efetuada a respetiva análise descritiva.
ResultadosObtiveram-se 159 respostas (46,9% do inquérito enviado) - 156 foram consideradas adequadas para análise. A maioria (66,0%) desconhecia a categoria de exposição à radiação correspondente e apenas 60,4% utilizaram o dosímetro de forma sistemática. 90,4% dos inquiridos utilizaram técnicas para minimizar a exposição à radiação. Praticamente todos os participantes utilizaram equipamento de proteção individual, mas a proteção ocular apenas ocorreu de forma frequente em 49,2% dos operadores principais. Escudos de teto e protetores de mesa foram os materiais disponíveis mais utilizados. Apenas dois terços conheciam a dose limite legalmente estabelecida para os trabalhadores ou a dose que deve desencadear um acompanhamento do paciente. A maioria dos inquiridos tinha uma formação não certificada em radiação ionizante e apenas 32,0% tiveram consulta anual de medicina do trabalho.
ConclusõesA consciencialização e as práticas adotadas para proteção contra radiação ionizante têm vindo a aumentar entre os profissionais de cardiologia de intervenção. Ainda assim, existe espaço para melhorar, nomeadamente no uso da proteção ocular, necessidade de monitoração e certificação.
Interventional cardiology (IC) has witnessed impressive evolution over the last 20 years, both due to improvements in knowledge of coronary heart disease, but also linked to newer and more modern techniques and equipment. Exposure to ionizing radiation (IR), projected through fluoroscopy/cinefluorography is a consequence of the improvements in minimally invasive techniques in cardiac procedures.1
Initially, these procedures had mainly diagnostic purposes, exposing patients to a minimum radiation time. The goal over several years was to improve imaging quality, and thereby increase radiation intensity.2 In the last 10 years, the concern regarding the consequences of IR has increased, as the incidence of adverse reactions and stochastic effects rose, leading to the publication of international guidelines on radiological protection during medical procedures.3–6
Modern equipment enables better image quality with less exposure to IR, by maximizing equipment technology features. Notwithstanding this, alongside technological innovation, procedures became more complex and mostly therapeutic; for example, coronary chronic total occlusions (CTO) with consequent greater exposure to IR. Thus, the focus on the complexity of the disease and intervention may overshadow the required measures that must be instituted in order to reduce exposure.2,7
The concern over patient exposure to IR is notorious among interventional cardiologists. Radiation doses in clinical practice have become a target of great interest. Unlike patients, the catheterization laboratory (Cath-Lab) team is constantly exposed to radiation, but surprisingly only a few Cath-Labs report their IR data.7–10
Interventional cardiologists should work towards implementing novel methods for IR protection, ensuring controlled exposure in order to reduce the deleterious effects in the short- and the long term, for both patients and professionals.11,12
This survey aimed to evaluate the awareness of IC health professionals regarding IR, its deleterious effects on patients and Cath-Lab team, as well as to understand the current practices concerning ionizing radiation protection.
ObjectivesThe aim of this survey, developed by the Portuguese Association of Interventional Cardiology (APIC), was to evaluate the level of awareness and current practices regarding IR protection.
MethodsSurveyA voluntary and anonymous questionnaire (Supplement S1) was emailed to all registered APIC members between August and November 2021. The questionnaire consisted of 50 questions, including demographics as well as four main topics: knowledge surrounding IR; techniques and methods used to minimize exposure to IR; equipment used to protect against IR; awareness/prevention on the effects of IR. Inclusion criteria were being an active member of APIC, and currently employed in an IC role. For the purpose of this study, the IC team was composed of the following members: main operator – interventional cardiologist who performs the procedures as the first operator; assistant operator – interventional cardiologist/interventional cardiology fellow/cardiology fellow or cardiorespiratory technician/nurse who is an intervention assistant on the intervention table; room assistant – cardiorespiratory or radiology technician/nurse whose function is to assist the team that is on the intervention table (for example as a circulating nurse or scrub assistant).
Data analysisData were cleaned and a descriptive analysis was subsequently performed. Categorical variables are presented as frequencies and percentages, and continuous variables as means and standard deviations, or medians and interquartile ranges for variables with skewed distribution or a significant Shapiro–Wilk test. Statistical analysis was performed with SPSS Inc., Chicago, IL, USA, version 21.0.
ResultsThe questionnaire was emailed to a total of 329 APIC members (186 were effective associates – medical specialists, 85 aggregate associates – residents, and 58 affiliates – non-physicians). All active members have a registered email in APIC's mailing list. A total of 159 completed surveys were returned (46.9%). Two questionnaires were excluded as they did not consent to publishing their responses, whereas another was excluded as they did not currently work in a Cath-Lab. The final sample was thus composed of 156 participants. At the time, 85 IC subspecialists were registered in the Association of Medical Doctors of Portugal (Ordem dos Médicos – https://ordemdosmedicos.pt/estatisticas-nacionais/#1505070622822-9e31b1b1-6d1a).
DemographicsMost of the survey respondents were male (81 of 156, 51.9%), aged between 30 and 49 years (62.2%). Physicians were the most represented class, accounting for 67 of 156 (42.9%), from which 61 (39.1%) were main operators (only six doctors were considered assistant operators). Radiation exposure reflected by a higher time experience in Cath-Lab for over 20 years was present in 49 (31.4%) participants. Most responses were from professionals based in the Greater Lisbon area (63 of 156, 40.4%), although all regions were represented (Table 1).
Demographic characteristics, occupation, years of radiation exposure and distribution by region of the survey respondents.
| Age | |||
|---|---|---|---|
| <40 years(n=60, 38.5%) | ≥40 years(n=96, 61.5%) | Total (n=156) | |
| Gender | |||
| Male, n (%) | 29 (48.3) | 52 (54.2) | 81 (51.9) |
| Female, n (%) | 31 (51.7) | 44 (45.8) | 75 (48.1) |
| Occupation | |||
| Doctor, n (%) | 27 (45.0) | 40 (41.7) | 67 (42.9) |
| Nurse, n (%) | 19 (31.7) | 17 (17.7) | 36 (23.1) |
| Cardiorespiratory technician, n (%) | 5 (8.3) | 11 (11.5) | 16 (10.3) |
| Radiographer, n (%) | 9 (15.0) | 28 (29.2) | 37 (23.7) |
| Operator role | |||
| Main operator, n (%) | 21 (35.0) | 40 (41.7) | 61 (39.1) |
| Assistant operator, n (%) | 22 (33.6) | 17 (17.7) | 39 (25.0) |
| Room assistant, n (%) | 17 (28.3) | 39 (40.6) | 56 (35.9) |
| Professional experience in Cath-Lab | |||
| <5 years, n (%) | 26 (43.3) | 5 (5.2) | 31 (19.9) |
| 5–10 years, n (%) | 23 (38.3) | 9 (9.4) | 32 (20.5) |
| 10–20 years, n (%) | 11 (18.3) | 33 (34.4) | 44 (28.2) |
| >20 years, n (%) | 0 (0.0) | 49 (51.0) | 49 (31.4) |
| Workplace location | |||
| Northern region, n (%) | 9 (15.0) | 20 (20.8) | 29 (18.6) |
| Central region, n (%) | 16 (26.7) | 22 (22.9) | 38 (24.4) |
| Greater Lisbon region, n (%) | 21 (35.0) | 42 (43.8) | 63 (40.4) |
| Southern region, n (%) | 11 (18.3) | 8 (8.3) | 19 (12.2) |
| Madeira and Azores, n (%) | 3 (5.0) | 4 (4.2) | 7 (4.5) |
These questions aimed to assess the level of knowledge regarding IR, as well as understanding the different forms of monitoring used by the sample (Supplement S1, Table 1).
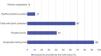
Most survey respondents were unaware of what type of occupational radiation exposure category they belonged to (103 of 156, 66.0%), with older participants mostly in category A (27 of 96, 28.7%). The vast majority of participants were monitored dosimetrically (150 of 156, 96.2%), despite only 60.4% (93 of 154) participants reporting a systematic use of the dosimeter. Full body monitoring was the most used approach by all participants (131 of 143, 91.6%). Almost a third of main operators also used a ring for radiation monitoring (15 of 53, 28.3%) (Figure 1). Dosimeter reading was performed monthly in 100 (64.9%) survey respondents. Exposure in more than one entity (54 of 156, 34.6%), as well as communication between them (13 of 82, 30.5%), was not a usual practice.
Most participants had access to dose recordings (117 of 155, 75.5%) and had not been previously called due to exceeding occupational dose limits (131 of 155, 84.5%). The majority knew the legally defined dose limits (100 of 155, 64.5%), as well as the need for mandatory notification in case of pregnancy (123 of 156, 78.8%), but were not aware of the trigger levels that determine the need for exposed patient follow-up (102 of 156, 65.4%).
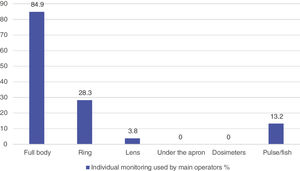
Having received training in radiation protection was reported by 104 of 156 (66.7%) survey respondents, but this was mainly informal training. Academic (formal) training was more commonly reported by younger participants (14 of 33, 42.4%) (Figure 2).
SafetyQuestions focusing on safety methods aimed to assess the use of techniques in clinical practice that minimize IR exposure (Supplement S1, Table 2).
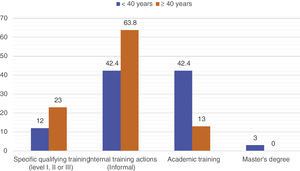
Most participants used techniques to minimize exposure to IR (141 of 156, 90.4%). Optimization of the interventional table and detector position were reported to be always used by 36 of 58 (62.1%) main operators. Fluoroscopy optimization and collimation were also frequently adopted by main operators (always or often in 68.4% and 65.5%, respectively). Distance to the radiation source was less frequently adopted by main operators (Figure 3) (details in Supplement S1, Table 2.1). IC operators mostly used low-dose protocols (total sample: 120 of 156, 76.9%; main operators: 48 of 61, 78.7%), favored a pulse rate of 7.5 pulse/second (p/s) during fluoroscopy (total sample: 71 of 128, 55.5%; main operators: 31 of 56, 55.4%) and a frame rate of 15 frame/second (f/s) in cinefluorography (total sample: 51 of 130, 39.2%; main operators: 28 of 56, 50.0%).
Almost a quarter reported having finished a procedure by reaching a radiation dose greater than tolerated levels (total sample: 42 of 156, 26.9%; main operators: 17 of 61, 27.9%), mainly when performing a CTO.
When not involved in direct patient contact, 96.5% (110 of 114) of survey respondents would follow specific room positioning within the Cath-Lab, with most favoring the bottom of the patient's table (81 of 112, 72.3%).
Personal protective equipmentOne section of the questionnaire also aimed to ascertain the access to and availability of radiological protection and its use within the Cath-Lab (Supplement S1, Table 3).
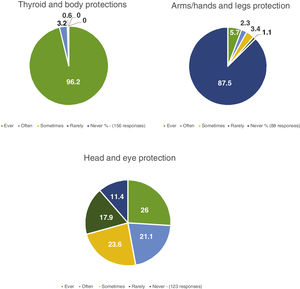
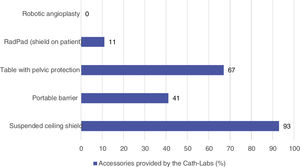
All participants reported using personal radiation protection equipment, mainly thyroid protectors and aprons (96.2%). Head and eye protections (32 of 123, 26.0%) and arms/hands and legs protections (5 of 88, 5.7%) were used less often (Figure 4). Despite largely available, eye protection with glasses/visors was seldom used (glasses: always and often in 50 of 127, 39.4%; visors: always and often in 6 of 91, 6.6%; glasses and visors: always and often in 56 of 156, 35.9%), and this was also reported when evaluating the main operators only (glasses: always and often in 26 of 58, 44.8%; visors: always and often in 4 of 45, 8.8%; glasses and visors: always and often in 30 of 61, 49.2%) (Supplement S1, Table 3.1). Protective gloves were frequently not used by survey respondents (only 3 of 44 main operators used, 6.8%). Beanies, gloves, sleeves, and boots were the radiation protection equipment least available by the Cath-Labs (Supplement S1, Figure 1).
Most Cath-Labs provided additional radiation protections (Figure 5) including suspended ceiling shield, table with pelvic protection and portable barrier, frequently used (Supplement S1, Figure 2).
Awareness and prevention of the consequences of radiationThe survey also assessed the awareness of participants regarding IR exposure, as well as determining the regularity of occupational health reviews (Supplement S1, Table 4).
Most survey respondents had attended at least one occupational health consultation (104 of 156, 66.7%), but only 39 of 122 (32.0%) reported a yearly attendance. Lens evaluation during occupational health review was reported by 28 of 134 (20.6%) of participants, and only one participant had been referred for an ophthalmology review. General investigations such as thyroid function tests, chest radiograph and electrocardiogram were usually included in the occupational health review (Table 2).
Exams requested in the occupational medicine consultation (%) (119 responses).
| Totaln=156 | |
|---|---|
| General analysis, n (%) | |
| 119 responses | 117 (98.3) |
| Thyroid function, n (%) | |
| 119 responses | 53 (44.5) |
| Chest X-ray, n (%) | |
| 119 responses | 46 (38.7) |
| Electrocardiogram, n (%) | |
| 119 responses | 64 (53.8) |
| Ophthalmology, n (%) | |
| 119 responses | 1 (0.8) |
| Thyroid ultrasound, n (%) | |
| 119 responses | 5 (4.2) |
| Other, n (%) | |
| 119 responses | 4 (3.4) |
Other: bone densitometry, respiratory function tests.
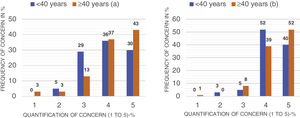
The majority of survey respondents had concerns regarding the exposure to radiation by operators (150 of 156, 96.2%) and patients (141 of 156, 90.4%) during procedures. Overall, the concern was high (Figure 6).
DiscussionThe findings of this survey highlight several features related to current knowledge, management and prevention strategies associated with IR across Cath-Labs in Portugal.
KnowledgeFor monitoring and surveillance, there are two categories of exposed workers:
- •
category A: workers who are liable to receive an effective dose of 20 mSv per year averaged over five consecutive years (100 mSv in 5 years) and of 50 mSv in any single year; an equivalent dose to the lens of the eye of 20 mSv per year averaged over five consecutive years (100 mSv in 5 years) and of 50 mSv in any single year; an equivalent dose to the extremities (hands and feet) or to the skin of 500 mSv in a year, and
- •
category B: workers who are not classified as A.3,13,14
Knowledge of these categories is crucial for the understanding of the suitability (and safety) for any given radiation dose exposure.
In the present survey, most of the workers did not know to which category they belonged (66.0%). This is also important in defining the periodicity of dosimeter readings (monthly in category A and quarterly in category B).13 A total of 64.9% of the survey respondents reported monthly readings, which should be equivalent to the true percentage of workers in category A.
The use of dosimeters should be systematic, which is not the case for about 40.0% of the survey respondents. Only two-thirds of participants knew the legally established limits for workers (50 mSv in any single year), as well as the exposure that should trigger patient follow-up due to possible tissue reactions (cumulative air kerma (Ka,r) of 5000 mGy or air kerma-area product (PKA) of 500 Gy cm2).15 Any pregnant or breastfeeding professional must report to the occupational health team, and may not perform functions involving a significant risk (should not exceed 1 mSv during pregnancy).4,13,16 The majority of participants appear to be aware of these regulations. Certified IR training is recommended to all team members, but this appears to be lacking in the majority of survey respondents.1,13
SafetyMethods and techniques to minimize radiation exposure were often used (90.4%), albeit “as low as reasonably achievable” (ALARA). The use of collimation and the reduced distance between the patient and the image detector (raised table, low detector) was widely used by the survey respondents (main operators). Collimation reduces the irradiated volume, the overall patient dose and scatter radiation, and this parameter directly affects PKA.1,17 In addition, guidelines also advise the use of “store-fluoro” option and to avoid angled projections, techniques to minimize IR that can potentially be used more often in Portuguese Cath-Labs.1,17
The use of low-dose protocols is important to minimize exposure, as was the case for 76.9% of survey respondents. Low-rate fluoroscopy at 7.5 p/s is a very effective measure to reduce both operator and patient radiation exposure, without significant effect on procedure duration, fluoroscopy time or contrast use. A reduction from 15 p/s to 7.5 p/s with a low-dose fluoroscopy mode minimizes radiation exposure by 67%.1,8,9,18–20 It is important to highlight that most main operators used fluoroscopy pulse rate at 7.5 p/s (55.4%), but this may not be standard practice in all Cath-Labs.
Performing a CTO was the main intervention leading to suspension of a procedure due to reaching the permitted radiation dose limit. Thereby, it is recommended that operators with experience in highly complex procedures must be aware of the importance of intensifying efforts to reduce radiation exposure for both the patient and the operator.8
Personal protective equipmentKnowledge of the distribution of scattered radiation levels around a patient and the effective use of protective devices are crucial for team protection.12,21 Personal protective devices comprise aprons (or vest/skirt), thyroid protectors, eyewear and radiation protection gloves.22 All survey respondents used aprons and thyroid protectors. Aprons should be individually tailored, because if oversized, they normally provide insufficient protection to the exposed areas. The fitting of the protective apron is often more important to reduce effective dose than the lead equivalent. Aprons do not protect the neck, and if no thyroid protection is worn, the dose at which the unprotected thyroid is irradiated may be twofold that of the effective dose.12
The most important factor in protecting the head and the eyes is the proper use of ceiling shields. Lead glasses/visors are an important component of the eyewear protection, proved to reduce the lens exposed dose substantially.12 In one study, 45.0% of IC professionals had posterior subcapsular lens changes attributed to IR exposure with infrequently use of lead glasses (only 57% of IC).23 Considering the low rates of glasses/visors used in this study, across all professionals, alongside the scarcity of lens evaluation at occupational health, eye health may be neglected in the sample.
Protective gloves block 30.0–40.0% of the scattered radiation with some limitation of finger movement. Its use can be justified when the IC have to operate close to the irradiated area.22 In the current study, only 6.8% of main operators of the survey respondents used this type of protection.
Curtains attached to the patient table and properly placed ceiling suspended shields have been shown to dramatically reduce operator dose.22 This type of protection is common in Cath-Labs and was used by most survey respondents.
Awareness and prevention of the consequences of radiationThere are two main biological effects of radiation: deterministic or tissue effects, which cause immediate and predictable tissue lesion, like cataracts (in professionals) and skin burns (in patients); and stochastic effects, with long term carcinogenic and genetic alterations.3 Most operators seem to have an insight into the deleterious effects of IR, with high rates of concern about their own and their patients’ IR exposure.
Workers in category A should have at least one yearly occupational health appointment (including ophthalmologic/lens evaluation).13 Only 32.0% of the participants in the survey have been checked with this periodicity, despite the estimated real percentage of operators in category A being 64.9%.
LimitationsThis survey has some methodological limitations worth highlighting. First, the survey was only sent to registered APIC members. Those professionals who were not registered, and would otherwise be eligible to participate, were not considered. This leads to the second limitation, which is the relatively small participant sample. However, considering the 85 IC subspecialists in Portugal in 2021, the main operators in the survey correspond to 71.8% of the population. Third, as certain members in the intervention team can have multiple roles, this may affect how they have responded to the survey. Finally, this survey was not applied to other areas of cardiology than IC and who also work with radiation, such as electrophysiology/pacing and pediatric cardiology. As such, the survey findings may not be generalizable to all national Cath-Labs or non-APIC members and would benefit from being disseminated to a wider sample of non-APIC members.
ConclusionsInterventional cardiology professionals have reported awareness of the use and implications of IR, as demonstrated by following relevant protocols and measures to minimize radiation, as well as the frequent use of personal protective equipment. Despite this, there is room for improvement, in particular when it comes to eyewear protection. In addition, considering the low rates of dosimeter use, as well as yearly occupational health follow-ups and the lack of knowledge of the legal limits of radiation dose, there is an urgent need to improve monitoring and certification. Similarly, the documentation and reporting of radiation protection practices should be performed in Cath-Labs to arrive at a national standardization of procedures.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to thanks to the physicians at Garcia de Orta Hospital, Vanessa de Sousa e Gabriela Cardoso, who collaborated very actively in the elaboration of the applied questionnaire. Also, the authors would like to express their gratitude to all APIC researchers and colleagues who cooperate in providing data for the current survey, and their commitment in attenuate the effects of IR in catheterization laboratories.