The authors report the case of a 53-year-old man, with a long-standing history of mild mitral stenosis, admitted for worsening fatigue. Transthoracic echocardiography (limited by poor image quality) showed mitral annular calcification, leaflets that were difficult to visualize and an estimated mitral valve area of 1.8 cm2 by the pressure half-time method. However, elevated mean transmitral and right ventricle/right atrium gradients were identified (39 and 117 mmHg, respectively). This puzzling discrepancy in the echocardiographic findings prompted investigation by transesophageal echocardiography, which revealed an echogenic structure adjacent to the mitral annulus, causing severe obstruction (effective orifice area 0.7 cm2). The suspicion of supravalvular mitral ring was confirmed during surgery. Following ring resection and mitral valve replacement there was significant improvement in the patient's clinical condition and normalization of the left atrium/left ventricle gradient.
Supravalvular mitral ring is an unusual cause of congenital mitral stenosis, characterized by an abnormal ridge of connective tissue on the atrial side of the mitral valve, which often obstructs mitral valve inflow. Few cases have been reported, most of them in children with concomitant congenital abnormalities. Diagnosis of a supravalvular mitral ring is challenging, since it is very difficult to visualize in most diagnostic tests. It was the combination of clinical and various echocardiographic findings that led us to suspect this very rare condition, enabling appropriate treatment, with excellent long-term results.
Os autores reportam o caso de um doente de 53 anos, com diagnóstico prévio de estenose mitral ligeira, admitido por agravamento do cansaço. O ecocardiograma (Eco) transtorácico, limitado pela janela acústica, mostrava válvula mitral com ecogenicidade aumentada a nível do anel, deficiente observação dos folhetos e área valvular estimada de 1,8 cm2 por tempo de hemipressão. No entanto, a identificação de elevados gradientes transmitral médio e ventrículo direito/aurícula direita (atingindo respetivamente 39 e 117 mmHg) intrigou os autores. No Eco transesofágico foi observada estrutura hiperecogénica sobre o anel mitral a condicionar obstrução grave (área do orifício efetivo de 0,7 cm2), o que levantou a suspeita de anel supramitral. Esta foi confirmada durante a cirurgia. Após a ressecção do anel e implantação de prótese mecânica, verificou-se uma franca melhoria clínica e normalização do gradiente aurícula esquerda (AE)/ventrículo esquerdo (VE).
O anel supramitral é uma causa invulgar de estenose mitral congénita, caracterizado pela presença de uma membrana fibrosa adjacente à face auricular da válvula mitral. Existem poucos casos reportados na literatura, sendo a maioria descritos em idade pediátrica e em associação a outras anomalias congénitas. O diagnóstico é desafiante, dado que o anel raramente é visualizado nos exames complementares. Uma elevada suspeita clínica e a integração dos vários achados ecocardiográficos são aspetos fundamentais para a sua identificação, permitindo o tratamento adequado com bons resultados a longo prazo.
Rheumatic disease is still the most common cause of mitral stenosis, particularly in developing countries,1 and congenital etiology is rare.
Supravalvular mitral ring, also called supramitral ring or supramitral membrane,1 is a rare form of congenital mitral stenosis. It is characterized by the presence of a ridge of connective tissue on the atrial side of the mitral valve, often attached to the valve annulus and/or leaflets,2,3 and may obstruct flow to the left atrium.
Supravalvular mitral ring was first described by Fisher in 1902,4 and fewer than 100 cases had been reported by 2002.5 The largest series to date included only 25 patients over a 20-year period,6 and there are no data on its actual incidence or predisposition by gender or race.1–3 In 90% of cases, it is associated with other congenital malformations, particularly Shone's complex, and/or mitral valve anomalies.1,2 Isolated occurrence, first described by Chung et al. in 1974,7 is rare.
Case reportA 53-year-old man had a history of bilateral vision loss due to juvenile glaucoma, intrinsic asthma, and suspected pulmonary sarcoidosis (under corticosteroid therapy). He had been previously followed in cardiology consultations for “a murmur since childhood”, and had been diagnosed with mild mitral stenosis based on a valve area of 1.8 cm2 estimated by the pressure half-time method.
In 2012, he was admitted to the emergency department for worsening fatigue and dyspnea. On physical examination, he was dyspneic, with mild hypoxemia at rest (PO2 60 mmHg), and hemodynamically stable. Cardiac auscultation revealed regular rhythm with a harsh mid-diastolic murmur, particularly audible over the apex, with presystolic accentuation, and pulmonary auscultation revealed rales in the left lung base and diffuse wheezing; there were no signs of right heart failure. Diagnostic exams included: electrocardiography showing sinus rhythm, heart rate (HR) of 80 bpm, and criteria for bi-atrial dilatation and partial right bundle branch block; laboratory tests showing elevated inflammatory markers; and chest X-ray showing increased cardiothoracic ratio and straightening of the left heart border, bilateral hilar enlargement, cephalization of the pulmonary vasculature and a reticulonodular/micronodular interstitial pattern, particularly in both lower pulmonary fields (similar to previous exams). The patient was admitted to the pneumology department with a diagnosis of respiratory infection.
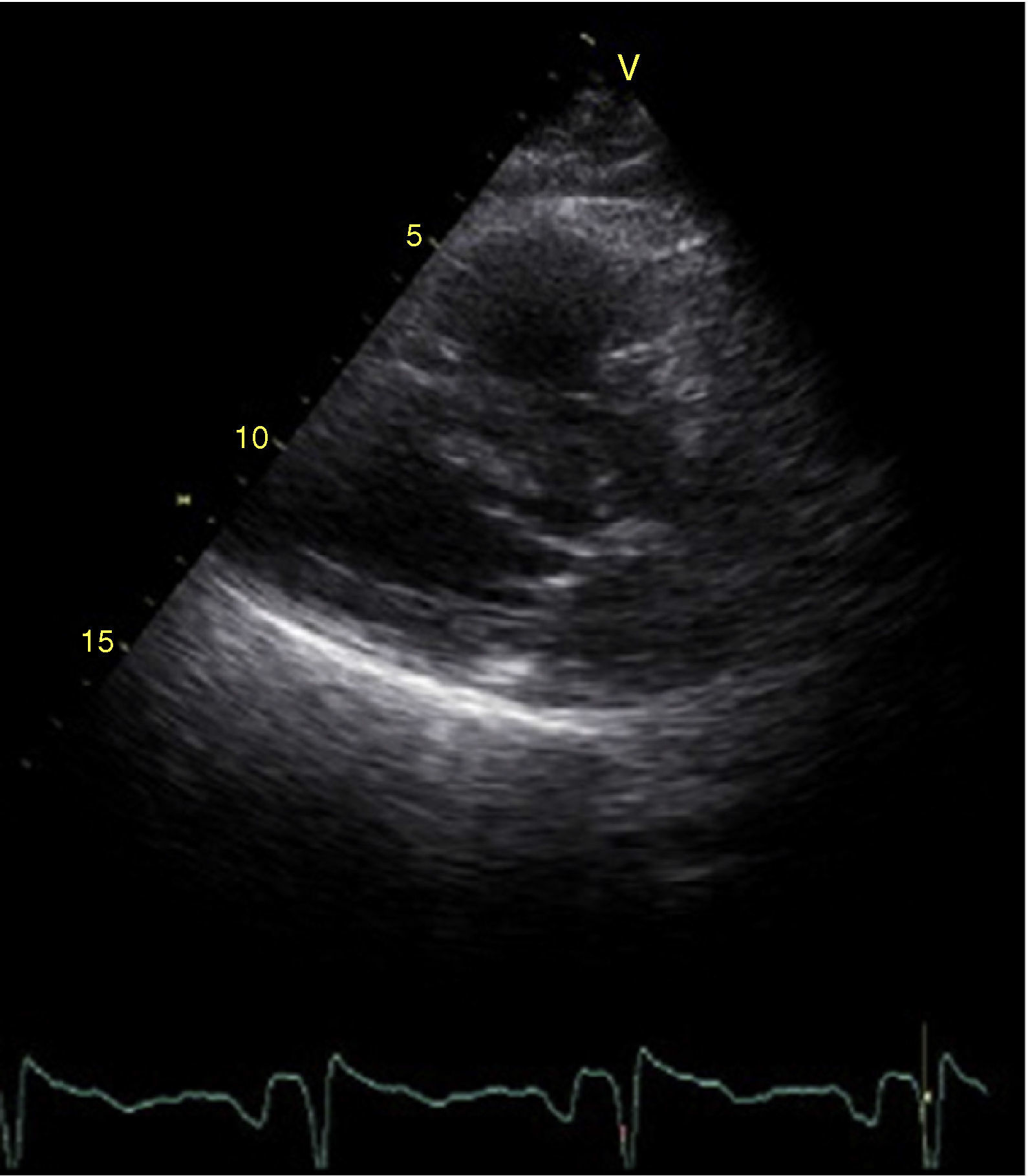
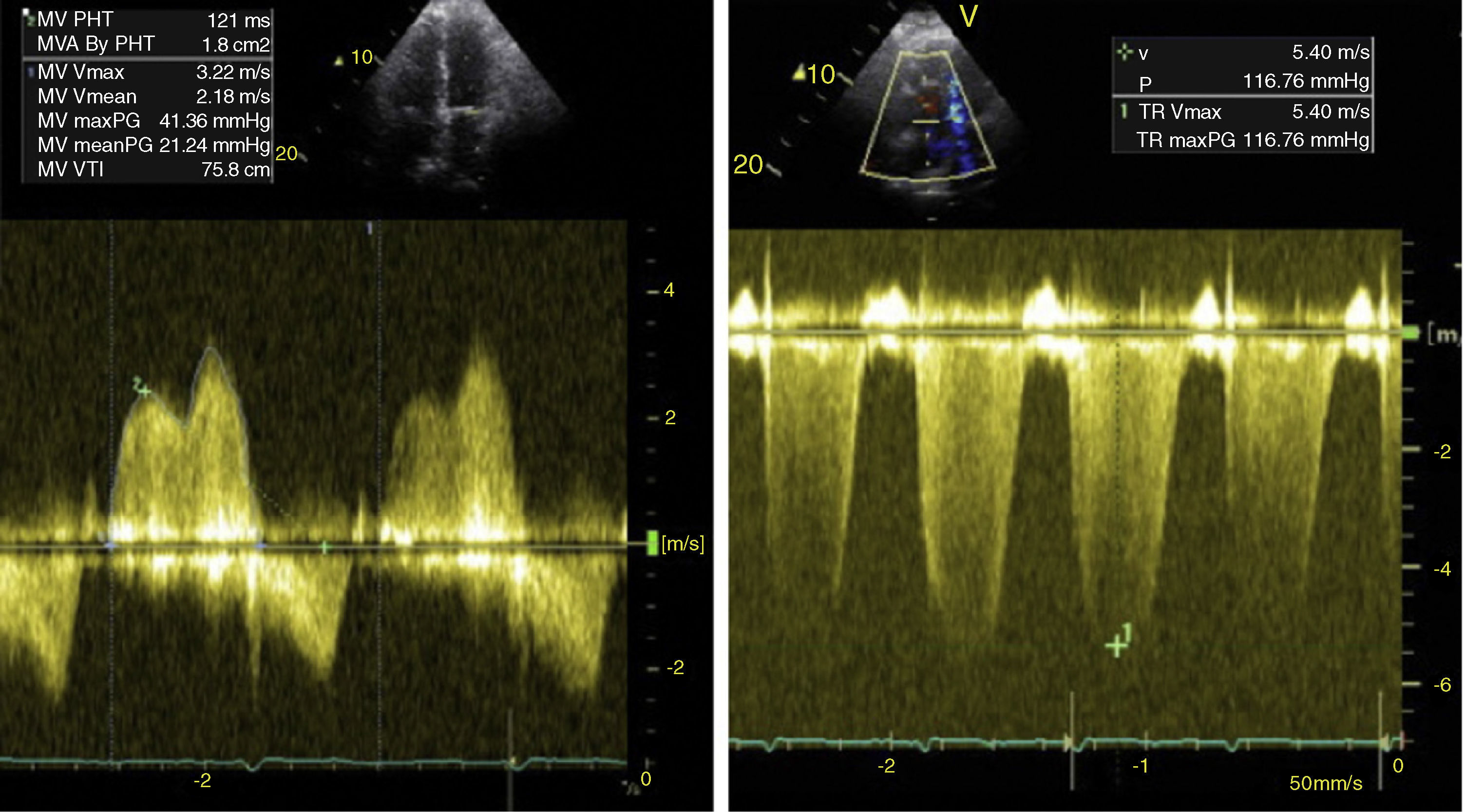
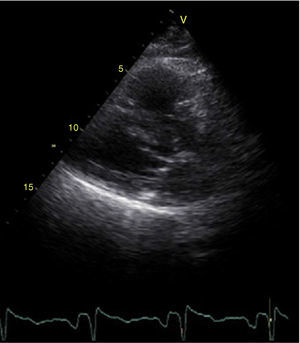
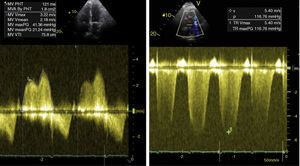
Antibiotic therapy was begun but the clinical setting persisted, and so transthoracic echocardiography (TTE) was performed, which, although limited by poor image quality, revealed no left ventricular (LV) dilatation and good global and segmental systolic function; mild left atrial (LA) dilatation (area in apical 4-chamber view: 22.8 cm2); mitral valve leaflets that were difficult to visualize but with apparently normal opening (Figure 1); a convergence zone on the atrial side of the mitral annulus plane that was difficult to visualize due to enhanced echogenicity; transmitral flow with peak diastolic gradient of 41 mmHg and mean of 21 mmHg (HR 104 bpm); valve area of 1.8 cm2 estimated by the pressure half-time method, with no mitral regurgitation; right ventricle/right atrium (RV/RA) systolic gradient of 117 mmHg, excluding pulmonary stenosis (Figure 2); and right chambers of normal dimensions and contractility.
Given the presence of severe pulmonary hypertension, thoracic computed tomography angiography was performed, which detected dilatation of the pulmonary artery trunk and its main branches and excluded pulmonary thromboembolism; calcification of the mitral annulus and aortic valve was observed.
Following optimization of therapy and consequent hemodynamic improvement, repeat TTE (at a HR of 85 bpm) showed a reduction in mean LA/LV gradient to 11 mmHg and in RV/RA gradient to 56 mmHg.
The discrepancy in the echocardiographic findings – a transvalvular gradient suggestive of severe obstruction of a valve with an estimated area >1.5 cm2 by the pressure half-time method and apparently normal leaflet opening – led to the hypothesis of supravalvular mitral ring or severe annular calcification.
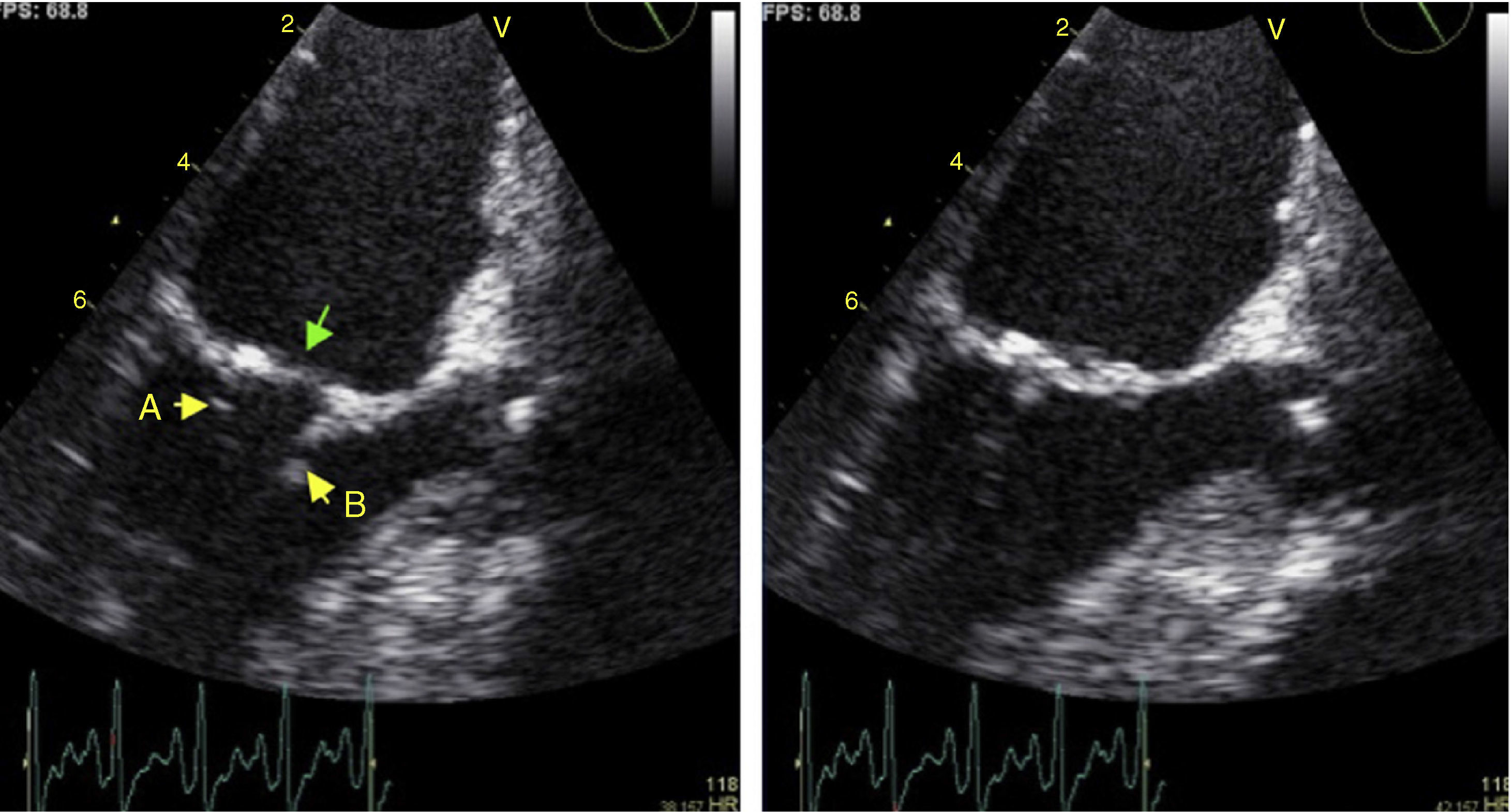
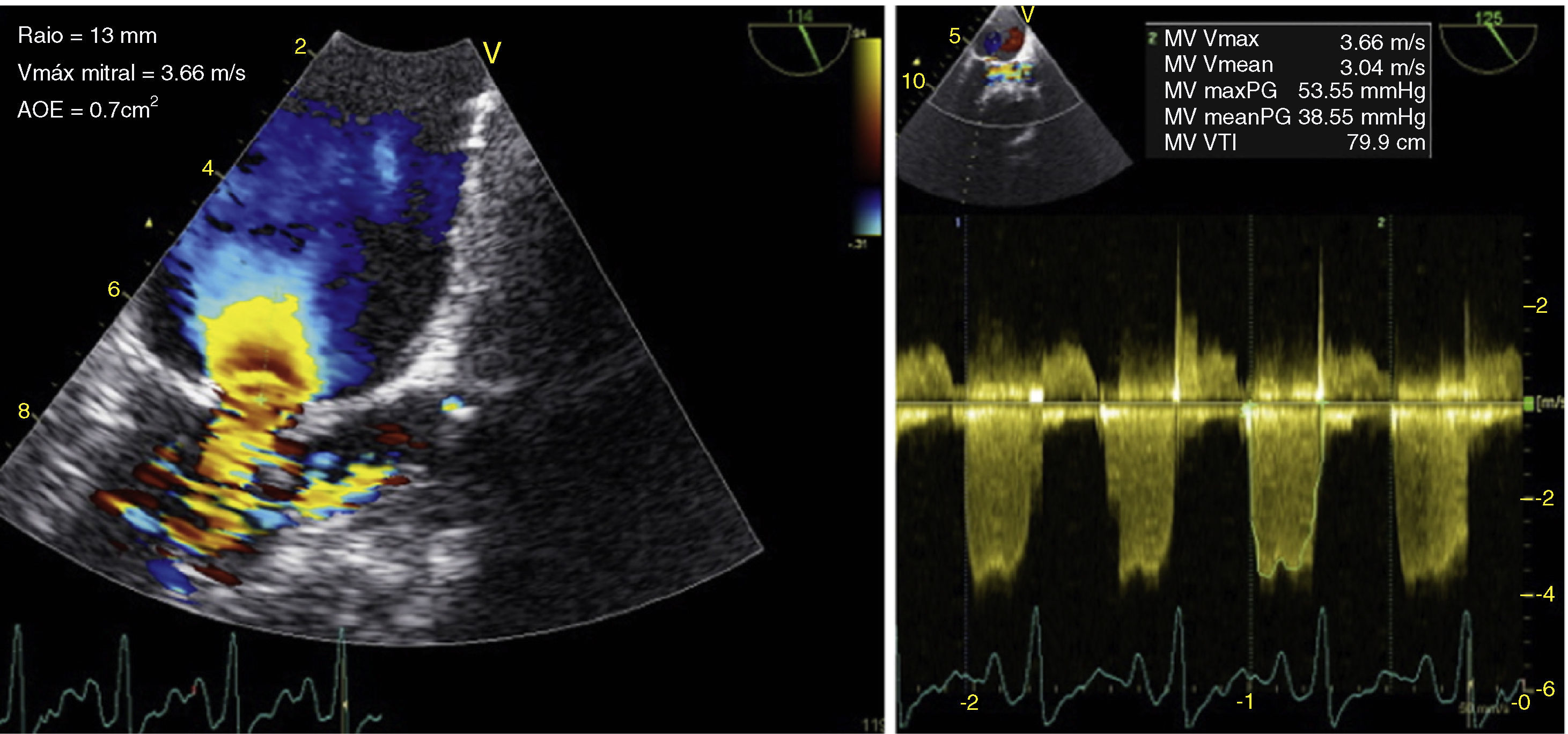
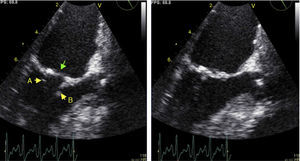
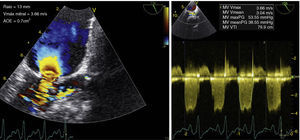
Transesophageal echocardiography (TEE), poorly tolerated by the patient and causing sinus tachycardia (HR 115 bpm), confirmed reasonable valve leaflet opening but showed an echogenic structure adjacent to the atrial side of the mitral annulus, distal to the insertion of the left atrial appendage (Figure 3), causing a high mean LA/LV diastolic gradient (39 mmHg). The effective orifice area estimated by the proximal isovelocity surface area method was 0.7 cm2, supporting the hypothesis of supravalvular mitral ring (Figure 4). No other congenital anomalies were identified.
Transesophageal echocardiography (121°) showing morphology of the mitral valve in diastole (left) and systole (right); good opening of the posterior (arrow A) and anterior (arrow B) leaflets can be seen, together with an echogenic structure on the atrial side of the mitral annulus (green arrow).
Transesophageal echocardiography (121°): a small convergence zone can be seen (poorly visualized on transthoracic echocardiography), suggesting supravalvular mitral stenosis; effective orifice area of 0.7 cm2 estimated by the proximal isovelocity surface area method (left); peak transmitral gradient of 54 mmHg and mean of 39 mmHg (right).
Catheterization revealed severe pulmonary hypertension (mean pulmonary artery pressure: 46 mmHg), high pulmonary capillary wedge pressure (PCWP) (20 mmHg) and an LA/LV gradient (based on PCWP) of 18 mmHg. Coronary angiography showed no coronary artery disease.
Given the presence of severe mitral valve obstruction associated with heart failure and pulmonary hypertension, the patient was referred for cardiac surgery. The surgical approach adopted was left atriotomy, which revealed a calcified structure attached to the mitral valve leaflets, consistent with supravalvular mitral ring. The ring was resected and since the valve could not be preserved, this was also excised, the posterior leaflet being preserved, and a mechanical prosthesis was implanted.
A year later, the patient showed improved functional capacity and heart failure symptoms (NYHA class I); TTE revealed a normally functioning mitral prosthesis with a mean gradient of 3.5 mmHg and RV/RA gradient of 26 mmHg.
DiscussionSupravalvular mitral ring is a rare entity with few cases reported.5 It is usually associated with other congenital anomalies and is often diagnosed in childhood. The case presented is thus unusual in that it occurred in isolation and was detected in an adult patient, an even rarer combination that was first reported in 2008.8
The absence of other congenital malformations, the poor image quality, and concomitant chronic pulmonary disease (that could have explained the patient's clinical setting) may have delayed the diagnosis. Although supramitral ring is a congenital defect, turbulent flow is known to cause a progressive increase in the stiffness and/or dimensions of the membrane, resulting in more severe obstruction over the years, leading to later onset of symptoms.3
Diagnosis of supravalvular mitral ring is challenging. Although there is considerable variation in the composition of the ring and in its relationship to the mitral valve, it usually presents as a thin membrane <1 mm thick, attached to the anterior mitral valve leaflet,2,3 and is thus difficult to visualize.7
TTE leads to diagnosis in less than 50% of cases.7 In a study by Sullivan et al., the ring was visualized before surgery in only 45% of the patients; postoperative retrospective analysis of the echocardiograms yielded the diagnosis in 91%, but this required a detailed frame-by-frame examination, which is impractical in clinical practice.5 Despite this limitation, TTE is essential in raising suspicion of the diagnosis.4 In the case presented, the discrepancy between echocardiographic findings – turbulent flow causing a high transmitral gradient in a morphologically normal valve – alerted the authors to the need for further investigation.
TEE is the best diagnostic exam for detection of supravalvular mitral ring,2,4 as it enables visualization of the ring and anchor points, assessment of native valve competence and differential diagnosis.5
Cardiac angiography, the preferred diagnostic technique when non-invasive exams were not generally available,9 is not now considered advantageous for diagnostic clarification.4,5 Cardiac magnetic resonance imaging has failed to detect supravalvular mitral ring in the cases in which it was used.2
In our patient, as in most reported cases, diagnostic confirmation was obtained only during surgery, although TEE had identified an anomalous structure adjacent to the mitral ring. Three-dimensional echocardiography may in the future be useful for assessing these patients, although there has been little mention of its use in the literature.10
When assessing a patient with suspected supravalvular mitral ring, it is essential to consider differential diagnosis from the more common cor triatriatum, which results from a failure of embryological development of the left pulmonary vein,4 leading to the left atrium being divided into two chambers by a membrane of fibromuscular tissue proximal to the LA appendage and well separated from the mitral valve. By contrast, supravalvular mitral ring arises from a failure of the endocardial cushions to divide completely,11 and is distal to the LA appendage, this being the main distinguishing feature between the two diagnoses.5
With regard to treatment, the first surgical repair of supravalvular mitral ring was described by Lynch et al. in 1962, in a series of 14 patients.7 In 2006, Collison et al. confirmed excellent long-term results.4 Surgical repair of the mitral valve is not always possible due to the presence of adhesions and contiguity with the anterior leaflet, and so valve replacement may be necessary as well as excision of the ring,10 as in the case presented. Factors determining a less favorable result are attachment of the membrane to the mitral valve, anomalies of the subvalvular apparatus, other congenital defects and pulmonary hypertension.5,6
Unlike other forms of mitral stenosis, in which balloon valvotomy is an acceptable alternative, surgery appears to be the only option for supravalvular stenosis.7 In a study by Spevak et al., of nine children with congenital mitral stenosis undergoing balloon angioplasty, less favorable results were obtained when the obstruction was not purely valvular, as it is with a supramitral ring.12
Follow-up of these patients is essential, given the risk of recurrence, which was first described by Tulloh et al.13 In a study of 23 children undergoing surgical resection of supravalvular mitral stenosis, four had recurrence of stenosis after 2–9 years. Although our patient has only been followed for a year, the outcome is satisfactory so far, with marked clinical improvement and significant reduction in the RV/RA gradient following removal of the obstruction.
ConclusionsThe case presented draws attention to a rare entity, for which the best method of diagnosis and treatment has yet to be established. A high level of clinical suspicion is necessary when performing TTE, and TEE is recommended whenever high transmitral gradients are observed. Resection of the ring, thus removing the obstruction, gives excellent results in the long term.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Almeida I, Caetano F, Trigo J, et al. Quando parece estenose mitral mas não é – implicações diagnósticas e terapêuticas. Rev Port Cardiol. 2014;33:471.