A 77-year-old woman with a history of hypertension, angioplasty of the anterior descending coronary artery, ischemic stroke, rheumatic mitral stenosis and atrial fibrillation, underwent gynecological surgery. Her warfarin therapy had been changed to enoxaparin, but at hospital discharge her international normalized ratio was below therapeutic levels, and so warfarin was restarted in addition to enoxaparin at prophylactic doses.
Two weeks after the procedure, she was admitted to the emergency department with chest discomfort. She was hypotensive and showed signs of peripheral hypoperfusion. The electrocardiogram revealed atrial fibrillation with complete atrioventricular block and ST-segment elevation in the inferior leads.
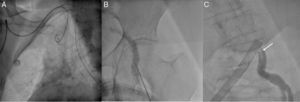
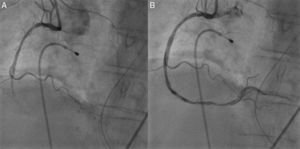
She was scheduled for primary angioplasty, which could not be performed by a radial approach due to the tortuosity of the subclavian artery (Figure 1A) and femoral access was hampered by absence of a pulse, and so a contrast-guided puncture was performed (Figure 1B and C). The external iliac artery was found to be occluded, but was passed using a hydrophilic guidewire. The mid segment of the right coronary artery was occluded by a thrombus (Figure 2A), which was removed by thrombectomy (Figure 2B).
Left heart catheterization: (A) radial access made impossible due to the tortuosity of the subclavian artery, which prevented passage of the guidewire; (B) contrast-guided puncture of the left femoral artery; (C) catheterization by femoral access revealing a mobile thread-like structure (arrow), consistent with a thrombus.
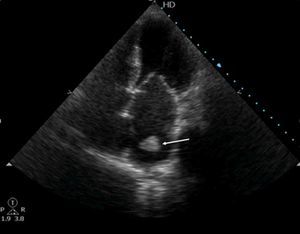
After reperfusion, signs of hypoperfusion persisted in the patient's lower limbs. In view of this finding, together with difficulty in femoral access, aortography was performed, which revealed thrombotic occlusion of the infrarenal abdominal aorta, extending to the iliac arteries (Figure 3). The echocardiogram showed a mass in the left atrium, consistent with a thrombus (Figure 4). Thromboembolectomy of the left iliac axis and femoro-femoral bypass were performed, but the patient developed multiple organ failure and died.
This case illustrates a cardioembolic catastrophe with both coronary and systemic embolization and highlights the importance of appropriate perioperative anticoagulation.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Arantes C, Marques J, Ribeiro S, Quina-Rodrigues C, Abreu G, Rocha S. Mãos quentes… pés frios…. Rev Port Cardiol. 2017;36:321–322.