Assessment of the electrocardiogram (ECG) in athletes remains controversial, with lack of standardization and difficulty in applying specific criteria in its interpretation. The purpose of this study was to assess variability in the interpretation of the ECG in athletes.
MethodsTwenty ECGs of competitive athletes were assessed by cardiologists and cardiology residents, 11 of them normal or with isolated physiological changes and nine pathological. Each ECG was classified as normal/physiological or pathological, with or without the use of specific interpretation criteria.
ResultsThe study presents responses from 58 physicians, 42 (72.4%) of them cardiologists. Sixteen (27.6%) physicians reported that they regularly assessed athletes and 32 (55.2%) did not use specific ECG interpretation criteria, of which the Seattle criteria were the most commonly used (n=13). Each physician interpreted 15±2 ECGs correctly, corresponding to 74% of the total number of ECGs (variation: 45%-100%). Interpretation of pathological ECGs was correct in 68% (variation: 22%-100%) and of normal/physiological in 79% (variation: 55%-100%). There was no significant difference in interpretation between cardiologists and residents (74±10% vs. 75±10%; p=0.724) or between those who regularly assessed athletes and those who did not (77±12% vs. 73±9%; p=0.286), but there was a trend for a higher rate of correct interpretation using specific criteria (77±10% vs. 72±10%; p=0.092). The reproducibility of the study was excellent (intraclass correlation coefficient=0.972; p<0.001).
ConclusionsA quarter of the ECGs were not correctly assessed and variability in interpretation was high. The use of specific criteria can improve the accuracy of interpretation of athletes’ ECGs, which is an important part of pre-competitive screening, but one that is underused.
A interpretação do eletrocardiograma (ECG) do atleta permanece controversa, com ausência de estandardização e dificuldade na aplicação de critérios específicos na sua interpretação. O objetivo deste trabalho é avaliar a variabilidade na interpretação do ECG de atletas.
MetodologiaVinte ECG de atletas foram avaliados por cardiologistas e internos de cardiologia, 11 normais ou apenas com alterações fisiológicas e nove patológicos. Cada ECG foi classificado pelos inquiridos em normal/com alterações fisiológicas ou patológico, usando ou não critérios específicos na sua interpretação.
ResultadosForam incluídas as respostas de 58 médicos, 42 (72,4%) cardiologistas. Dezasseis (27,6%) afirmaram avaliar frequentemente atletas e 32 (55,2%) não usar critérios específicos na interpretação do ECG, sendo os mais usados os critérios de Seattle (n=13). Em média, cada médico interpretou corretamente 15±2 ECG, correspondendo a 74% dos traçados (variação: 45-100%). A interpretação dos ECG foi correta em 68% (variação: 22-100%) dos patológicos e em 79% (variação: 55-100%) dos normais/com alterações fisiológicas. Não houve diferença significativa na interpretação entre cardiologistas e internos (74±10% versus 75±10%; p=0,724), nem entre os que avaliam frequentemente ou não atletas (77±12% versus 73±9%; p=0,286), verificando-se uma tendência para interpretação mais correta com critérios específicos (77±10% versus 72±10%; p=0,092). A reprodutibilidade do estudo foi excelente (intraclass correlation coefficient=0,972; p<0,001).
ConclusãoNa amostra estudada, cerca de um quarto dos ECG foram incorretamente avaliados, havendo uma elevada variabilidade na sua interpretação. O uso de critérios específicos na interpretação do ECG do atleta pode melhorar a acuidade deste exame no screening de atletas, mas são ainda subutilizados.
The main purpose of pre-competitive screening of athletes is to enable early (pre-clinical) identification of pathological conditions associated with increased risk of serious clinical events, including sudden death. Data from Italy show an 89% reduction in the incidence of sudden death in competitive athletes following the inclusion of the electrocardiogram (ECG) in pre-competitive screening.1 In view of this, most European countries currently recommend that pre-competitive screening should include personal and family history, physical examination, and a resting 12-lead ECG.2
Despite this evidence and the many arguments in support of ECG assessment, the inclusion of this exam in pre-competitive screening remains controversial, basically because of disagreement between Europe and the US, where it is not formally recommended.3,4 Of the arguments put forward against ECGs in athletes, the most frequent is the high false-positive rate, which can lead to unnecessary additional diagnostic exams and inappropriate exclusion of healthy individuals from competition. Most false positives result from incorrect interpretation of the ECG, mainly because alterations caused by exercise-induced physiological adaptations of the heart are wrongly classified as pathological.5–7 Thus, the central issue in this controversy is not whether the ECG should be included in pre-participation screening, but rather how the exam should be interpreted.
Various increasingly restrictive criteria have been published with the aim of standardizing interpretation of the ECG in athletes, notably those of the European Society of Cardiology (ESC), the Seattle criteria, and the ‘refined’ criteria.8–11 However, although the application of these criteria has led to a significantly lower number of false positives, they are still underused, and variability in the interpretation of the ECG in athletes remains high.12,13
The purpose of this study was to assess variability in the interpretation of the ECG in competitive athletes, with or without the use of specific criteria, in a sample of cardiologists and cardiology residents in Portugal.
MethodsStudy population and selection of electrocardiogramsTwenty ECGs of competitive athletes from pre-competitive screening assessments were selected. Most athletes were male (n=18) and Caucasian (n=17); median age was 24 (22-31) years. They performed at least eight hours of training a week and participated in various sports, most involving high-intensity dynamic exercise: medium- or long-distance running (n=7), soccer (n=4), cycling (n=2), rugby (n=1), swimming (n=1), gymnastics (n=1), tennis (n=1), boxing (n=1), judo (n=1) and kickboxing (n=1).
Of the selected ECGs, 11 were normal or with isolated physiological changes, and nine were pathological. The traces were selected after a validation and classification process agreed unanimously by three cardiologists experienced in sports medicine, particularly in interpreting athletes’ ECGs. For the pathological ECGs, the diagnosis of heart disease (cardiomyopathy or primary arrhythmia) was established on the basis of additional diagnostic exams. Table 1 presents the main characteristics of the athletes and ECGs under analysis.
Main characteristics of the athletes and electrocardiograms under analysis.
| ECG | Athlete | Interpretation | Main alterations |
|---|---|---|---|
| 1 | Male, Caucasian, age 35 years; running | Pathological (Brugada syndrome) | Type 1 Brugada |
| 2 | Male, Caucasian, age 24 years; judo | Pathological (ARVD) | Voltage criteria for RVH; right axis deviation (>120°) |
| 3 | Female, black, age 22 years; handball | Pathological (HCM) | Negative T waves in inferior leads and V5-V6 |
| 4 | Male, Caucasian, age 23 years; gymnastics | Physiological | Sinus bradycardia; incomplete right bundle branch block |
| 5 | Male, Caucasian, age 30 years; 11-a-side soccer | Pathological (anomalous coronary artery origin) | ST-segment depression in lateral leads, negative T waves in inferior leads |
| 6 | Male, Caucasian, age 23 years; running | Pathological (HCM) | Pathological Q waves in inferior and lateral leads |
| 7 | Male, Caucasian, age 31 years; running | Physiological | Sinus bradycardia; early repolarization |
| 8 | Male, Caucasian, age 35 years; running | Physiological | Sinus bradycardia; voltage criteria for LVH |
| 9 | Male, Caucasian, age 22 years; running | Physiological | Sinus bradycardia; early repolarization; voltage criteria for LVH |
| 10 | Male, black, age 24 years; boxing | Physiological | Sinus bradycardia; negative T waves in V1-V4; voltage criteria for LVH |
| 11 | Female, Caucasian, age 24 years; running | Physiological | Sinus bradycardia |
| 12 | Male, Caucasian, age 18 years; kickboxing | Physiological | Sinus arrhythmia; early repolarization; voltage criteria for LVH |
| 13 | Male, Caucasian, age 31 years; tennis | Pathological (WPW) | Short PR interval (<120 ms), delta wave |
| 14 | Male, Caucasian, age 30 years; cycling | Physiological | Sinus bradycardia |
| 15 | Male, Caucasian, age 19 years; 11-a-side soccer | Physiological | Sinus bradycardia; early repolarization; voltage criteria for LVH |
| 16 | Male, Caucasian, age 22 years; running | Physiological | Type 1 2nd-degree atrioventricular block |
| 17 | Male, black, age 25 years; 11-a-side soccer | Pathological (HCM) | Negative T waves in inferior leads and V3-V6 |
| 18 | Female, Caucasian, age 30 years; cycling | Pathological (ARVD) | Isolated PVCs with LBBB pattern and negative T waves in inferior leads |
| 19 | Male, Caucasian, age 15 years; swimming | Pathological (LQTS) | Long QT interval (QTc >480 ms) |
| 20 | Male, Caucasian, age 16 years; rugby | Physiological | Sinus bradycardia; juvenile pattern (negative T waves in V1-V3) |
ARVD: arrhythmogenic right ventricular dysplasia; HCM: hypertrophic cardiomyopathy; LBBB: left bundle branch block; LQTS: long QT syndrome; LVH: left ventricular hypertrophy; PVCs: premature ventricular contractions; QTc: corrected QT interval; RVH: right ventricular hypertrophy; WPW: Wolff-Parkinson-White syndrome.
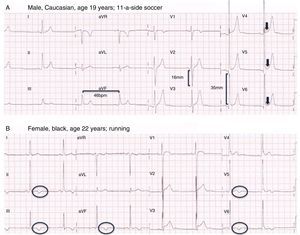
Figure 1 shows two examples of the ECGs included in this study, one non-pathological (Figure 1A), with only physiological alterations irrespective of the criteria used for its interpretation, and the other pathological (Figure 1B), that of an athlete with hypertrophic cardiomyopathy.
Two of the electrocardiograms (ECGs) in the study questionnaire. (A) ECG showing physiological alterations (sinus bradycardia, isolated voltage criteria for left ventricular hypertrophy and early repolarization); (B) ECG showing pathological alterations (negative T waves in all inferior leads and V5-V6), in an athlete diagnosed with hypertrophic cardiomyopathy.
The ECGs selected for this analysis were included in a form developed on the Google Forms platform (https://docs.google.com/forms/d/1vpVaTKSSlp2TfjiIkGtvX4qZBmkiNnnKnSKHKUYJSR4/viewform). The form was emailed to cardiologists and cardiology residents working in representative cardiology departments throughout Portugal (a total of 186 physicians). After an introductory text explaining the study's background and aims, the physicians were asked to identify themselves as a cardiologist or a cardiology resident and to state the main area of their clinical practice (specifically whether they worked within a subspecialty of cardiology), whether they regularly assessed athletes’ ECGs and whether they used specific criteria to do so, and if so, which. Each ECG was accompanied by information on the athlete's demographic characteristics (age, gender and race) and sport. For each ECG, the respondent was asked whether they considered the trace pathological or non-pathological. Only questionnaires with responses to all questions were considered valid, and only one could be submitted by each physician. Data collection took place over a period of one month (November 2015). All records were kept confidential and only the lead investigator had access to the results.
Statistical analysisThe data were analyzed using SPSS for Windows, version 22.0. Categorical variables were expressed as absolute values and percentages and compared with the chi-square test, while continuous variables were expressed as means ± standard deviation and were compared with the Student's t test under conditions of normality and homoscedasticity or as medians and interquartile range (25th-75th percentile) for non-normal distributions. The reproducibility of the study was assessed by calculating the intraclass correlation coefficient. Results with p<0.05 were considered statistically significant.
ResultsThe study included responses from 58 physicians (response rate 31%), 42 (72.4%) of them cardiologists and the remainder cardiology residents; 16 (27.6%) of the physicians stated that they regularly assessed athletes. More than half (32; 55.2%) did not use specific criteria for assessing athletes’ ECGs, and of those who did, the most commonly used were the Seattle criteria (n=13), followed by the ESC criteria (n=8). Table 2 presents the characteristics of the physicians surveyed and the percentages of correctly interpreted ECGs.
Interpretation of electrocardiograms according to the characteristics of the physicians surveyed and the methods used.
| n (%) | Total | Mean percentage of correctly interpreted ECGs | ||
|---|---|---|---|---|
| Total | Non-pathological | Pathological | ||
| Main area of clinical practice | ||||
| Cardiologist | 42 (72.4) | 74 | 79 | 67 |
| Cardiology resident | 16 (27.6) | 75 | 79 | 70 |
| Clinical cardiology | 41 (70.7) | 75 | 80 | 70 |
| Other areas of cardiology | 17 (29.3) | 72 | 78 | 64 |
| Regular assessment of athletes | 16 (27.6) | 77 | 84 | 68 |
| Interpretation of ECG | ||||
| Based on clinical experience | 32 (55.2) | 72 | 80 | 73 |
| Based on specific criteria | 26 (44.8) | 77 | 78 | 75 |
| ESC criteria | 8 (13.8) | 72 | 74 | 69 |
| Seattle criteria | 13 (22.4) | 77 | 80 | 74 |
| Refined criteria | 4 (6.9) | 86 | 86 | 86 |
| Other criteria | 1 (1.9) | 70 | 55 | 89 |
ECG: electrocardiogram; ESC: European Society of Cardiology.
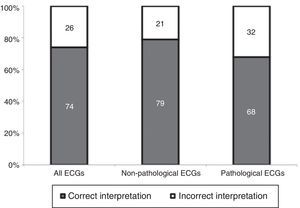
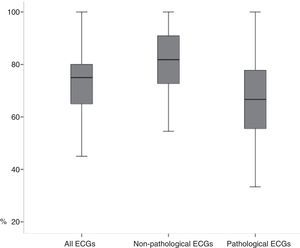
Each physician correctly interpreted a mean of 15±2 traces, corresponding to 74% of the ECGs analyzed, ranging between 45% and 100%. For pathological ECGs, the interpretation was correct in 68% of cases, ranging between 22% and 100%, while for non-pathological traces it was correct in 79% of cases (55%-100%) (Figures 2 and 3).
There were no statistically significant differences between cardiologists and residents concerning correctness of interpretation (74±10% vs. 75±10%; p=0.724), or between physicians who regularly assessed athletes’ ECGs and those who did not (77±12% vs. 73±9%; p=0.286). There was a trend for a higher rate of correct interpretation using specific criteria (77±10% vs. 72±10%; p=0.092). The intraclass correlation coefficient was 0.972 (95% confidence interval 0.951-0.987; p<0.001), showing that the reproducibility of the study was excellent.
DiscussionThis study demonstrates that assessment of the ECG in athletes remains less than optimal, since around a quarter of the ECGs analyzed were not correctly assessed and variability in interpretation was high. Although most of the physicians surveyed (cardiologists and residents) stated that they did not use specific criteria for ECG interpretations, there was a trend for a higher rate of correct interpretation using such criteria.
These results are consistent with previously published findings, and empirically there is a perception that variability (intra- and inter-observer) in interpretation of the ECG in athletes is high. However, there have been few recent studies on the subject. Berte et al.12 carried out a similar study, using a larger number of ECGs (138) and a smaller number of physicians (seven cardiologists and seven sports physicians), in which the ECGs were interpreted according to established criteria; variability was high, with disagreement on 35% of the ECGs overall. In a study by Hill et al.14 using a similar sample to the present work (18 ECGs analyzed by 53 pediatric cardiologists), the rate of incorrect interpretation was 31%. Analyzing 40 ECGs of athletes interpreted by physicians of various specialties, Drezner et al.15 showed that accuracy improved significantly after participants were provided with and asked to adopt the Seattle criteria; among cardiologists, the proportion of ECGs interpreted incorrectly fell from 15% to 4%.15
Although the difference was not statistically significant, in our study the rate of correct interpretation was lower for pathological ECGs, i.e. the proportion of false negatives was higher than that of false positives. Since the main problem with interpreting athletes’ ECGs is the high false-positive rate, the opposite would be expected. Irrespective of the characteristics analyzed, the proportion of pathological ECGs interpreted correctly was low except with the refined criteria,11 which were only used by a small number of physicians. Since these are the most recent criteria, they are probably more familiar to physicians with more experience and/or more interest in the area, who are thus more likely to interpret the ECG correctly. In previous studies the false-positive rate was similar, with more accurate interpretation seen after the adoption of specific criteria.14–16 For example, an assessment of the diagnostic accuracy of the Seattle criteria showed that the false-positive rate fell from 30% to 9% after they were applied.15 It is thus essential to raise awareness of specific criteria for the interpretation of the ECG in athletes and ensure they are correctly applied.
Variability in interpretation means that many athletes undergo unnecessary additional diagnostic exams, which have a considerable socioeconomic impact. There is also the question of the psychological stress caused by an incorrect reading, as well as the fact that these exams do not identify all causes of sudden death or ensure that athletes have been inappropriately barred from competing. Furthermore, the low prevalence of pathological ECGs in athletes means that they are more difficult to identify, increasing the variability of interpretation (the prevalence effect).15 Another important aspect is the influence of exercise-induced (physiological) electrical adaptations in the heart, which are affected by the athlete's demographic characteristics and the type of sport.5
There are many arguments in favor of including the ECG in pre-competitive screening of athletes, but it is still essential to optimize their interpretation. Possible ways to achieve this include training, standardization of methods, and centralized screening in specialized units. It is also important to raise awareness of the specific criteria for interpreting athletes’ ECGs and of their advantages and disadvantages, ideally through the publication of consensus documents and protocols indicating which criteria to adopt, in order to encourage standardization. However, the current criteria are the product of expert opinion and retrospective studies, and there have been few prospective analyses that can identify the ECG alterations that correlate most closely with clinical events, especially sudden death. Despite the shortcomings of the currently available criteria, their limitations cannot be evaluated, let alone overcome, until they have been applied in clinical practice.
LimitationsThis study has certain limitations that should be pointed out. The sample size was small, which limits the applicability of its results, and fewer than one third of surveyed physicians responded to the questionnaire. However, even so, the final study population was larger than in some previous studies on this subject. The characteristics of the selected athletes were very similar, with few non-Caucasians, females, or older athletes included. Although the questionnaire responses were confidential, physicians who were more interested and experienced in this area may have been more motivated to respond, and this also may have skewed the results. Some of the participants may have consulted the criteria when analyzing the ECGs, which hampers assessment of their existing knowledge; however, this does not affect the main purpose of the study and is in fact to be recommended in clinical practice, particularly for physicians who do not regularly assess athletes.
ConclusionsIn the study population, a quarter of athletes’ ECGs were not correctly assessed and variability in interpretation was high. Standardization of ECG interpretation in athletes with the use of specific criteria can improve the accuracy of this exam in pre-competitive screening. However, these criteria are still underused, a situation that could be changed by improvements in medical training in this area.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Dores H, Ferreira Santos J, Dinis P, et al. Variabilidade na interpretação do eletrocardiograma do atleta: mais uma limitação na avaliação pré-competitiva. Rev Port Cardiol. 2017;36:443–449.