A 2-day-old male infant required a conventional VVI pacemaker for congenital atrioventricular block. Three years later, he developed progressive heart failure due to left ventricular (LV) dysfunction and mitral regurgitation despite optimized medical treatment, and a cardiac resynchronization therapy (CRT) device was implanted. This is the first Portuguese report of CRT in a pediatric patient.
One-year echocardiographic follow-up showed that LV shortening fraction had improved and LV end-diastolic dimension and mitral regurgitation had decreased. New York Heart Association class had improved from III–IV to I at 1-year follow-up.
Um recém-nascido do sexo masculino apresenta bloqueio auriculo-ventricular completo pelo que foi implantado um pacemaker VVI ao 2.° dia de vida.
Três anos depois o doente desenvolve disfunção ventricular esquerda, regurgitação mitral grave e insuficiência cardíaca progressiva apesar da terapêutica médica otimizada. Nesse contexto efetuamos terapêutica de ressincronização (CRT). Este é o primeiro relato português de implantação de CRT em idade pediátrica.
Um ano após a implantação o ecocardiogrma mostra melhoria da fração de ejeção, redução do diâmetro telediastólico do ventrículo esquerdo e redução muito significativa da regurgitação mitral. A classe funcional de New York Heart Association melhorou de III-IV para I.
Right ventricular (RV) pacing is the standard treatment for children with advanced second-degree or complete atrioventricular block (AVB). However, permanent right ventricular pacing can be associated with left ventricular (LV) dysfunction, particularly in this age-group,1 and a significant number of children develop heart failure or dilated cardiomyopathy.2,3
The efficacy of cardiac resynchronization therapy (CRT) is well established in adults with severe LV systolic dysfunction or complete left bundle branch block.4–8
Upgrading patients with conventional right ventricular pacing to a biventricular pacing system has been shown to improve LV function.9 However, the few data available on the use of this strategy in pediatric patients come from non-randomized studies in heterogeneous populations.10–16
This article describes our initial experience with CRT implantation in a 3-year-old child, who had previously undergone permanent right ventricular pacing for congenital atrioventricular block and subsequently developed refractory heart failure. This is the first CRT implantation in such a young patient in Portugal.
Case reportA 3-year-old boy, weighing 12kg, the son of a mother with systemic lupus erythematosus, had a history of complete AVB detected prenatally at 27 weeks. There were no other complications during the pregnancy, which was full term. In the immediate postnatal period, the infant presented a setting of hypotonia and hypoactivity due to an inadequate escape rhythm, and a VVI pacemaker (St. Jude Microny II SR+) was implanted on the second day of life, a bipolar epicardial electrode being implanted in the right ventricular (RV) anterior wall and the generator in subxiphoid location.
The child remained pacemaker-dependent with no atrioventricular (AV) synchrony. Serial echocardiograms were normal, showing preserved LV function and no significant structural or functional valve abnormalities. The patient also showed good clinical evolution and normal height-weight development, requiring no medication.
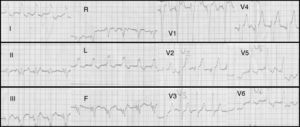
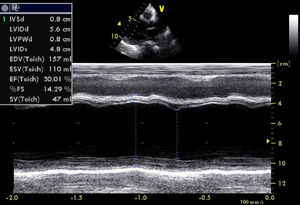
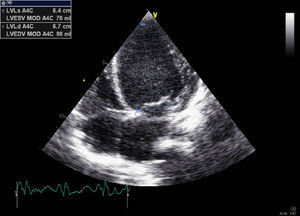
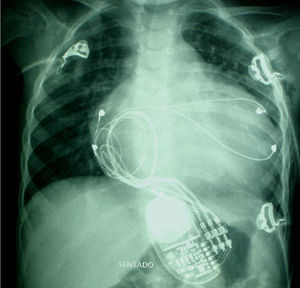
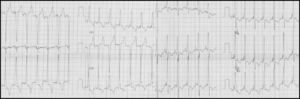
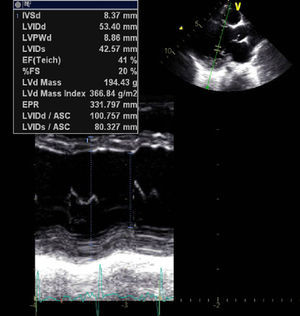
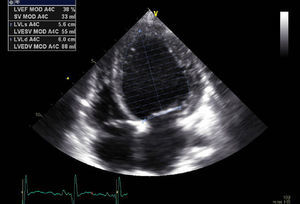
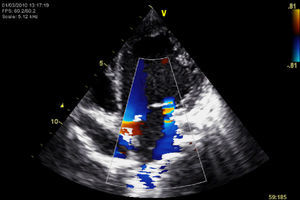
At the age of three, he was hospitalized with congestive heart failure (New York Heart Association [NYHA] functional class III–IV). The chest X-ray showed marked cardiomegaly and signs of pulmonary congestion (Figure 1). The electrocardiogram (ECG) showed atrioventricular dissociation, sinus rhythm and right ventricular pacing with QRS of 180ms (Figure 2). Echocardiography revealed LV dilatation (end-diastolic diameter [EDD] 56mm; end-systolic volume [ESV] 90ml), with severe systolic dysfunction (biplane ejection fraction 20%) due to generalized hypokinesia, with preserved RV global systolic function (as assessed by 2D echo, TAPSE measurement and strain imaging). The mitral valve presented no structural abnormalities but had moderate to severe functional regurgitation. There was also AV dyssynchrony as assessed by pulsed spectral Doppler of antegrade flow across the mitral valve (in complete AVB), together with interventricular dyssynchrony as assessed by pulsed spectral Doppler of antegrade flow in the LV and RV outflow tracts. Intraventricular dyssynchrony was also clearly identified in 2D and M-mode by the presence of septal flash (Figures 3–5).
Despite optimized medical treatment that included captopril 10mg three times a day, carvedilol 0.15mg twice a day, spironolactone 12.5mg/day and intravenous furosemide 10mg three times a day, the patient showed no clinical improvement, remaining in NYHA class III.
In view of the wide QRS interval, macroscopic signs of intraventricular dyssynchrony (septal flash), AV dissociation and the etiology of ventricular dysfunction, it was decided to upgrade the VVI pacemaker to a CRT system.
The patient underwent left thoracotomy under general anesthesia. The VVI generator and RV electrode were explanted, the latter showing unstable impedance values during the intraoperative period, probably due to damage during the procedure. Three bipolar leads (CapSure EPI, Medtronic) were then implanted in the right atrium, the RV inferior wall and the mid-basal segment of the LV lateral wall. The biventricular generator (InSync® III CRT-P, Medtronic) was implanted in subcostal location (Figure 6).
The generator was programmed in DDD mode at 90bpm and the AV delay was optimized by echocardiography.
The immediate postoperative period was complicated by an episode of sustained pulseless ventricular tachycardia, which reverted spontaneously during resuscitation maneuvers, and by left pneumothorax that required draining.
Following resolution of these complications, there was significant clinical improvement and the patient was discharged 13 days after CRT implantation.
After 11 months of follow-up, the child is currently asymptomatic (NYHA class I), medicated with captopril and carvedilol only.
The most recent ECG showed AV synchrony and QRS interval of 120ms (Figure 7).
There has been a slight improvement in LV dimensions (EDD 53mm; EDV 88ml) and significant improvement in systolic function (biplane ejection fraction: 38%) (Figures 8 and 9). There has also been a very significant reduction in the severity of mitral regurgitation, which is now only mild (Figure 10).
Resynchronization therapy in the case presented was effective both in relieving heart failure symptoms and in improving LV function and mitral regurgitation.
CRT resulted in reverse electrical remodeling (shortened QRS interval) and mechanical remodeling (reduced EDV and increased ejection fraction). At the same time, there was significant clinical improvement in heart failure symptoms. This was the first case in Portugal of CRT implantation in a pediatric patient.
RV pacing can lead to ventricular dyssynchrony, which at pediatric ages is usually mild, with no significant hemodynamic or clinical impact. However, a significant number of children develop dilated cardiomyopathy as a result of asynchronous electrical activation, as can occur in pediatric patients with preexcitation through right-sided accessory pathways.1,17
Indications for CRT in the pediatric population have not been validated, since few children with dilated cardiomyopathy meet the usual criteria recommended in the guidelines for adults (ejection fraction <35%, left bundle branch block and QRS >120ms, and NYHA class >II).18
The findings that most strongly supported the indication for CRT in our patient were the wide QRS, AV dissociation and mechanical dyssynchrony (septal flash on 2D echocardiography) and the etiology of ventricular dysfunction. Furthermore, pediatric patients with RV pacing-induced cardiomyopathy may be good candidates for CRT, as has been demonstrated in some small series of patients, who presented a higher than usual rate of responders.10,11,14,15,19
The technical difficulties and complications of CRT implantation in pediatric patients are its most challenging aspects. The rate of immediate complications in this population ranges between 10 and 19%,14,16 and mortality has reached 5% in some series.14 In very young children, as in the case presented, the only approach that enables implantation of the three leads is surgery under general anesthesia, which is associated with a higher risk of complications.
In our patient, there were two complications – ventricular tachycardia and left pneumothorax – both of which have been previously reported in this type of procedure.
ConclusionRight ventricular pacing is still the preferred therapy for children with complete AVB, but there is growing evidence that CRT has a role in the treatment of those who develop dilated cardiomyopathy secondary to RV pacing.
CRT may even constitute an alternative to conventional pacing, although there are few data on long-term outcomes.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Carmo, P. Terapêutica de ressincronização na miocardiopatia induzida pelo pacing ventricular direito em doente pediátrico. doi:10.1016/j.repc.2011.09.017.