Coronary artery disease is becoming the leading cause of death in women in Western society. However, the available data shows that women are still underdiagnosed and undertreated with guideline-recommended secondary prevention therapy, leading to a significantly higher rate of in-hospital complications and in-hospital mortality.
ObjectiveThe main objective of this work is to assess the approach to acute coronary syndrome (ACS) in Portugal, including form of presentation, in-hospital treatment and in-hospital complications, according to gender and in three different periods.
MethodsWe performed an observational study with retrospective analysis of all patients included between 2002 and 2019 in the Portuguese Registry of Acute Coronary Syndromes (ProACS), a voluntary, observational, prospective, continuous registry of the Portuguese Society of Cardiology and the National Center for Data Collection in Cardiology.
ResultsA total of 49 113 patients (34 936 men and 14 177 women) were included. Obesity, hypertension, diabetes (p<0.001 for all) and dyslipidemia (p=0.022) were all more prevalent in women, who were more frequently admitted for non-ST segment elevation ACS (p<0.001), and more frequently presented with atypical symptoms. Women had more time until needle and until reperfusion, which is less accessible to this gender (p<0.001). During hospitalization, women had a significantly higher risk of in-hospital mortality (OR 1.94 [1.78-2.12], p<0.001), major bleeding (OR 1.53 [1.30-1.80], p<0.001), heart failure (OR 1.87 [1.78-1.97], p<0.001), atrial fibrillation (OR 1.55 [1.36-1.77], p<0.001), mechanical complications (OR 2.12 [1.78-2.53], p<0.001), cardiogenic shock (OR 1.71 [1.57-1.87], p<0.001) and stroke (OR 2.15 [1.76-2.62], p<0.001). Women were more likely to have a normal coronary angiogram or coronary lesions with <50% luminal stenosis (p<0.001 for both), and thus a final diagnosis other than ACS. Both during hospitalization and at hospital discharge, women were less likely to receive guideline-recommended secondary prevention therapy.
ConclusionIn women admitted for ACS, revascularization strategies are still underused, as is guideline-recommended secondary prevention therapy, which may explain their higher incidence of in-hospital complications and higher unadjusted mortality.
A doença arterial coronária está-se a tornar a principal causa de morte no mundo ocidental no género feminino. Contudo, os dados de que dispomos mostram que as mulheres são ainda subdiagnosticadas e subtratadas com as terapias de prevenção secundária recomendadas, levando a taxas significativamente mais altas de complicações intra-hospitalares e mortalidade intra-hospitalar.
ObjetivoAvaliar a abordagem nacional às síndromas coronárias agudas, incluindo forma de apresentação, tratamento intra-hospitalar e complicações intra-hospitalares, de acordo com o género e em três períodos distintos.
MétodosEstudo observacional com análise retrospetiva de todos os doentes incluídos entre 2002 e 2019 no Registo Nacional de Síndromas Coronárias Agudas (RNSCA), um registo voluntário, observacional, prospetivo e contínuo da Sociedade Portuguesa de Cardiologia e do Centro Nacional de Coleção de Dados em Cardiologia.
ResultadosForam incluídos 49 113 doentes (34 936 homens e 14 177 mulheres). Obesidade, hipertensão arterial, diabetes mellitus (p < 0,001 para todos) e dislipidémia (p = 0,022) foram mais prevalentes nas mulheres, que são mais frequentemente admitidas por síndroma coronária aguda sem supradesnivelamento do segmento ST (p < 0,001) e mais frequentemente se apresentam com sintomas atípicos. As mulheres têm tempos mais longos até agulha e até reperfusão, esta última menos frequente neste género (p < 0,001). Durante hospitalização, as mulheres têm um risco significativamente maior de mortalidade intra-hospitalar (OR 1,94 [1,78;2,12], p < 0,001), hemorragia major (OR 1,53 [1,30;1,80], p < 0,001), insuficiência cardíaca (OR 1,87 [1,78;1,97], p < 0,001), fibrilhação auricular (OR 1,55 [1,36;1,77], p < 0,001), complicações mecânicas (OR 2,12 [1,78;2,53], p < 0,001), choque cardiogénico (OR 1,71 [1,57;1,87], p < 0,001) e acidente vascular cerebral (OR 2,15 [1,76;2,62], p < 0,001). É mais provável que as mulheres tenham uma coronariografia normal ou lesão coronárias com estenose luminal < 50% (p < 0,001 para ambos) e, assim, um diagnóstico final alternativo a síndroma coronária aguda. Seja durante hospitalização ou à alta hospitalar, é menos provável que as mulheres recebam as terapias de prevenção secundária recomendadas.
ConclusãoEm mulheres admitidas com síndroma coronária aguda as estratégias de revascularização são subutilizadas, assim como as terapias de prevenção secundária recomendadas, podendo justificar a maior incidência de complicações intra-hospitalares e maior mortalidade não ajustada.
Historically, coronary artery disease (CAD) has been perceived as a disease of men, rarely presenting in women, which leads to under-appreciation by health professionals of symptoms in women.1 However, this historical view is no longer correct, since CAD is now becoming the leading cause of death in women in Western society, overtaking uterine cancer, breast cancer and peripartum mortality.2 In Europe, around 23% of all deaths in females are due to CAD, and, although the number of women diagnosed with CAD has grown substantially in the last few years compared to men, the disease is still clearly underdiagnosed and undertreated in women, who have less access to revascularization and optimal medical therapy.2 In addition, although in recent decades there has been a significant reduction in mortality from myocardial infarction (MI), mainly in those aged over 65 years, there is evidence that this improvement in incidence and mortality is slowing down, especially in younger women aged under 55 years.3
The main objective of this work is to assess the approach to acute coronary syndrome (ACS) in Portugal, including form of presentation, in-hospital treatment and in-hospital complications, according to gender and in three different time periods: 2002-2010, 2011-2015, and 2016-2019, using data from the Portuguese Registry on Acute Coronary Syndromes (ProACS) of the Portuguese Society of Cardiology and the National Center for Data Collection in Cardiology.
MethodsWe performed an observational study with retrospective analysis of all patients included in the ProACS between 2002 and May 15, 2019 (n=49 247).
PopulationThe ProACS is a voluntary, observational, prospective, continuous performed through the CardioBase (InforTUCANO SI), which includes all patients aged ≥18 years of age with a diagnosis of ACS of less than 48hours duration, excluding patients with type 2, 4 or 5 MI. The inclusion and exclusion criteria and the data collection form have been published elsewhere.4,5 The three periods studied (2002-2010, 2011-2015, and 2016-2019) were chosen taking into consideration the release of new guidelines for the treatment of patients with ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction.
The population was characterized in demographic and clinical terms, including assessment of traditional cardiovascular risk factors, cardiovascular and non-cardiovascular history, description of the acute episode (including main symptom, physical examination, electrocardiogram and laboratory tests), therapy (during hospitalization and at hospital discharge), timings (such as door-to-balloon time), reperfusion strategy, coronary angiography results and complications.
Statistical analysisThe groups of men and women were characterized according to continuous and categorical variables, continuous variables being expressed as sample mean and standard deviation or median and interquartile range, and categorical variables as absolute and relative frequencies. Comparisons between groups regarding categorical variables were conducted using the chi-square test or Fisher's test. Means of continuous variables were compared using t tests whenever possible; otherwise, the Mann-Whitney U test was used to compare the medians. When three groups were analyzed together, the chi-square test or the Monte Carlo simulation test for the chi-square statistic was used for categorical variables and analysis of variance or the Kruskal-Wallis test was used for continuous variables. The statistical analysis was performed using IBM SPSS 19.0®, and a significance level of 5% was assumed for testing the hypothesis.
ResultsPopulation characteristicsAfter exclusion of 134 patients due to missing data, a total of 49 113 patients were included for analysis, divided by gender and in three different periods.
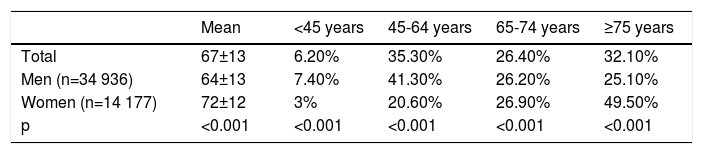
Most patients were included between 2002 and 2010 (n=30 046), with a progressive decrease in the number of until only 5287 patients included between 2016 and May 2019. The number of men included was considerably higher in all three periods (20 995 vs. 9051 in 2002-2010; 10 020 vs. 3760 in 2011-2015; and 3921 vs. 1366 in 2016-2019). We are unable to determine whether this is due to a smaller number of hospital admissions due to ACS in women or to a smaller number of records for women. The mean age of the population was 67±13 years, with women being, on average, eight years younger than men, and being the dominant gender in the younger age ranges (<45 years and 45-64 years), a tendency that was reversed in those aged ≥65 years (Table 1).
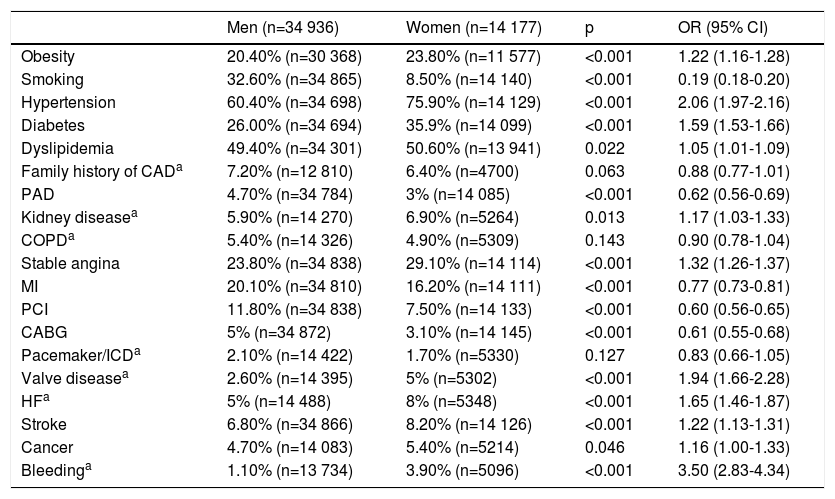
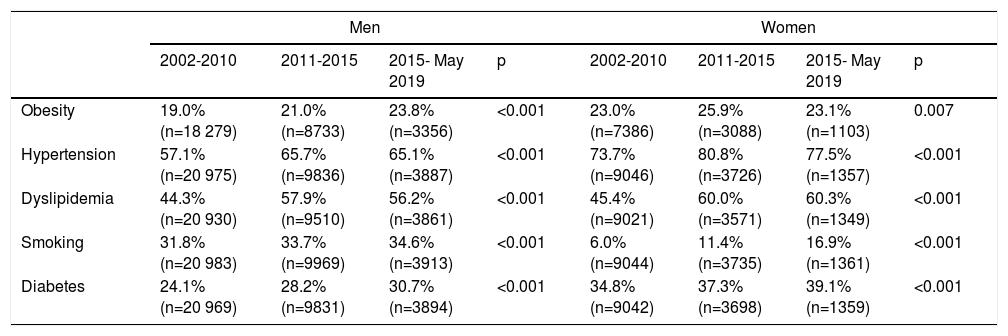
Regarding classical cardiovascular risk factors, significant differences were found in obesity, hypertension, diabetes and dyslipidemia, all of which were more prevalent in women (Tables 2 and 3). Furthermore, between 2002 and 2019 there was a clear tendency towards a greater prevalence of diabetes, dyslipidemia, and smoking among women admitted to hospital due to ACS, with only slight improvements in hypertension and obesity.
Cardiovascular risk factors and other personal history (2002-May 2019).
| Men (n=34 936) | Women (n=14 177) | p | OR (95% CI) | |
|---|---|---|---|---|
| Obesity | 20.40% (n=30 368) | 23.80% (n=11 577) | <0.001 | 1.22 (1.16-1.28) |
| Smoking | 32.60% (n=34 865) | 8.50% (n=14 140) | <0.001 | 0.19 (0.18-0.20) |
| Hypertension | 60.40% (n=34 698) | 75.90% (n=14 129) | <0.001 | 2.06 (1.97-2.16) |
| Diabetes | 26.00% (n=34 694) | 35.9% (n=14 099) | <0.001 | 1.59 (1.53-1.66) |
| Dyslipidemia | 49.40% (n=34 301) | 50.60% (n=13 941) | 0.022 | 1.05 (1.01-1.09) |
| Family history of CADa | 7.20% (n=12 810) | 6.40% (n=4700) | 0.063 | 0.88 (0.77-1.01) |
| PAD | 4.70% (n=34 784) | 3% (n=14 085) | <0.001 | 0.62 (0.56-0.69) |
| Kidney diseasea | 5.90% (n=14 270) | 6.90% (n=5264) | 0.013 | 1.17 (1.03-1.33) |
| COPDa | 5.40% (n=14 326) | 4.90% (n=5309) | 0.143 | 0.90 (0.78-1.04) |
| Stable angina | 23.80% (n=34 838) | 29.10% (n=14 114) | <0.001 | 1.32 (1.26-1.37) |
| MI | 20.10% (n=34 810) | 16.20% (n=14 111) | <0.001 | 0.77 (0.73-0.81) |
| PCI | 11.80% (n=34 838) | 7.50% (n=14 133) | <0.001 | 0.60 (0.56-0.65) |
| CABG | 5% (n=34 872) | 3.10% (n=14 145) | <0.001 | 0.61 (0.55-0.68) |
| Pacemaker/ICDa | 2.10% (n=14 422) | 1.70% (n=5330) | 0.127 | 0.83 (0.66-1.05) |
| Valve diseasea | 2.60% (n=14 395) | 5% (n=5302) | <0.001 | 1.94 (1.66-2.28) |
| HFa | 5% (n=14 488) | 8% (n=5348) | <0.001 | 1.65 (1.46-1.87) |
| Stroke | 6.80% (n=34 866) | 8.20% (n=14 126) | <0.001 | 1.22 (1.13-1.31) |
| Cancer | 4.70% (n=14 083) | 5.40% (n=5214) | 0.046 | 1.16 (1.00-1.33) |
| Bleedinga | 1.10% (n=13 734) | 3.90% (n=5096) | <0.001 | 3.50 (2.83-4.34) |
variable included only after October 2010.
CABG: coronary artery bypass grafting; CAD: coronary artery disease; COPD: chronic obstructive pulmonary disease; ICD: implantable cardioverter-defibrillator; HF: heart failure; MI: myocardial infarction; PAD: peripheral arterial disease; PCI: percutaneous coronary intervention.
Changes in classical cardiovascular risk factors.
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| 2002-2010 | 2011-2015 | 2015- May 2019 | p | 2002-2010 | 2011-2015 | 2015- May 2019 | p | |
| Obesity | 19.0%(n=18 279) | 21.0%(n=8733) | 23.8%(n=3356) | <0.001 | 23.0%(n=7386) | 25.9%(n=3088) | 23.1%(n=1103) | 0.007 |
| Hypertension | 57.1%(n=20 975) | 65.7%(n=9836) | 65.1%(n=3887) | <0.001 | 73.7%(n=9046) | 80.8%(n=3726) | 77.5%(n=1357) | <0.001 |
| Dyslipidemia | 44.3%(n=20 930) | 57.9%(n=9510) | 56.2%(n=3861) | <0.001 | 45.4%(n=9021) | 60.0%(n=3571) | 60.3%(n=1349) | <0.001 |
| Smoking | 31.8%(n=20 983) | 33.7%(n=9969) | 34.6%(n=3913) | <0.001 | 6.0%(n=9044) | 11.4%(n=3735) | 16.9%(n=1361) | <0.001 |
| Diabetes | 24.1%(n=20 969) | 28.2%(n=9831) | 30.7%(n=3894) | <0.001 | 34.8%(n=9042) | 37.3%(n=3698) | 39.1%(n=1359) | <0.001 |
The same pattern was seen in men, except for a slight, non-significant, improvement in hypertension and dyslipidemia (Table 3). Stable angina prior to hospital admission was more prevalent in women, as was a history of heart failure, significant valve disease, and stroke, while a personal history of MI, percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) was more common in men (Table 2).
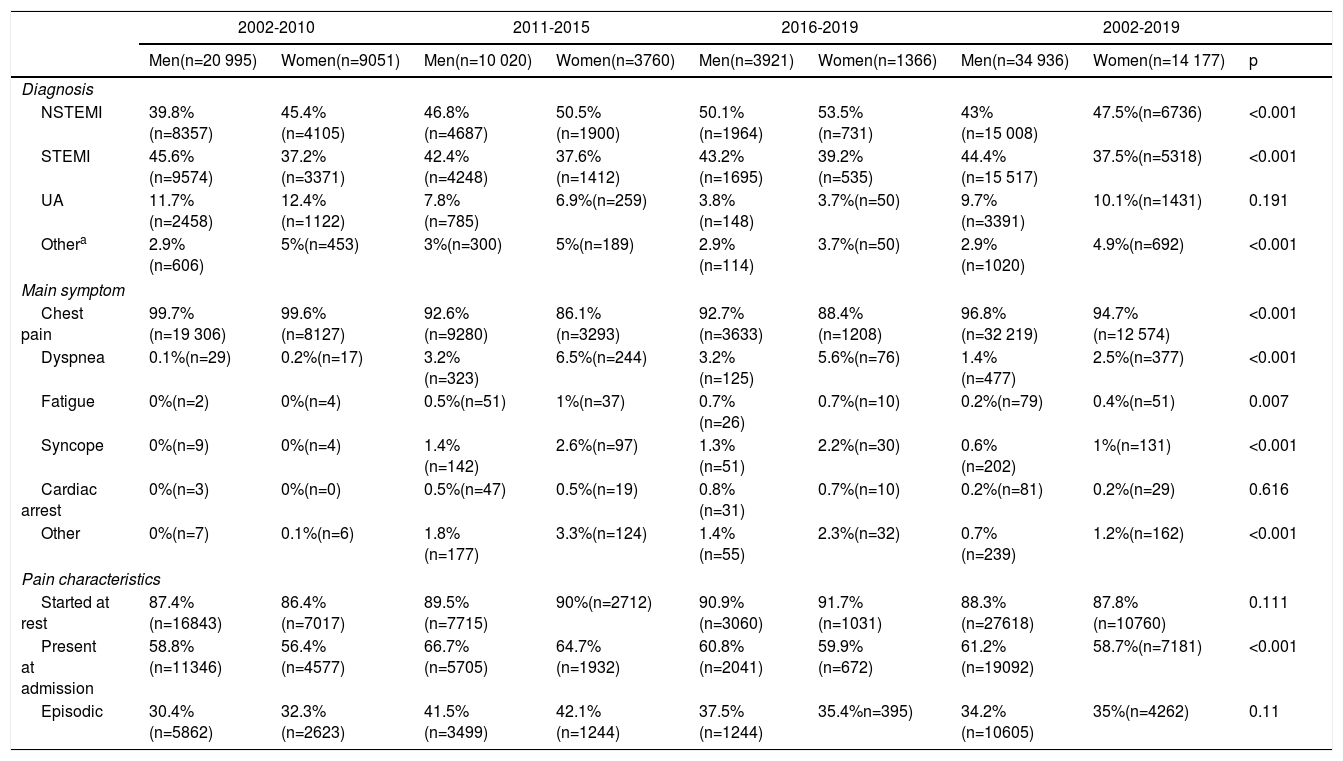
Hospital admission and timingsOur analysis by the three periods and by the overall study period reveals that compared with men, women were more frequently admitted with a diagnosis of non-ST-elevation ACS, including non-ST-elevation MI and unstable angina. Although the most common symptom at presentation in both sexes was chest pain, women more frequently presented with symptoms interpreted as equivalent, such as dyspnea, fatigue or syncope; in addition, fewer women reported chest pain at admission. Both of these are potential reasons for a delay in diagnosis (Table 4).
Diagnosis. main symptom and pain characteristics at hospital presentation.
| 2002-2010 | 2011-2015 | 2016-2019 | 2002-2019 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Men(n=20 995) | Women(n=9051) | Men(n=10 020) | Women(n=3760) | Men(n=3921) | Women(n=1366) | Men(n=34 936) | Women(n=14 177) | p | |
| Diagnosis | |||||||||
| NSTEMI | 39.8%(n=8357) | 45.4%(n=4105) | 46.8%(n=4687) | 50.5%(n=1900) | 50.1%(n=1964) | 53.5%(n=731) | 43%(n=15 008) | 47.5%(n=6736) | <0.001 |
| STEMI | 45.6%(n=9574) | 37.2%(n=3371) | 42.4%(n=4248) | 37.6%(n=1412) | 43.2%(n=1695) | 39.2%(n=535) | 44.4%(n=15 517) | 37.5%(n=5318) | <0.001 |
| UA | 11.7%(n=2458) | 12.4%(n=1122) | 7.8%(n=785) | 6.9%(n=259) | 3.8%(n=148) | 3.7%(n=50) | 9.7%(n=3391) | 10.1%(n=1431) | 0.191 |
| Othera | 2.9%(n=606) | 5%(n=453) | 3%(n=300) | 5%(n=189) | 2.9%(n=114) | 3.7%(n=50) | 2.9%(n=1020) | 4.9%(n=692) | <0.001 |
| Main symptom | |||||||||
| Chest pain | 99.7%(n=19 306) | 99.6%(n=8127) | 92.6%(n=9280) | 86.1%(n=3293) | 92.7%(n=3633) | 88.4%(n=1208) | 96.8%(n=32 219) | 94.7%(n=12 574) | <0.001 |
| Dyspnea | 0.1%(n=29) | 0.2%(n=17) | 3.2%(n=323) | 6.5%(n=244) | 3.2%(n=125) | 5.6%(n=76) | 1.4%(n=477) | 2.5%(n=377) | <0.001 |
| Fatigue | 0%(n=2) | 0%(n=4) | 0.5%(n=51) | 1%(n=37) | 0.7%(n=26) | 0.7%(n=10) | 0.2%(n=79) | 0.4%(n=51) | 0.007 |
| Syncope | 0%(n=9) | 0%(n=4) | 1.4%(n=142) | 2.6%(n=97) | 1.3%(n=51) | 2.2%(n=30) | 0.6%(n=202) | 1%(n=131) | <0.001 |
| Cardiac arrest | 0%(n=3) | 0%(n=0) | 0.5%(n=47) | 0.5%(n=19) | 0.8%(n=31) | 0.7%(n=10) | 0.2%(n=81) | 0.2%(n=29) | 0.616 |
| Other | 0%(n=7) | 0.1%(n=6) | 1.8%(n=177) | 3.3%(n=124) | 1.4%(n=55) | 2.3%(n=32) | 0.7%(n=239) | 1.2%(n=162) | <0.001 |
| Pain characteristics | |||||||||
| Started at rest | 87.4%(n=16843) | 86.4%(n=7017) | 89.5%(n=7715) | 90%(n=2712) | 90.9%(n=3060) | 91.7%(n=1031) | 88.3%(n=27618) | 87.8%(n=10760) | 0.111 |
| Present at admission | 58.8%(n=11346) | 56.4%(n=4577) | 66.7%(n=5705) | 64.7%(n=1932) | 60.8%(n=2041) | 59.9%(n=672) | 61.2%(n=19092) | 58.7%(n=7181) | <0.001 |
| Episodic | 30.4%(n=5862) | 32.3%(n=2623) | 41.5%(n=3499) | 42.1%(n=1244) | 37.5%(n=1244) | 35.4%n=395) | 34.2%(n=10605) | 35%(n=4262) | 0.11 |
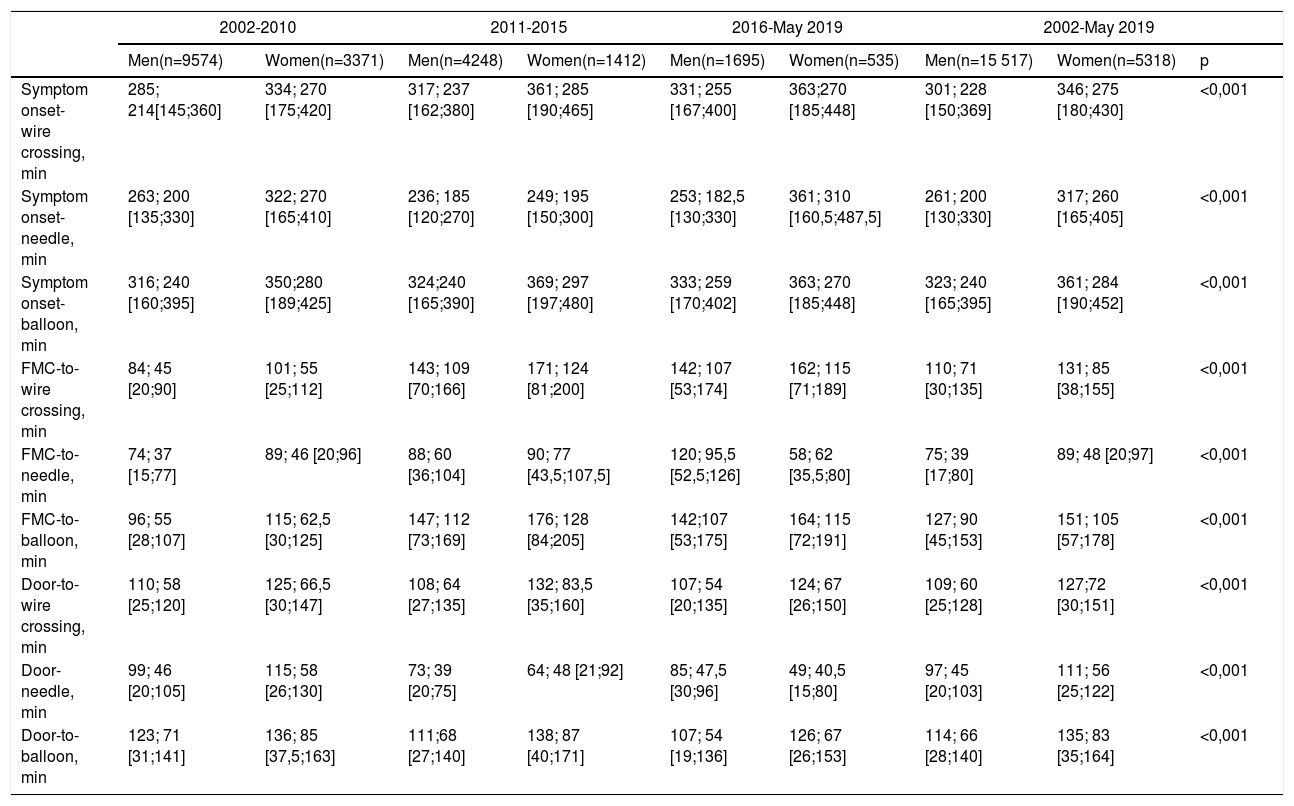
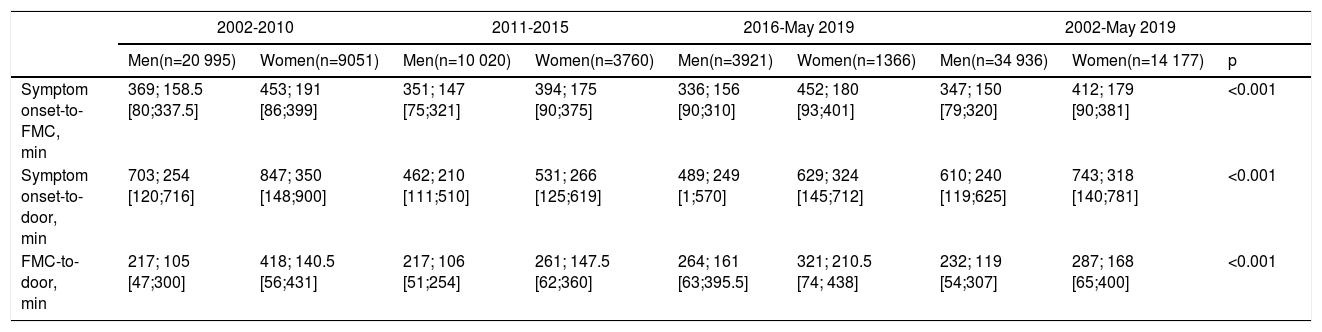
Regarding timings between, first medical contact (FMC) or arrival at the door, there are several interesting findings. In the overall period considered, in all the timings analyzed for patients with STEMI (Table 5), times to needle and to reperfusion were longer in women (whether reperfusion is defined as time-to-balloon or wire-crossing, and whether the starting point is defined as symptom onset, FMC or arrival at the door). As shown in Table 6, however, there was no continuous or consistent improvement over the periods when compared within the same gender; for example, regarding FMC-to-needle or FMC-to-reperfusion times, the shortest times were in the period 2002-2010 for both sexes (except for FMC-to-needle time in women, for which the shortest time was in the period 2016-2019). Also, when considering times starting at symptom onset, the same pattern is observed, with the longest delays in the more recent periods, with the exception of symptom onset-to-needle time in men, for which an improvement was noted, and symptom onset-to-balloon in women, for which there are no significant differences.
Changes in timings starting at symptom onset, arrival at the door and first medical contact for patients admitted with ST-elevation myocardial infarction.
| 2002-2010 | 2011-2015 | 2016-May 2019 | 2002-May 2019 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Men(n=9574) | Women(n=3371) | Men(n=4248) | Women(n=1412) | Men(n=1695) | Women(n=535) | Men(n=15 517) | Women(n=5318) | p | |
| Symptom onset-wire crossing, min | 285; 214[145;360] | 334; 270 [175;420] | 317; 237 [162;380] | 361; 285 [190;465] | 331; 255 [167;400] | 363;270 [185;448] | 301; 228 [150;369] | 346; 275 [180;430] | <0,001 |
| Symptom onset-needle, min | 263; 200 [135;330] | 322; 270 [165;410] | 236; 185 [120;270] | 249; 195 [150;300] | 253; 182,5 [130;330] | 361; 310 [160,5;487,5] | 261; 200 [130;330] | 317; 260 [165;405] | <0,001 |
| Symptom onset-balloon, min | 316; 240 [160;395] | 350;280 [189;425] | 324;240 [165;390] | 369; 297 [197;480] | 333; 259 [170;402] | 363; 270 [185;448] | 323; 240 [165;395] | 361; 284 [190;452] | <0,001 |
| FMC-to-wire crossing, min | 84; 45 [20;90] | 101; 55 [25;112] | 143; 109 [70;166] | 171; 124 [81;200] | 142; 107 [53;174] | 162; 115 [71;189] | 110; 71 [30;135] | 131; 85 [38;155] | <0,001 |
| FMC-to-needle, min | 74; 37 [15;77] | 89; 46 [20;96] | 88; 60 [36;104] | 90; 77 [43,5;107,5] | 120; 95,5 [52,5;126] | 58; 62 [35,5;80] | 75; 39 [17;80] | 89; 48 [20;97] | <0,001 |
| FMC-to-balloon, min | 96; 55 [28;107] | 115; 62,5 [30;125] | 147; 112 [73;169] | 176; 128 [84;205] | 142;107 [53;175] | 164; 115 [72;191] | 127; 90 [45;153] | 151; 105 [57;178] | <0,001 |
| Door-to-wire crossing, min | 110; 58 [25;120] | 125; 66,5 [30;147] | 108; 64 [27;135] | 132; 83,5 [35;160] | 107; 54 [20;135] | 124; 67 [26;150] | 109; 60 [25;128] | 127;72 [30;151] | <0,001 |
| Door-needle, min | 99; 46 [20;105] | 115; 58 [26;130] | 73; 39 [20;75] | 64; 48 [21;92] | 85; 47,5 [30;96] | 49; 40,5 [15;80] | 97; 45 [20;103] | 111; 56 [25;122] | <0,001 |
| Door-to-balloon, min | 123; 71 [31;141] | 136; 85 [37,5;163] | 111;68 [27;140] | 138; 87 [40;171] | 107; 54 [19;136] | 126; 67 [26;153] | 114; 66 [28;140] | 135; 83 [35;164] | <0,001 |
Values are mean; median [25th;75th percentile].
FMC: first medical contact.
Changes in timings starting at symptom onset, arrival at the door and first medical contact for patients admitted with ST-elevation myocardial infarction, according to gender.
| 2002-2010 | 2011-2015 | 2016-May 2019 | 2002-May 2019 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Men(n=20 995) | Women(n=9051) | Men(n=10 020) | Women(n=3760) | Men(n=3921) | Women(n=1366) | Men(n=34 936) | Women(n=14 177) | p | |
| Symptom onset-to-FMC, min | 369; 158.5 [80;337.5] | 453; 191 [86;399] | 351; 147 [75;321] | 394; 175 [90;375] | 336; 156 [90;310] | 452; 180 [93;401] | 347; 150 [79;320] | 412; 179 [90;381] | <0.001 |
| Symptom onset-to-door, min | 703; 254 [120;716] | 847; 350 [148;900] | 462; 210 [111;510] | 531; 266 [125;619] | 489; 249 [1;570] | 629; 324 [145;712] | 610; 240 [119;625] | 743; 318 [140;781] | <0.001 |
| FMC-to-door, min | 217; 105 [47;300] | 418; 140.5 [56;431] | 217; 106 [51;254] | 261; 147.5 [62;360] | 264; 161 [63;395.5] | 321; 210.5 [74; 438] | 232; 119 [54;307] | 287; 168 [65;400] | <0.001 |
Values are mean; median [25th;75th percentile].
FMC: first medical contact.
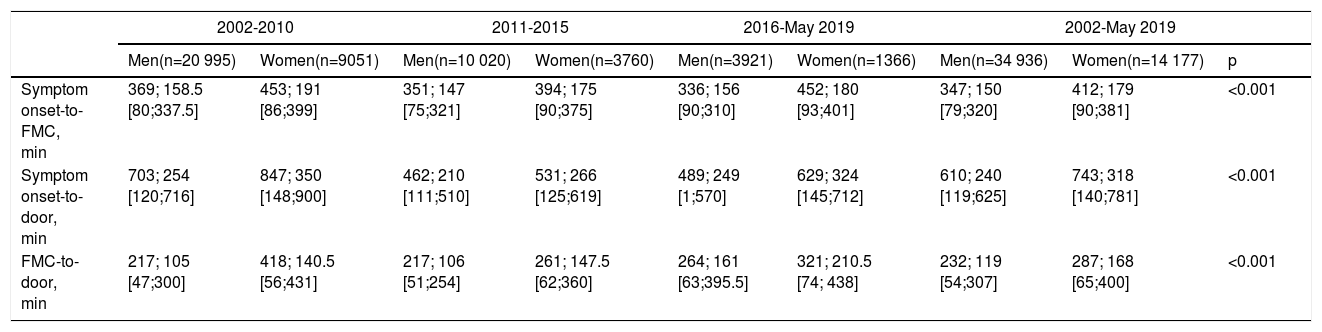
The same gender differences are seen in the timings for all patients with ACS (Table 7), with women having significantly longer times than men.
Changes in timings starting at symptom onset and first medical contact for all patients with acute coronary syndrome.
| 2002-2010 | 2011-2015 | 2016-May 2019 | 2002-May 2019 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Men(n=20 995) | Women(n=9051) | Men(n=10 020) | Women(n=3760) | Men(n=3921) | Women(n=1366) | Men(n=34 936) | Women(n=14 177) | p | |
| Symptom onset-to-FMC, min | 369; 158.5 [80;337.5] | 453; 191 [86;399] | 351; 147 [75;321] | 394; 175 [90;375] | 336; 156 [90;310] | 452; 180 [93;401] | 347; 150 [79;320] | 412; 179 [90;381] | <0.001 |
| Symptom onset-to-door, min | 703; 254 [120;716] | 847; 350 [148;900] | 462; 210 [111;510] | 531; 266 [125;619] | 489; 249 [1;570] | 629; 324 [145;712] | 610; 240 [119;625] | 743; 318 [140;781] | <0.001 |
| FMC-to-door, min | 217; 105 [47;300] | 418; 140.5 [56;431] | 217; 106 [51;254] | 261; 147.5 [62;360] | 264; 161 [63;395.5] | 321; 210.5 [74; 438] | 232; 119 [54;307] | 287; 168 [65;400] | <0.001 |
Values are mean; median [25th;75th percentile].
FMC: first medical contact.
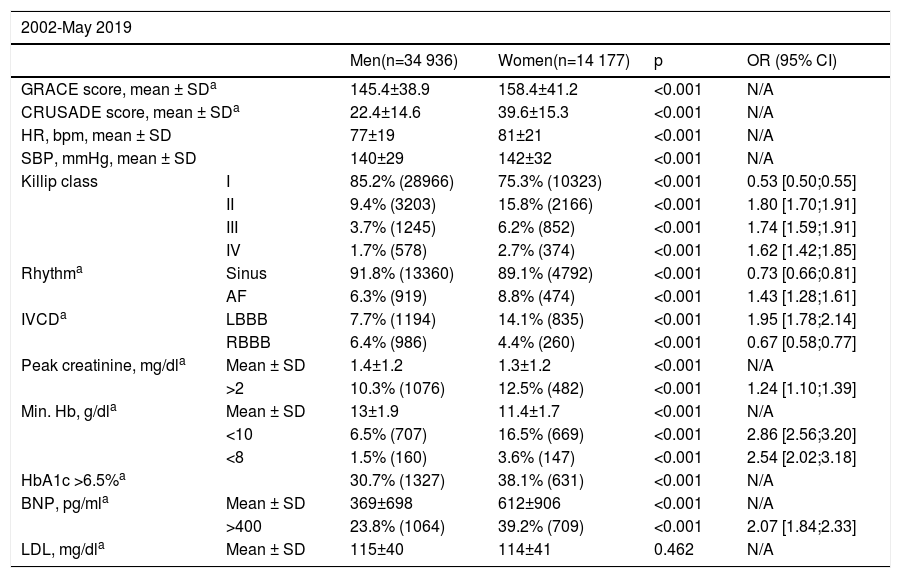
Based on the available clinical, laboratory, electrocardiographic and risk stratification data, women had a significantly higher risk of in-hospital death than men, with significantly higher GRACE scores (158.4±41.2 vs. 145.4±38.9, p<0.001), which represents a mean mortality risk of 20-30% (mortality risk with a GRACE score of 150-173). Furthermore, women were also at greater risk of major bleeding during hospital stay, as indicated by a mean CRUSADE score of 39.6±15.3 (vs. 22.4±14.6 in men, p<0.001), representing an 8.6% risk (moderate) compared to men, whose risk was estimated to be low (5.5%). In addition, as an indicator of severity of heart failure and risk of 30-day mortality after ACS, women were also less likely to be in Killip class I at admission or during hospital stay, the difference being statistically significant in all Killip classes, attributing greater severity to the female gender (Table 8). Women were also more likely to develop atrial fibrillation (8.8% vs. 6.3%, p<0.001), to have acute kidney injury or creatinine >2mg/dl (12.5% vs. 10.3%), and to have anemia (with statistically lower mean hemoglobin), as well as hemoglobin below 10g/dl and 8g/dl (16.5% and 3.6% vs. 3.6% and 1.5%, respectively, p<0.001 for both). Women were also more likely to fulfill criteria for a diagnosis of diabetes (glycated hemoglobin >6.5%) (38.1% vs. 30.7%, p<0.001), and to have higher brain natriuretic peptide levels (Table 8).
Parameters assessed during hospitalization.
| 2002-May 2019 | |||||
|---|---|---|---|---|---|
| Men(n=34 936) | Women(n=14 177) | p | OR (95% CI) | ||
| GRACE score, mean ± SDa | 145.4±38.9 | 158.4±41.2 | <0.001 | N/A | |
| CRUSADE score, mean ± SDa | 22.4±14.6 | 39.6±15.3 | <0.001 | N/A | |
| HR, bpm, mean ± SD | 77±19 | 81±21 | <0.001 | N/A | |
| SBP, mmHg, mean ± SD | 140±29 | 142±32 | <0.001 | N/A | |
| Killip class | I | 85.2% (28966) | 75.3% (10323) | <0.001 | 0.53 [0.50;0.55] |
| II | 9.4% (3203) | 15.8% (2166) | <0.001 | 1.80 [1.70;1.91] | |
| III | 3.7% (1245) | 6.2% (852) | <0.001 | 1.74 [1.59;1.91] | |
| IV | 1.7% (578) | 2.7% (374) | <0.001 | 1.62 [1.42;1.85] | |
| Rhythma | Sinus | 91.8% (13360) | 89.1% (4792) | <0.001 | 0.73 [0.66;0.81] |
| AF | 6.3% (919) | 8.8% (474) | <0.001 | 1.43 [1.28;1.61] | |
| IVCDa | LBBB | 7.7% (1194) | 14.1% (835) | <0.001 | 1.95 [1.78;2.14] |
| RBBB | 6.4% (986) | 4.4% (260) | <0.001 | 0.67 [0.58;0.77] | |
| Peak creatinine, mg/dla | Mean ± SD | 1.4±1.2 | 1.3±1.2 | <0.001 | N/A |
| >2 | 10.3% (1076) | 12.5% (482) | <0.001 | 1.24 [1.10;1.39] | |
| Min. Hb, g/dla | Mean ± SD | 13±1.9 | 11.4±1.7 | <0.001 | N/A |
| <10 | 6.5% (707) | 16.5% (669) | <0.001 | 2.86 [2.56;3.20] | |
| <8 | 1.5% (160) | 3.6% (147) | <0.001 | 2.54 [2.02;3.18] | |
| HbA1c >6.5%a | 30.7% (1327) | 38.1% (631) | <0.001 | N/A | |
| BNP, pg/mla | Mean ± SD | 369±698 | 612±906 | <0.001 | N/A |
| >400 | 23.8% (1064) | 39.2% (709) | <0.001 | 2.07 [1.84;2.33] | |
| LDL, mg/dla | Mean ± SD | 115±40 | 114±41 | 0.462 | N/A |
variable included only after October 2010.
AF: atrial fibrillation; bpm: beats per minute; BNP: brain natriuretic peptide; CI: confidence interval; Hb: hemoglobin; HbA1c: glycated hemoglobin; HR: heart rate; IVCD: intraventricular conduction delay; LBBB: left bundle branch block; LDL: low-density lipoprotein; Min.: minimum; N/A: not applicable; OR: odds ratio; RBBB: right bundle branch block; SBP: systolic blood pressure; SD: standard deviation.
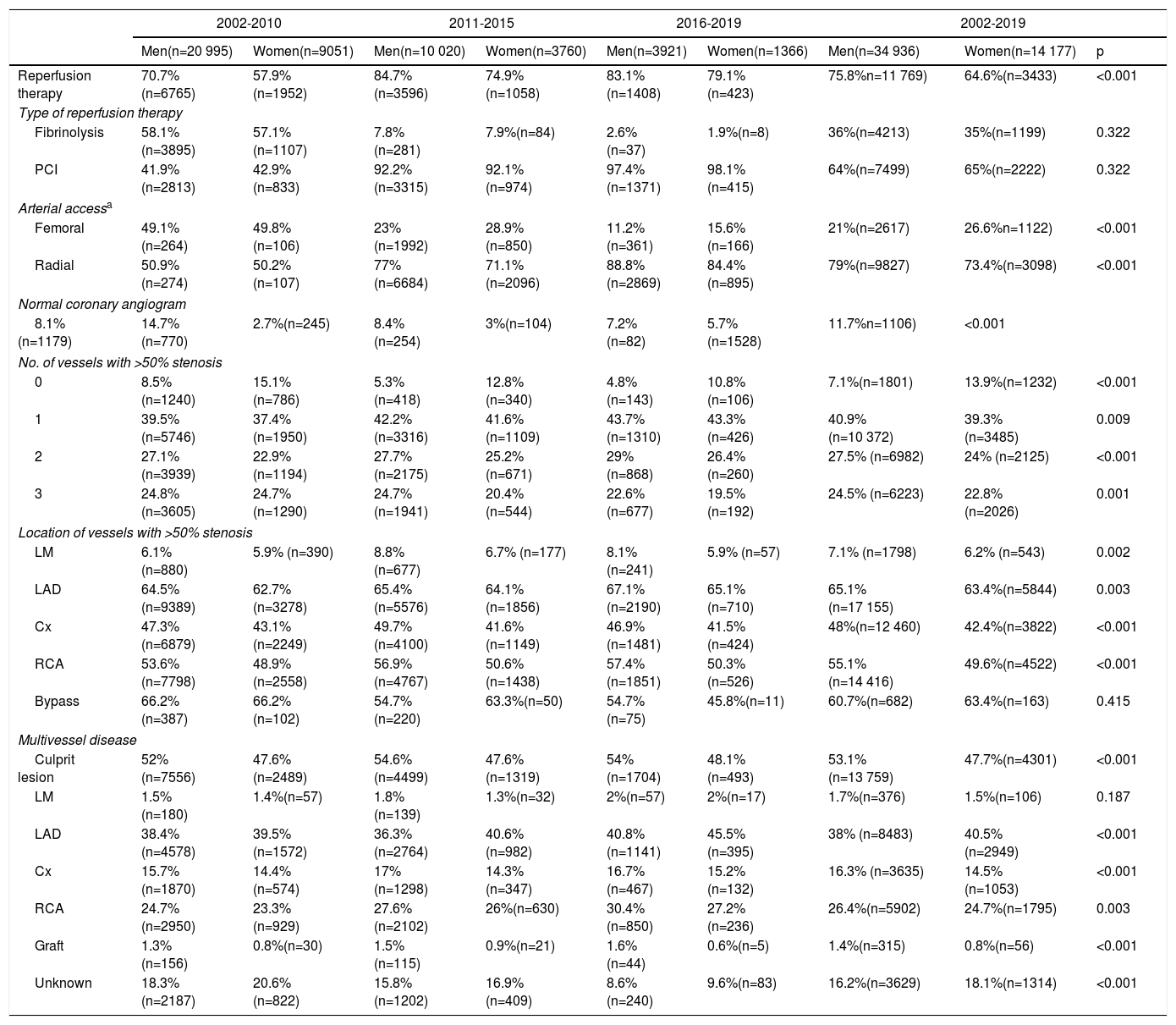
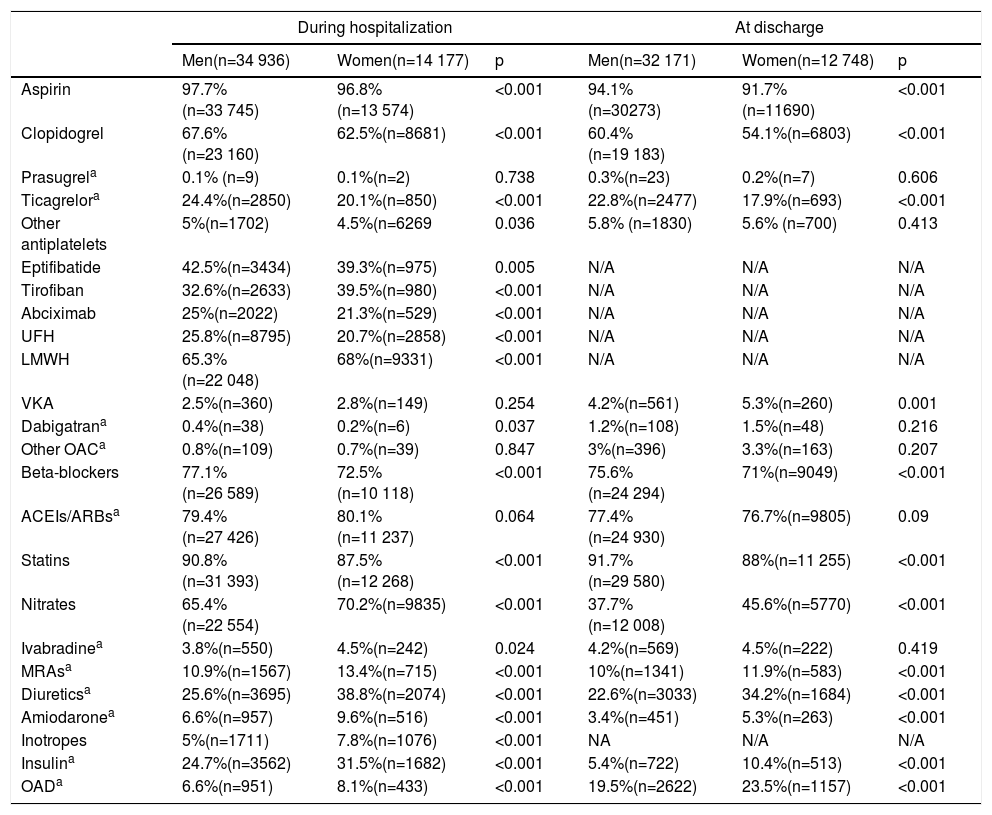
Analysis of reperfusion therapies in the overall ACS population shows that although their use increased over the three study periods, in general women had less access to both invasive and pharmacologic reperfusion therapies than men (p<0.001). When reperfusion was performed, no significant differences were observed between periods or the overall period analyzed, with less use of fibrinolysis and a clear dominance of primary angioplasty. For the latter, a difference can be seen regarding vascular access, with radial access used less frequently in women than in men (p<0.001) (Table 9). Women were more likely to have a normal coronary angiogram or coronary lesions with <50% luminal stenosis, and thus a final diagnosis other than ACS. Women were also less likely to have multivessel disease (two or three vessels); however, the culprit lesion was more difficult to identify in women (18.1% vs. 16.2%, p<0.001) (Table 9). Regarding pharmacological therapy during hospitalization, the situation was similar, women being less likely to receive guideline-recommended therapy, including aspirin, P2Y12 inhibitors, beta-blockers, and statins; however, based on the available data, it is impossible to be sure whether this difference is due to there being more potential diagnoses other than ACS in women compared with men. Women were more likely to receive more nitrates, mineralocorticoid receptor antagonists, diuretics, amiodarone, inotropes, insulin, and oral antidiabetic therapy during hospitalization, which can be interpreted as indicators of severity. The same tendency can be seen at hospital discharge, when women were less likely to be prescribed antiplatelet therapy with aspirin or P2Y12 inhibitors, beta-blockers, and statins. On the other hand, women were more likely to receive vitamin K antagonists, mineralocorticoid receptor antagonists, diuretics, amiodarone, insulin and oral antidiabetic therapy as outpatients (Table 10).
Reperfusion therapy and coronary angiography findings.
| 2002-2010 | 2011-2015 | 2016-2019 | 2002-2019 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Men(n=20 995) | Women(n=9051) | Men(n=10 020) | Women(n=3760) | Men(n=3921) | Women(n=1366) | Men(n=34 936) | Women(n=14 177) | p | |
| Reperfusion therapy | 70.7%(n=6765) | 57.9%(n=1952) | 84.7%(n=3596) | 74.9%(n=1058) | 83.1%(n=1408) | 79.1%(n=423) | 75.8%n=11 769) | 64.6%(n=3433) | <0.001 |
| Type of reperfusion therapy | |||||||||
| Fibrinolysis | 58.1%(n=3895) | 57.1%(n=1107) | 7.8%(n=281) | 7.9%(n=84) | 2.6%(n=37) | 1.9%(n=8) | 36%(n=4213) | 35%(n=1199) | 0.322 |
| PCI | 41.9%(n=2813) | 42.9%(n=833) | 92.2%(n=3315) | 92.1%(n=974) | 97.4%(n=1371) | 98.1%(n=415) | 64%(n=7499) | 65%(n=2222) | 0.322 |
| Arterial accessa | |||||||||
| Femoral | 49.1%(n=264) | 49.8%(n=106) | 23%(n=1992) | 28.9%(n=850) | 11.2%(n=361) | 15.6%(n=166) | 21%(n=2617) | 26.6%n=1122) | <0.001 |
| Radial | 50.9%(n=274) | 50.2%(n=107) | 77%(n=6684) | 71.1%(n=2096) | 88.8%(n=2869) | 84.4%(n=895) | 79%(n=9827) | 73.4%(n=3098) | <0.001 |
| Normal coronary angiogram | |||||||||
| 8.1%(n=1179) | 14.7%(n=770) | 2.7%(n=245) | 8.4%(n=254) | 3%(n=104) | 7.2%(n=82) | 5.7%(n=1528) | 11.7%n=1106) | <0.001 | |
| No. of vessels with >50% stenosis | |||||||||
| 0 | 8.5%(n=1240) | 15.1%(n=786) | 5.3%(n=418) | 12.8%(n=340) | 4.8%(n=143) | 10.8%(n=106) | 7.1%(n=1801) | 13.9%(n=1232) | <0.001 |
| 1 | 39.5% (n=5746) | 37.4% (n=1950) | 42.2% (n=3316) | 41.6% (n=1109) | 43.7% (n=1310) | 43.3% (n=426) | 40.9% (n=10 372) | 39.3% (n=3485) | 0.009 |
| 2 | 27.1% (n=3939) | 22.9% (n=1194) | 27.7% (n=2175) | 25.2% (n=671) | 29% (n=868) | 26.4% (n=260) | 27.5% (n=6982) | 24% (n=2125) | <0.001 |
| 3 | 24.8% (n=3605) | 24.7% (n=1290) | 24.7% (n=1941) | 20.4% (n=544) | 22.6% (n=677) | 19.5% (n=192) | 24.5% (n=6223) | 22.8% (n=2026) | 0.001 |
| Location of vessels with >50% stenosis | |||||||||
| LM | 6.1% (n=880) | 5.9% (n=390) | 8.8% (n=677) | 6.7% (n=177) | 8.1% (n=241) | 5.9% (n=57) | 7.1% (n=1798) | 6.2% (n=543) | 0.002 |
| LAD | 64.5%(n=9389) | 62.7%(n=3278) | 65.4%(n=5576) | 64.1%(n=1856) | 67.1%(n=2190) | 65.1%(n=710) | 65.1%(n=17 155) | 63.4%(n=5844) | 0.003 |
| Cx | 47.3%(n=6879) | 43.1%(n=2249) | 49.7%(n=4100) | 41.6%(n=1149) | 46.9%(n=1481) | 41.5%(n=424) | 48%(n=12 460) | 42.4%(n=3822) | <0.001 |
| RCA | 53.6%(n=7798) | 48.9%(n=2558) | 56.9%(n=4767) | 50.6%(n=1438) | 57.4%(n=1851) | 50.3%(n=526) | 55.1%(n=14 416) | 49.6%(n=4522) | <0.001 |
| Bypass | 66.2%(n=387) | 66.2%(n=102) | 54.7%(n=220) | 63.3%(n=50) | 54.7%(n=75) | 45.8%(n=11) | 60.7%(n=682) | 63.4%(n=163) | 0.415 |
| Multivessel disease | |||||||||
| Culprit lesion | 52%(n=7556) | 47.6%(n=2489) | 54.6%(n=4499) | 47.6%(n=1319) | 54%(n=1704) | 48.1%(n=493) | 53.1%(n=13 759) | 47.7%(n=4301) | <0.001 |
| LM | 1.5%(n=180) | 1.4%(n=57) | 1.8%(n=139) | 1.3%(n=32) | 2%(n=57) | 2%(n=17) | 1.7%(n=376) | 1.5%(n=106) | 0.187 |
| LAD | 38.4% (n=4578) | 39.5% (n=1572) | 36.3% (n=2764) | 40.6% (n=982) | 40.8% (n=1141) | 45.5% (n=395) | 38% (n=8483) | 40.5% (n=2949) | <0.001 |
| Cx | 15.7% (n=1870) | 14.4% (n=574) | 17% (n=1298) | 14.3% (n=347) | 16.7% (n=467) | 15.2% (n=132) | 16.3% (n=3635) | 14.5% (n=1053) | <0.001 |
| RCA | 24.7%(n=2950) | 23.3%(n=929) | 27.6%(n=2102) | 26%(n=630) | 30.4%(n=850) | 27.2%(n=236) | 26.4%(n=5902) | 24.7%(n=1795) | 0.003 |
| Graft | 1.3%(n=156) | 0.8%(n=30) | 1.5%(n=115) | 0.9%(n=21) | 1.6%(n=44) | 0.6%(n=5) | 1.4%(n=315) | 0.8%(n=56) | <0.001 |
| Unknown | 18.3%(n=2187) | 20.6%(n=822) | 15.8%(n=1202) | 16.9%(n=409) | 8.6%(n=240) | 9.6%(n=83) | 16.2%(n=3629) | 18.1%(n=1314) | <0.001 |
Cx: circumflex artery; LAD: left anterior descending artery; LM: left main; PCI: percutaneous coronary intervention; RCA: right coronary artery
Pharmacological therapy during hospitalization and at hospital discharge.
| During hospitalization | At discharge | |||||
|---|---|---|---|---|---|---|
| Men(n=34 936) | Women(n=14 177) | p | Men(n=32 171) | Women(n=12 748) | p | |
| Aspirin | 97.7%(n=33 745) | 96.8%(n=13 574) | <0.001 | 94.1%(n=30273) | 91.7%(n=11690) | <0.001 |
| Clopidogrel | 67.6%(n=23 160) | 62.5%(n=8681) | <0.001 | 60.4%(n=19 183) | 54.1%(n=6803) | <0.001 |
| Prasugrela | 0.1% (n=9) | 0.1%(n=2) | 0.738 | 0.3%(n=23) | 0.2%(n=7) | 0.606 |
| Ticagrelora | 24.4%(n=2850) | 20.1%(n=850) | <0.001 | 22.8%(n=2477) | 17.9%(n=693) | <0.001 |
| Other antiplatelets | 5%(n=1702) | 4.5%(n=6269 | 0.036 | 5.8% (n=1830) | 5.6% (n=700) | 0.413 |
| Eptifibatide | 42.5%(n=3434) | 39.3%(n=975) | 0.005 | N/A | N/A | N/A |
| Tirofiban | 32.6%(n=2633) | 39.5%(n=980) | <0.001 | N/A | N/A | N/A |
| Abciximab | 25%(n=2022) | 21.3%(n=529) | <0.001 | N/A | N/A | N/A |
| UFH | 25.8%(n=8795) | 20.7%(n=2858) | <0.001 | N/A | N/A | N/A |
| LMWH | 65.3%(n=22 048) | 68%(n=9331) | <0.001 | N/A | N/A | N/A |
| VKA | 2.5%(n=360) | 2.8%(n=149) | 0.254 | 4.2%(n=561) | 5.3%(n=260) | 0.001 |
| Dabigatrana | 0.4%(n=38) | 0.2%(n=6) | 0.037 | 1.2%(n=108) | 1.5%(n=48) | 0.216 |
| Other OACa | 0.8%(n=109) | 0.7%(n=39) | 0.847 | 3%(n=396) | 3.3%(n=163) | 0.207 |
| Beta-blockers | 77.1%(n=26 589) | 72.5%(n=10 118) | <0.001 | 75.6%(n=24 294) | 71%(n=9049) | <0.001 |
| ACEIs/ARBsa | 79.4%(n=27 426) | 80.1%(n=11 237) | 0.064 | 77.4%(n=24 930) | 76.7%(n=9805) | 0.09 |
| Statins | 90.8%(n=31 393) | 87.5%(n=12 268) | <0.001 | 91.7%(n=29 580) | 88%(n=11 255) | <0.001 |
| Nitrates | 65.4%(n=22 554) | 70.2%(n=9835) | <0.001 | 37.7%(n=12 008) | 45.6%(n=5770) | <0.001 |
| Ivabradinea | 3.8%(n=550) | 4.5%(n=242) | 0.024 | 4.2%(n=569) | 4.5%(n=222) | 0.419 |
| MRAsa | 10.9%(n=1567) | 13.4%(n=715) | <0.001 | 10%(n=1341) | 11.9%(n=583) | <0.001 |
| Diureticsa | 25.6%(n=3695) | 38.8%(n=2074) | <0.001 | 22.6%(n=3033) | 34.2%(n=1684) | <0.001 |
| Amiodaronea | 6.6%(n=957) | 9.6%(n=516) | <0.001 | 3.4%(n=451) | 5.3%(n=263) | <0.001 |
| Inotropes | 5%(n=1711) | 7.8%(n=1076) | <0.001 | NA | N/A | N/A |
| Insulina | 24.7%(n=3562) | 31.5%(n=1682) | <0.001 | 5.4%(n=722) | 10.4%(n=513) | <0.001 |
| OADa | 6.6%(n=951) | 8.1%(n=433) | <0.001 | 19.5%(n=2622) | 23.5%(n=1157) | <0.001 |
variable included only after October 2010.
ACEIs: angiotensin-converting enzyme inhibitors; ARBs: angiotensin II receptor blockers; LMWH: low molecular weight heparin; MRAs: mineralocorticoid receptor antagonists; OAC: oral anticoagulants; OAD: antidiabetic therapy; UFH: unfractionated heparin; VKA: vitamin K antagonist.
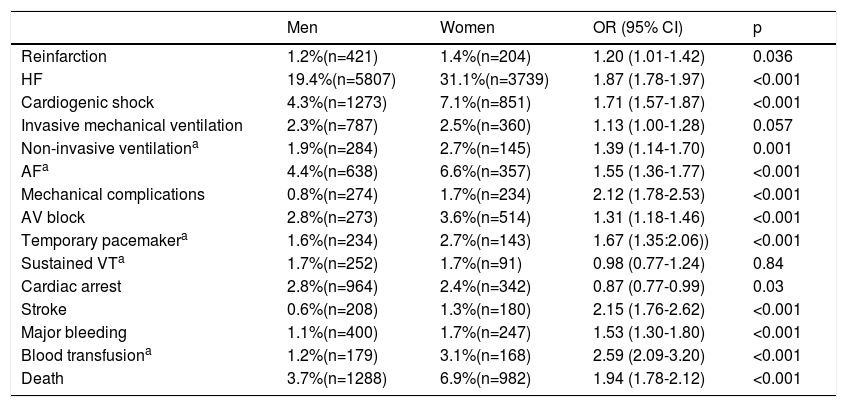
In this study, women were at greater risk for ACS-associated complications during hospitalization, with a significantly higher prevalence of development of heart failure (p<0.001), cardiogenic shock (p<0.001), mechanical complications (p<0.001) and need for non-invasive ventilation (p<0.001), arrhythmic events including atrial fibrillation (p<0.001), atrioventricular block and need for temporary pacing (p<0.001 for both) and cardiac arrest (p=0.03), ischemic and bleeding events including stroke (p<0.001), major bleeding (p<0.001), and need for blood transfusion (p<0.001) (Table 11). Left ventricular ejection fraction did not differ significantly between groups, even when divided into quartiles.
Complications during hospitalization.
| Men | Women | OR (95% CI) | p | |
|---|---|---|---|---|
| Reinfarction | 1.2%(n=421) | 1.4%(n=204) | 1.20 (1.01-1.42) | 0.036 |
| HF | 19.4%(n=5807) | 31.1%(n=3739) | 1.87 (1.78-1.97) | <0.001 |
| Cardiogenic shock | 4.3%(n=1273) | 7.1%(n=851) | 1.71 (1.57-1.87) | <0.001 |
| Invasive mechanical ventilation | 2.3%(n=787) | 2.5%(n=360) | 1.13 (1.00-1.28) | 0.057 |
| Non-invasive ventilationa | 1.9%(n=284) | 2.7%(n=145) | 1.39 (1.14-1.70) | 0.001 |
| AFa | 4.4%(n=638) | 6.6%(n=357) | 1.55 (1.36-1.77) | <0.001 |
| Mechanical complications | 0.8%(n=274) | 1.7%(n=234) | 2.12 (1.78-2.53) | <0.001 |
| AV block | 2.8%(n=273) | 3.6%(n=514) | 1.31 (1.18-1.46) | <0.001 |
| Temporary pacemakera | 1.6%(n=234) | 2.7%(n=143) | 1.67 (1.35:2.06)) | <0.001 |
| Sustained VTa | 1.7%(n=252) | 1.7%(n=91) | 0.98 (0.77-1.24) | 0.84 |
| Cardiac arrest | 2.8%(n=964) | 2.4%(n=342) | 0.87 (0.77-0.99) | 0.03 |
| Stroke | 0.6%(n=208) | 1.3%(n=180) | 2.15 (1.76-2.62) | <0.001 |
| Major bleeding | 1.1%(n=400) | 1.7%(n=247) | 1.53 (1.30-1.80) | <0.001 |
| Blood transfusiona | 1.2%(n=179) | 3.1%(n=168) | 2.59 (2.09-3.20) | <0.001 |
| Death | 3.7%(n=1288) | 6.9%(n=982) | 1.94 (1.78-2.12) | <0.001 |
Unadjusted in-hospital mortality was significantly higher in women, who had a 1.9-fold greater risk of dying during hospitalization (Table 11).
DiscussionCardiovascular disease (CVD) is the leading cause of death in both sexes worldwide. Each year, according to the 2017 European Cardiovascular Disease Statistics, CVD is responsible for 3.9 million deaths in Europe, accounting for 45% of all deaths, and is the leading cause of death in women in all except two countries. The largest gap in mortality by gender is found in the Baltic states, Slovenia and Romania, where the percentage of women dying from cardiovascular diseases is 13.5-17.4% higher than in men.6 Another European analysis from 2015 shows that the difference between the sexes is more marked regarding ischemic heart disease (IHD); however, unlike in all CVD, the mortality rate from IHD is 1.8 times higher in men.7 Our results show that in Portugal, although published data from the ProACS indicate that in-hospital mortality has declined steadily since 2002,8 in the period studied, among patients admitted to hospital with ACS women were more likely to die than men. This apparent difference in results may be due to the fact that official European data analyze overall mortality from IHD (which includes a spectrum of disease) over time, unlike our work, in which we assessed a single event in the continuum of IHD and associated in-hospital mortality. However, it should be borne in mind that this higher mortality is unadjusted for other variables, and in a report from China, in which unadjusted in-hospital mortality for women initially appeared to be higher, this was no longer the case after adjustment for clinical characteristics and acute treatments.9 A similar result was seen in a study on patients from the ProACS, in which after propensity score adjustment, gender was no longer a predictor of in-hospital mortality.2
When traditional cardiovascular risk factors were analyzed, there was a higher prevalence of hypertension, dyslipidemia, diabetes and obesity and a growing prevalence in the periods studied of smoking, diabetes and dyslipidemia in women, showing that the efforts of the health community to call attention to the need for better risk factor control are still insufficient, since despite the growing number of patients at hospital admission who are, for example, prescribed antihypertensive and statin therapy, these patients are still lower in number than those diagnosed with ACS à despite the growing number of patients that at hospital admission are, for example, treated with anti-hypertensive therapy and statins; those are still in lower number than those with the diagnosis.
Data from the US Centers for Disease Control and Prevention show that women are less likely to be prescribed a statin, and that their therapeutic adherence is also low.10,11 In terms of secondary prevention, a meta-analysis performed by the Cholesterol Treatment Trialists’ Collaboration with 170 000 patients from statin trials shows that a reduction of 38.66mg/dl in LDL cholesterol is associated with a 22% relative risk reduction in major vascular events, the results being similar for both sexes.12 Despite this evidence, in our study women were undertreated with statins both during hospitalization and at discharge, even though the prevalence of dyslipidemia is higher in women. It is unclear whether this is due to a higher prevalence of adverse effects of statins in women than in men, but it probably signals the need for greater physician and patient awareness.
Hypertension is more strongly associated with MI in women than in men.13 Furthermore, pregnancy-related complications such as pre-eclampsia and gestational hypertension are associated with a greater long-term risk of developing hypertension and CVD, and postmenopausal women are also more likely to have a non-dipper pattern, which has been associated with worse cardiovascular outcomes and target organ damage.14,15 There is no evidence that antihypertensive therapy has a different efficacy or safety profile in women, even though most trials do not analyze their data by gender. In our study, we found no differences in the prescription of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers (ACEIs/ARBs) between genders, either during hospitalization or at discharge, but the rate of beta-blocker prescription was higher in men at both times. The prescription of other antihypertensive therapy during hospitalization or at discharge is unknown.
Compared to women without diabetes, those with diabetes have a three-fold higher risk of fatal CAD, and their risk is also higher than in men with diabetes. Women with diabetes have a more aggressive profile of CAD, related to greater impairment of endothelium-dependent vasodilation and greater likelihood of hypercoagulable states, atherogenic dyslipidemia, and metabolic syndrome. Considering that the harmful effects of glucose begin to occur at blood glucose levels lower than those currently accepted for a diagnosis of diabetes, the transition from normoglycemia to glucose intolerance and diabetes may be more detrimental in women.16–18 Although there was no difference in the rate of prescription of insulin or oral antidiabetic therapy between the sexes before hospital admission, during hospitalization and at hospital discharge there were significant differences, combined with the underdiagnosis of diabetes in outpatients and/or undertreatment.
Smoking is the most important preventable cause of MI in women, and a major risk factor for women aged <55 years, leading to an increase in the risk of MI. Although there has been an overall reduction in the use of tobacco products in the US, this decline is considerably less marked in women,19,20 which agrees with our data.
The prevalence of obesity is higher in women, as well as the impact that this risk factor has on the development of CAD. In the Framingham Heart Study, obesity increased the relative risk of CAD by 64% for women (vs. 46% for men). Despite this knowledge, the prevalence of obesity in women with ACS is still higher than in men.21 Additionally, women have other non-traditional risk factors that are not analyzed in our study, such as depression, premature labor, radiotherapy for breast cancer, and many chemotherapy drugs.
It is increasingly recognized that CAD in women is not restricted to obstructive atherosclerotic coronary disease, but also includes microvascular and endothelial dysfunction, coronary vasomotor abnormalities, and spontaneous coronary artery dissection. This extended spectrum of a single disease creates difficulties not only in diagnosis but also in treatment, resulting in women frequently being underdiagnosed and undertreated if they do not present with the typical pattern of obstructive coronary atherosclerosis.22 This is a possible explanation for our finding of a significant difference between the sexes regarding coronary angiograms with normal coronary arteries or with <50% stenosis, which reflects a well-known paradox: women had a higher prevalence than men of stable angina pre-hospital admission (29.1% vs. 23.8%, p<0.001) and less likelihood of obstructive CAD on coronary angiography (5.7% vs. 11.7%, p<0.001) but a worse prognosis (in-hospital mortality 6.9% vs. 3.7%, p<0.001). In addition to this, pathology and image studies have shown that women have smaller coronary arteries, a more diffuse pattern of atherosclerosis with fewer obstructive lesions, and a greater incidence of plaque erosion as the substrate of acute thrombosis.23 This paradox of less obstructive CAD with worse outcomes can, at least in part, be explained by the connection between microvascular disease and coronary atherosclerosis; in addition, there is increasing evidence that more extensive non-obstructive CAD is associated with a similar rate of adverse cardiovascular outcomes to obstructive CAD.24
With regard to clinical presentation of ACS, our results confirm what was previously known: women more frequently have atypical symptoms, even though the most common presenting symptom is still chest pain.25,26 This gender difference in clinical presentation affects the timely identification of ischemic symptoms, appropriate triage, and therapeutic approach, leading to delays in revascularization and higher mortality. In a study in France, all the timings were longer in women; in-hospital morbidity and mortality rates were also significantly higher, and rates of prescription of guideline-recommended therapies were lower.27 Our results are in line with these findings and those of similar studies, and all the timings analyzed were longer in women, regardless of whether the starting point was symptom onset, FMC or arrival at the door. However, comparing the two more recent periods, FMC-to-needle, door-to-needle and symptom onset-to-balloon times improved in women, unlike in men, and in both sexes there were improvements in FMC-to-balloon, door-to-wire crossing, door-to-balloon, and FMC-to-wire crossing times. On the other hand, in these two more recent periods, longer times were observed in women from symptom onset to admission, wire crossing and needle, as well as from FMC to admission, leading to the conclusion that overall, although after FMC and/or hospital admission the path to treatment is becoming more efficient, the female population do not seem to be aware of the need for timely recognition of the signs and symptoms of MI, leading to greater delays, particularly in patient-dependent times. A similar discrepancy has been observed in other countries, including New Zealand, Australia, France and the USA.27–29 Another important point is the paradoxically greater delays in STEMI quality indices when the period 2002-2010 is compared to the two more recent periods. The mortality benefit achieved with primary PCI in STEMI patients is reduced by treatment delays,30 and mortality fell between these periods.8 This paradox was addressed in a Portuguese study from 2017,8 in which the authors state that, while there have been improvements in centers with a catheterization laboratory, with the proportion of patients with door-to-balloon time <60min rising from 52.5% to 73.5% (86.1% <90min), in centers without PCI facilities, the timings vary widely over the years, and were <60min in only 14.6%, <90min in 22.4% and <120min in 36.5%. In addition, there was considerable variability in the first years of the registry in centers without PCI facilities, associated with the smaller number of patients in these groups. This variability in the first years of the registry and the differences between centers with and without PCI facilities may be partly responsible for the paradox.
The high risk profile of women undergoing primary angioplasty, in terms of both ischemic risk (as shown by the GRACE score) and bleeding risk (as shown by the CRUSADE score), is reflected in a higher proportion of no or non-significant coronary lesions in our study, less extensive CAD and a lower prevalence of multivessel disease on coronary angiography in women compared with men. These findings are similar to those of a previous study in which the authors showed that despite the higher risk profile of women, there were no differences between the sexes in the extent of coronary disease or the prevalence of multivessel disease.2 It should be borne in mind, however, that this risk profile is essentially a clinical assumption, considering that in ACS little is known regarding the prognostic factors for adverse outcomes in women, and, although several risk scores such as GRACE and TIMI are commonly used, these were developed based on populations of which two-thirds were male, and so their performance in women is not well established.22
Despite the clear recommendation in the guidelines for radial access as the preferred mode of access, and the higher bleeding risk of women, our data indicate that this arterial route is less used in women, even though a substudy of the MATRIX trial showed that women have greater risk of severe bleeding and access complications, and that radial access is an effective way of reducing these complications.31
Even after adjusting for factors like age, comorbidities and disease severity, several studies have shown that women are less likely to be given recommended therapies either at hospital admission or at hospital discharge, including beta-blockers, ACEIs/ARBs, and statins.27,32,33 Our results indicate that for ACEIs/ARBs the prescription rate is similar to men (unlike statins and beta-blockers), which itself may represent under-prescription, considering the higher risk profile of women, as demonstrated by the fact that women have more complications, such as sustained VT or the need for non-invasive ventilation, even though they have less extensive CAD.34 Factors that may contribute to this finding in women are their higher rates of diabetes, hypertension, and obesity, a higher prevalence of outpatient HF, delays between symptom onset and reperfusion therapy, a higher prevalence of acute kidney injury, and the fact that they may less frequently be offered reperfusion therapy and medication for secondary prevention.
LimitationsThe observational nature of this study means that we cannot exclude the existence of possible additional confounders that are not identified or accounted for in the data analysis. Furthermore, although the data from ProACS is largely representative of the various geographic regions of Portugal, it is not possible to infer conclusions about the country as a whole. As the registry is voluntary, it is not possible to ensure that patients were included consecutively; some ACS patients were not hospitalized in cardiology departments and therefore are not included in the database; and only patients who were admitted alive are included, and so a proportion of patients with fatal complications before admission were omitted from the analysis. In addition, the number of records has decreased in recent years, which may have led to bias when comparing periods, and as the registry is voluntary, some data may have been missed, leading to data inconsistencies. Another limitation of our study is that some data were only collected after October 2010, and so a considerable number of patients did not have all of their parameters recorded.
ConclusionThe number of women with CAD is increasing; however, compared with men, this disease is still underdiagnosed and undertreated, and women have less access to revascularization and optimal medical therapy. Although in the overall population a significant increase in the use of PCI was observed, there is still a statistically significant difference in its use between the sexes; women are less likely to receive guideline-recommended therapy in the context of secondary prevention, even in the most recent time period; and in-hospital complications and unadjusted mortality are still higher in women, despite improvements in overall mortality over the years. These findings are based on a voluntary registry and the inherent limitations should be borne in mind.
Greater awareness of both patients and health professionals is urgently needed to change the way ACS is treated in women.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors thank the Portuguese National Cardiology Data Collection Center (CNCDC), particularly Dr. Adriana Belo, for their help in the statistical treatment of the data.