Coronary artery disease rarely manifests itself in the first decades of life, which explains why this population is underrepresented in clinical studies. The mechanisms and natural history of the disease seem to differ between this population and older patients. Recent studies suggest a more rapid disease progression in youth, presenting more unstable atherosclerotic plaques, although this correlation has yet to be proven. In this paper, we present the case of a 41-year-old man who presented with a non-ST elevation myocardial infarction, with percutaneous coronary intervention of the culprit lesion (70-90% lesion at bifurcation of the circumflex artery with the first marginal obtuse artery and a sub-occlusive lesion of the ramus intermedius). There was also a non-significant lesion (estimated at 30%) located in the left anterior descending coronary artery. Ten days after discharge, the patient suffered another non-ST elevation myocardial infarction. The coronary angiography revealed a surprising sub-occlusive lesion of the left anterior descending coronary artery. Regarding this case, the authors reviewed the literature on the pathophysiology of rapidly progressive coronary artery disease and the approach for non-significant lesions in patients with acute coronary syndrome, especially in the younger population.
A doença coronária de natureza aterosclerótica raramente se manifesta nas primeiras décadas de vida, encontrando-se assim esta população muito pouco representada nos estudos de larga escala. Os mecanismos e a história natural da doença coronária nesta população são diferentes da população mais idosa. Estudos recentes sugerem uma mais rápida progressão da doença nos indivíduos jovens, os quais apresentam placas ateroscleróticas com maior instabilidade. A correlação entre ambos os factos permanece por esclarecer. No presente trabalho, descreve-se o caso clínico de um homem que, aos 41 anos, apresenta a primeira manifestação de doença coronária sob a forma de enfarte agudo do miocárdio sem supradesnivelamento do segmento ST, tendo realizado tratamento percutâneo das artérias culpadas (lesão 70-90% em bifurcação da artéria coronária circunflexa com primeira obtusa marginal e lesão suboclusiva de ramus intermédio). Registou-se também uma lesão angiograficamente não significativa, estimada em cerca de 30% localizada na artéria descendente anterior. Dez dias após alta, o doente sofreu novo enfarte agudo miocárdio sem supradesnivelamento do segmento ST. Repetindo o estudo angiográfico, este revelou uma surpreendente lesão suboclusiva na artéria descendente anterior, a qual não tinha sido intervencionada. A propósito deste caso clínico, os autores fazem uma revisão da literatura relativa à fisiopatologia da progressão rápida de lesões coronárias e à abordagem de lesões não significativas em doentes com síndroma coronária aguda, especialmente na população mais jovem.
change
body mass index
blood pressure
body surface area
cardiovascular risk factors
diastolic blood pressure
electrocardiogram
fat mass
global longitudinal strain
heart rate
interventricular septum
left atrium
left ventricle
left ventricular diastolic diameter
left ventricular ejection fraction
left ventricular posterior wall
muscle mass
relative wall thickness
systolic blood pressure
tricuspid annular plane systolic excursion
transthoracic echocardiography
The cause of rapid atherosclerosis progression in the coronary tree with no vascular lesion that exposes the subendothelial tissue to contact with blood components is unclear. It may be associated with coronary vasospasm, prior complex lesions and/or inflammatory markers.1–3 There is no universal definition of rapid progression of atherosclerosis. However, most studies that describe the phenomenon use the following definition: (I) ≥10% diameter reduction of at least one preexisting stenosis ≥50%, (II) ≥30% diameter reduction of a preexisting stenosis <50%, and (III) progression of a lesion to total occlusion within a few months.4 Rapid coronary artery disease (CAD) progression has been described in young patients, and could be explained by genetic phenomena,5 increased pro-inflammatory activity and, in some cases, by the increased vulnerable plaques.6,7
Acute CAD tends to occur in young adults, with smoking being the most common classic cardiovascular risk factor.8 The pathophysiology and aggressiveness of the disease in this age range have specific features that may cause unique concerns.9–11 The treatment strategy to use for non-culprit atherosclerotic plaques in acute coronary syndrome (ACS) is unclear in the current guidelines, which give indications only for ST-elevation myocardial infarction (STEMI).12,13 Recent studies on non-ST-elevation myocardial infarction (NSTEMI) patients suggest that multivessel revascularization may be safer in NSTEMI patients than in STEMI patients.14,15 The American Heart Association (AHA) recommendations give a IIb-B indication for complete revascularization of patients with NSTEMI and multivessel CAD, emphasizing that this is controversial and needs further research.16 In Europe, there are no clear recommendations for identifying non-culprit plaques in unstable angina/NSTEMI. Given accelerated CAD progression in the younger population, the need for recommendations is even more pertinent. This is due to the fact that the younger population most often survives acute episodes,17 but has greater exposure to another episode in the near future.17–19
We describe a case of CAD in a young adult, which manifested as NSTEMI with recurrence 10 days later, despite appropriate pharmacological and revascularization therapy.
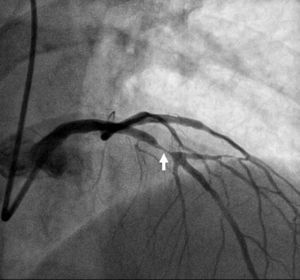
Case reportThe patient is a 41-year-old male with a history of hypertension, smoking (20 pack-years) and dyslipidemia (prior tests showed an LDL of 107 mg/dl), with no family history of coronary artery disease. He had an NSTEMI on March 4, 2016 as the first symptom of coronary artery disease. He underwent cardiac catheterization around 12 hours after admission to the hospital. The procedure revealed the presence of coronary artery disease extensively involving several segments of the circumflex artery (Cx), with 50% ostial stenosis associated with a 70-90% lesion at the bifurcation to the outlet of the first obtuse marginal branch (OM1), as well as a 70-90% lesion in the ramus intermedius. A mild lesion was found in left anterior descending artery (LAD), with less than a 30% reduction in the lumen (Figure 1). During the same procedure, angioplasty was performed on the Cx/OM1 and ramus intermedius lesions with placement of a drug-eluting stent in each lesion, with good angiographic result and no complications. No further ischemic events were recorded during hospital stay. The patient was discharged three days after the procedure, with a peak troponin I value of 0.88 ng/ml (normal value <0.04) and a peak CRP value of 4.3 mg/l (normal value <5.0). His outpatient medication was aspirin 100 mg once daily, perindopril 5 mg/amlodipine 5 mg once daily, carvedilol 6.25 mg twice daily and atorvastatin 20 mg once daily. Ticagrelor 90 mg twice daily was also recommended, which the patient refused due to financial constraints, so he was medicated with clopidogrel 75 mg once daily. The only significant transthoracic echocardiography finding was hypokinesis of the distal segment of the inferolateral wall, with preservation of left ventricular systolic function (calculated ejection fraction: 55-60%).
Coronary angiography with a 30% lesion in the middle segment of the LAD (white arrow). A circumflex artery (Cx) with 50% ostial stenosis, 70-90% lesion at the bifurcation to the outlet of the first obtuse marginal branch (OM1), as well as a 70-90% lesion in the ramus intermedius were found.
On March 12, 2016, the patient was readmitted to the hospital due to an episode of NSTEMI. He underwent another catheterization procedure around 12 hours after admission, which showed normal patency of the previously treated vessels with no signs of restenosis in the stents previously implanted. A new severe sub-occlusive lesion with abundant thrombotic material was found in the left anterior descending (LAD) artery. A lesion with a lumen reduction of about 30% was also identified in the same segment (Figure 2). Intracoronary nitrate administration ruled out vasospasm. Angioplasty of this new lesion was performed during the same procedure, with implantation of a drug-eluting stent. Abciximab was used as supplemental antithrombotic therapy. In the hours following the procedure, a peak troponin value of 0.30 pg/ml (normal value <0.04 pg/ml), a peak BNP value of 59 mg/ml and a peak CRP value of 18.6 mg/l (normal value <5.0) were recorded. Thyroid function was normal and thrombophilia testing was negative. The patient remained electrically and hemodynamically stable, maintaining sinus rhythm at all times. He was discharged three days later with instructions to increase to atorvastatin dose to 80 mg. The other outpatient medication remained unchanged. The echocardiography performed prior to discharge was comparable to the previous one, with no new alterations in motility and no deterioration of ventricular function.
DiscussionThis article presents the case of a male patient with major cardiovascular risk factors and initial symptoms of coronary artery disease at a young age. He presented with myocardial infarction (MI) and several coronary lesions. After percutaneous intervention of what appeared to be the culprit lesions and initiation of pharmacological therapy, another acute episode occurred a few days later. The second angiography showed a rapid change in an untreated vessel, a very unusual occurrence, which is why it merits attention. To our knowledge, there are no reported cases of such early reinfarction not associated with treatment failure or complications.
It is currently believed that most CAD symptoms occurring at a young age (<45-55 years) result from the acceleration of the same progressive atherosclerosis that occurs at elderly ages.11 Other causes, such as thrombophilia, vasospasm or autoimmune diseases, although more common in the elderly, are not the main cause of CAD in young adults.20,21 Intravascular ultrasound performed in young heart donors has shown the presence of atherosclerotic coronary plaque in one of every six adolescents aged 13-19 years,22 which demonstrates the presence of subclinical disease from very young ages. An individual with acute coronary syndrome at a young age also has a greater likelihood of progression of non-culprit coronary lesions, which may be explained by polymorphisms that form the basis of the early manifestation of coronary artery disease.6,23 Traditional cardiovascular risk factors explain 90% of the overall population attributable risk, and are even more decisive in young patients.24 Smoking and dyslipidemia, considered to be the most significant risk factors in young individuals,5–26 and hypertension – with particular significance in young adult smokers27 – will play a pivotal role in the early development of MI. A metabolic profile favoring accelerated disease progression is preserved even immediately after smoking cessation.28 However, non-traditional risk factors also play an important role in each patient's risk of progression. Elevated homocysteine levels have been found in cardiovascular disease patients,29 although their role as an independent risk factor is still unclear.30,31 Thrombophilia and inflammatory activity seem to play an important role, especially in the younger population,32,33 and should be the focus of further large-scale studies.34 Several studies are underway, especially in the area of chronic inflammatory diseases. These aim to clarify the usefulness of anti-inflammatory effects on the cardiovascular risk of these patients.5,35 The effects of dyslipidemia as an inflammatory modulator, the change in monocyte production, and its association with CAD instability have also been recently postulated.33
The use of drugs that stabilize atherosclerotic plaques is even more essential in young adults with CAD, regardless of whether or not lipid values are within therapeutic targets. In this case, the initial use of submaximal statin doses may not enable adequate CAD stabilization. In addition to the known efficacy of statins, in the future, PCSK9 inhibitors may also play an important role here, given the marked reduction in cholesterol they achieve. Moreover, they may, depending on the forthcoming results from some clinical studies, contribute to a radical change in standard practice.36–38 The recent Global Assessment of Plaque Regression With a PCSK9 Antibody as Measured by Intravascular Ultrasound (GLAGOV) study demonstrated plaque regression and greater change in atheroma volume in patients with angiographic evidence of coronary lesions after the use of evolucumab for 76 weeks, in combination with statins.38
CAD is a panvascular disease with a high prevalence of unstable lesions, even in arteries with apparently insignificant, non-culprit lesions.9 In this case, the rarity of the ultra-rapid progression between the two events is a sign that the underlying coronary artery disease is very unstable. The elevated CRP in the second event further suggests that the underlying pathophysiology is partly associated with inflammatory phenomena, more frequently manifested in young patients, which facilitate plaque instability. Several studies suggest that pro-inflammatory status, assessed through circulating inflammatory markers such as endothelin2 or C-reactive protein,39 is predictive of instability and rapid progression of the underlying coronary artery disease.33,34 In these studies, there was no difference in prevalence with regard to traditional cardiovascular risk factors between the population with rapid progression and the population that progressed, in the short term, with no complications.2,3 This same pathophysiology seems to correlate rapid disease progression with the increased instability of atherosclerotic plaques in young patients.2 However, targeted studies to answer this question have not yet been conducted.11
The rarity of events associated with arteries with angiographically insignificant stenosis (<50%) means that there are no clear indications for their treatment when they are identified during an acute coronary event. Fractional flow reserve (FFR) assessment has been studied in this context, but always in plaques with stenoses with a greater than 50% lumen reduction.40,41 The recent Compare-Acute study favors the use of FFR in STEMI patients with multivessel disease.42 Studies with intravascular imaging assessment have shown that ACS patients have atherosclerotic plaques in non-culprit coronary arteries with greater instability indexes than patients with no history of acute events.43 Complete intravascular imaging assessment of the coronary trees of these patients revealed multiple ruptures and fissures in non-obstructive plaques in non-culprit arteries.44,45 The importance of coronary CT angiography for assessing the total calcium score may also play an important role in predicting CAD instability.7,46,47
The concept of a single vulnerable plaque has long been questioned and somewhat abandoned, with the focus having progressed to “vulnerable patients”.48–50 The entire coronary tree, regardless of the histopathological structure of the lesions, has more or less inflammatory and pro-thrombotic activity, which translates into more or less vulnerability for the occurrence of acute events.49,51 Prospective studies have revealed that even plaques with a thin capsule and high lipid content, traditionally defined as vulnerable, may not in fact be unstable, and are therefore not a good risk marker.52 Identifying vulnerable CAD may affect treatment, requiring a more aggressive approach with closer monitoring and greater control of all of the patient's risk factors.53 The paper recently published by A. Arbab-Zadeh and V. Fuster suggests that identifying vulnerable CAD may enable identifying patients at greater risk, which may be indicated for new, more aggressive treatments,50 or which may be relevant for future clinical research.50,51,53 Approximately 70-80% of ACS patients have plaque ruptures in non-culprit vessels, justifying the idea of multiculprit disease, creating some evidence to consider complete revascularization in these cases.44 FFR use in STEMI in a patient with multivessel disease42 and FFR integration with tissue characterization by intravascular imaging may be a means for identifying future high-risk cases to prevent events similar to those presented here.54
ConclusionsThis case supports considering ACS to be a panvascular disease, in which the overall vulnerability of the CAD may be more relevant than the specific characteristics of each individual plaque, especially in the case of non-obstructive plaque. Young adults, typically associated with a better prognosis, have characteristics that promote accelerated progression, and their pathophysiology may also explain the greater CAD instability in this population. The best prognosis in the short term is not found in the long term,18 with five-year mortality rates of around 8.5% and 15-year mortality rates of 30%.17,21 As such, aggressively controlling all modifiable risk factors is crucial for the medium-to-long-term reduction of events. In contrast, in the short-term, the treatment of non-culprit lesions lacks clear recommendations; therapy to stabilize the atherosclerotic disease therefore plays a key role. Identifying the total atherosclerotic burden and correlating it with systemic factors that alter disease progression, such as inflammatory or coagulation abnormalities, will be crucial to determine the actual CAD vulnerability.51 The lack of scientific evidence in this field is the main impediment, and more clinical research is needed.
In this case, the authors believe the second coronary event to likely be due to an aggressive and unstable panvascular disease. Therefore, and although the first manifestation of CAD was an NSTEMI with clearly culprit plaques in the circumflex artery, the assessment of the remaining CAD was not aimed at clarifying its degree of instability, so the second event would be explained by a potential plaque rupture triggering the common thrombotic complications.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Montenegro Sá F, Ruivo C, Graça Santos L, Antunes A, Soares FC, Baptista J, et al. Progressão ultrarrápida de doença coronária ou placa instável não detetada? Rev Port Cardiol. 2018;37:259–264.