We sought to define trends in AF prevalence and its medical management using recent data based on data from two cross-sectional studies performed in a European country in 1999 and 2009.
MethodsCARDIOTENS 1999 and CARDIOTENS 2009 were two observational, cross-sectional, multicenter studies. Patients were recruited in from primary care and cardiology outpatient clinics. A total of 32 051 and 25 137 subjects were analyzed in the two studies, 1540 and 1524 of them, respectively, diagnosed with AF.
ResultsOver the course of the study period there was an increase in the prevalence of AF (from 4.8% to 6.1%), mainly due to the higher prevalence of AF in patients aged over 70 years (24.7% vs. 37.1%). Furthermore, patients with AF had a higher prevalence of hypertension (64.9% vs. 87.0%), diabetes (19.0% vs. 37.4%), heart failure (30.8% vs. 34.8%), coronary artery disease (23.0% vs. 25.8%) and previous stroke (1.5% vs. 8.9%). An overall increase in prescription of antithrombotic/antiplatelet therapy was observed (33.0% vs. 62.7% and 31.0% vs. 38.2% respectively); the difference observed in 1999 between prescription of oral anticoagulation by general practitioners and cardiologists was not seen in the later study. Differences in prescription of angiotensin-converting enzyme inhibitors (28.0% vs. 40.7%), angiotensin receptor blockers (10.0% vs. 40.0%), beta-blockers (14.0% vs. 41.5%) and calcium channel blockers (21.0% vs. 34.9%) were also identified.
ConclusionsThe number of patients with AF and a higher risk for thromboembolic events increased over the last 10 years. More aggressive antithrombotic treatment has been observed, especially in older patients.
Procuramos definir as tendências prevalentes de fibrilhação auricular (FA) e o tratamento médico utilizando dados recentes, colhidos de dois estudos transversais realizados num país europeu entre 1999 e 2009.
MétodosCARDIOTENS 1999 e CARDIOTENS 2009 são dois estudos observacionais, transversais multicêntricos. Os pacientes foram recrutados de clínicas de ambulatório dirigidas por generalistas e cardiologistas. Um total de 32 051 e de 25 137 indivíduos foram analizados; 1 540 e 1 524 dos quais foram diagnosticados com FA.
ResultadosDurante a realização do nosso estudo houve um aumento na incidência de FA (de 4,8% a 61,%) sobretudo devido à elevada prevalência de FA em pacientes com mais de 70 anos de idade (24,7% versus 37,1%). Para além disso doentes com FA revelam mais tendência para hipertensão (64,9% versus 87,0%), diabetes mellitus (19,0% versus 37,4%), insuficiência cardíaca (30,8% versus 34,8%), doença coronária (23% versus 25,8%) e acidente vascular cerebral prévio (1,5% versus 8,9%). No que se refere a terapia antitrombótica/antiplaquetária, foi observado um aumento generalizado na sua prescrição (33,0% versus 62,7% e 31,0% versus 38,2% respetivamente). Sobre este assunto, a diferença de prescrição de anticoagulantes orais observada em 1999 entre os generalistas e cardiologistas não se verifica atualmente. Diferenças nos agentes inibidores da enzima de conversão da angiotensina (28,0% versus 40,7%), bloqueadores recetores da angiotensina (10,0% versus 40,0%), beta-bloqueantes (14,0% versus 41,5%) e bloqueadores dos canais de cálcio (21,0% versus 34,9%) foram igualmente identificadas.
ConclusõesO número de pacientes com FA e eventos trombo-embólicos com risco mais elevado aumentou ao longo da última década. Um tratamento antitrombótico mais agressivo foi observado sobretudo na população mais idosa.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia in clinical practice.1,2 What was defined in the past as a simple arrhythmia characterized by irregularly irregular heartbeats is now accepted as a common and rapidly growing clinical problem and as a disease entity. Few previous studies have reported trends in the prevalence3–5 and medical management of AF in the last 10 years in a European country, specifically regarding oral anticoagulation, which should reflect the recommendations of the European guidelines.
Against this background, we sought to define trends in AF prevalence and its medical management based on data from two cross-sectional studies performed in a European country at an interval of 10 years (1999 and 2009).
MethodsStudy designCARDIOTENS 19996 and CARDIOTENS 20097 were two observational, cross-sectional, multicenter studies designed by the Hypertension Section of the Spanish Society of Cardiology with the aim of describing the prevalence and degree of control of hypertension and other cardiovascular risk factors in Spain. Both studies recruited patients from primary care and cardiology outpatient clinics. Inclusion criteria were age ≥18 years, availability of clinical records and previous cardiovascular diagnoses, and provision of written informed consent. Exclusion criteria were illegal drug use and refusal to give informed consent. A total of 1159 physicians were selected in the CARDIOTENS 1999 study and 885 in CARDIOTENS 2009 (79.0% and 89.1% were general practitioners and 21.0% and 10.9% cardiologists, respectively). In CARDIOTENS 1999 all outpatients were seen on the same day in both primary care and cardiology settings. In CARDIOTENS 2009, every physician recruited the first six patients on five consecutive days. A total of 32051 and 25137 subjects constituted the final sample of each registry; 1540 and 1524, respectively, had a current or previous history of AF and entered this substudy.
Definition of variablesA patient was identified as having AF if the records included either a medical report or an electrocardiogram confirming the diagnosis. Hypertension was defined, in accordance with the ESC/ESH guidelines8,9 in force at the time of the study, as two determinations of blood pressure ≥140/90 mmHg or specific treatment with previous diagnosis; blood pressure control was defined as <140/90 mmHg. Dyslipidemia was recorded if the patient had a history of the diagnosis or total cholesterol >220 mg/dl or low-density lipoproteins (LDL) >160mg/dl or specific drug treatment. A diagnosis of diabetes was considered in the case of previous diagnosis in the patient's medical records, specific drug treatment or two consecutive blood glucose determinations >126 mg/dl. Obesity was defined as body mass index >30 kg/m2. Abdominal obesity was included as a variable if waist circumference was >102 cm in men or >88 cm in women. Glomerular filtration rate was assessed by means of the Modification of Diet in Renal Disease equation: (186×creatinine−1.154×age−0.203) (×0.742 in women).10
Statistical analysisThe data were analyzed using SPSS version 15.0 (SPSS Inc., Chicago, IL). All variables maintained normal distribution, and are presented as mean (standard deviation). Proportions were compared using the Student's t and chi-square tests in order to identify statistical differences between the medical treatments in the two samples. The use of oral anticoagulation (OAC) in the CARDIOTENS 1999 and CARDIOTENS 2009 studies was compared by means of the Student's t test and by calculating variance of estimated percentages for each entry. The level of statistical significance was set at p<0.05.
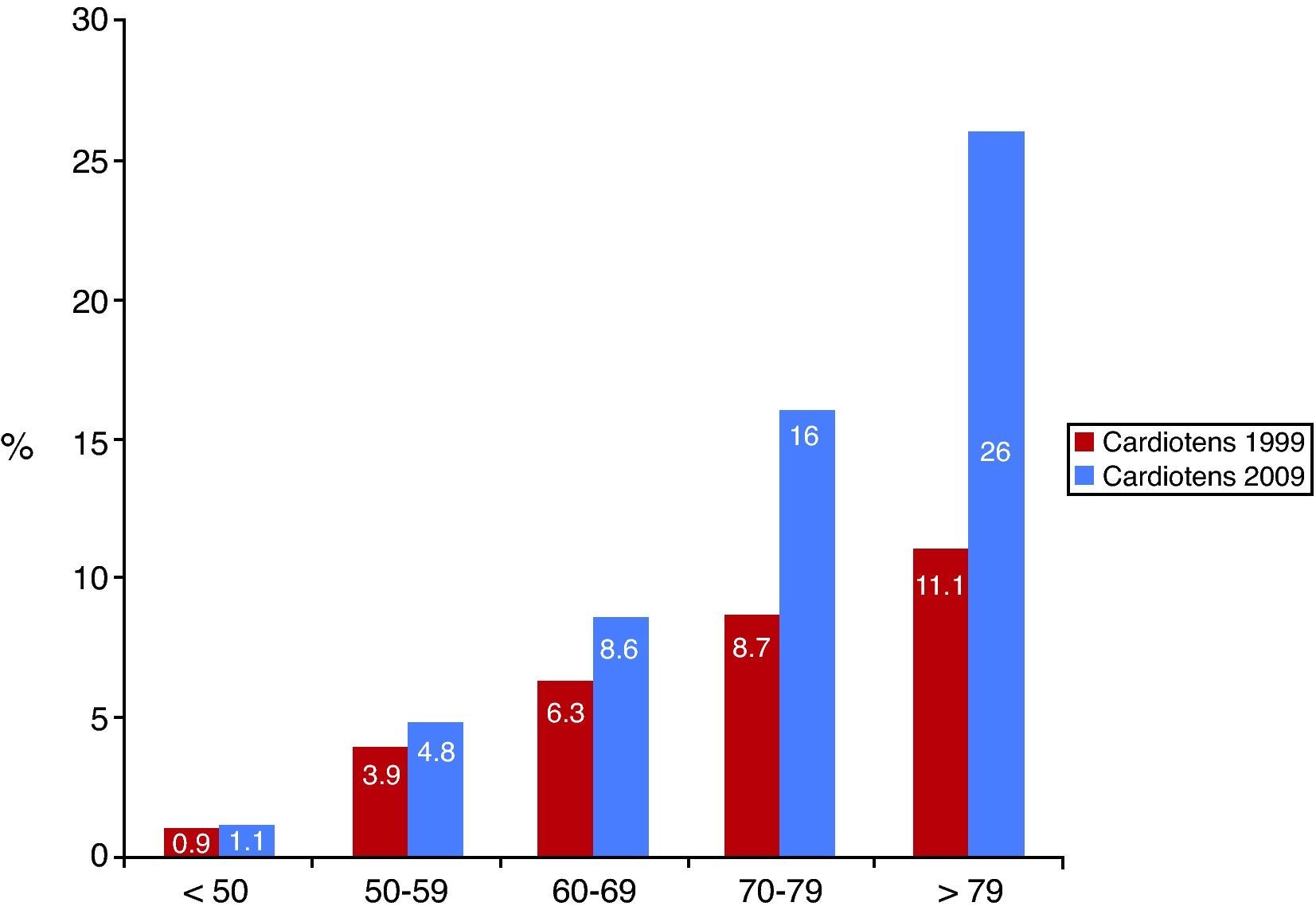
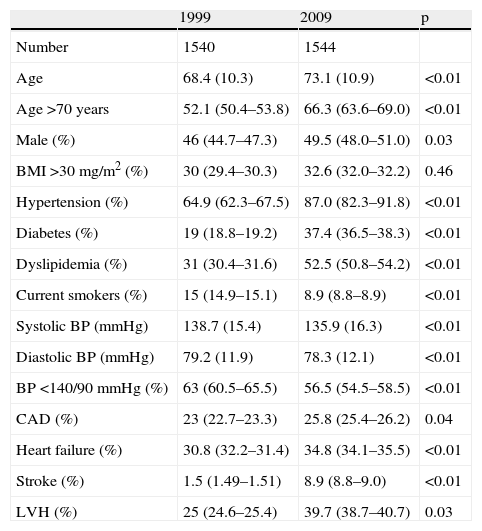
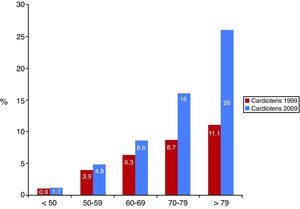
ResultsThe prevalence of AF increased by 27.9% between the two registries: from 4.8% (1540/32051) to 6.14% (1544/25137) (p<0.01). This increase was mainly in those aged over 70 (Figure 1). In both registries the proportion of women was higher in patients with AF. It is noteworthy that the prevalence of hypertension, diabetes, heart failure (HF), coronary artery disease (CAD), dyslipidemia, left ventricular hypertrophy (LVH) and previous stroke in AF patients also increased significantly between 1999 and 2009 (Table 1). Of the 10743 patients with hypertension, 55.4% (95% CI: 55.1–55.7%) had controlled blood pressure in the 2009 registry, compared with 40% (95% CI: 39.9–40.1%) in the 1999 CARDIOTENS study, a relative increase of 38.5% (p<0.01) in the rate of blood pressure control. On the other hand, the prevalence of current smokers was significantly lower in the later study (15.0%, 95% CI: 14.9–15.1 vs. 8.9%, 95%: CI: 8.8–8.9, p=0.01).
Comparative characteristics of the patients included in the two studies.
| 1999 | 2009 | p | |
| Number | 1540 | 1544 | |
| Age | 68.4 (10.3) | 73.1 (10.9) | <0.01 |
| Age >70 years | 52.1 (50.4–53.8) | 66.3 (63.6–69.0) | <0.01 |
| Male (%) | 46 (44.7–47.3) | 49.5 (48.0–51.0) | 0.03 |
| BMI >30 mg/m2 (%) | 30 (29.4–30.3) | 32.6 (32.0–32.2) | 0.46 |
| Hypertension (%) | 64.9 (62.3–67.5) | 87.0 (82.3–91.8) | <0.01 |
| Diabetes (%) | 19 (18.8–19.2) | 37.4 (36.5–38.3) | <0.01 |
| Dyslipidemia (%) | 31 (30.4–31.6) | 52.5 (50.8–54.2) | <0.01 |
| Current smokers (%) | 15 (14.9–15.1) | 8.9 (8.8–8.9) | <0.01 |
| Systolic BP (mmHg) | 138.7 (15.4) | 135.9 (16.3) | <0.01 |
| Diastolic BP (mmHg) | 79.2 (11.9) | 78.3 (12.1) | <0.01 |
| BP <140/90 mmHg (%) | 63 (60.5–65.5) | 56.5 (54.5–58.5) | <0.01 |
| CAD (%) | 23 (22.7–23.3) | 25.8 (25.4–26.2) | 0.04 |
| Heart failure (%) | 30.8 (32.2–31.4) | 34.8 (34.1–35.5) | <0.01 |
| Stroke (%) | 1.5 (1.49–1.51) | 8.9 (8.8–9.0) | <0.01 |
| LVH (%) | 25 (24.6–25.4) | 39.7 (38.7–40.7) | 0.03 |
Results presented as percentages (95% CI) and mean (SD). BMI: body mass index; BP: blood pressure; CAD: coronary artery disease; LVH: left ventricular hypertrophy.
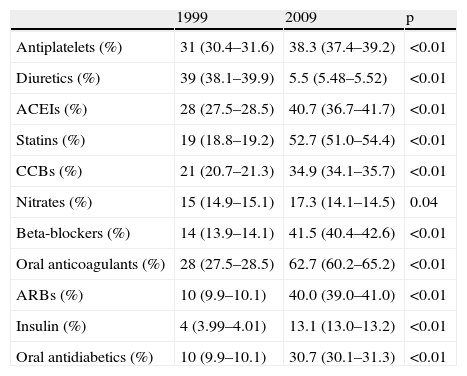
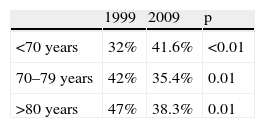
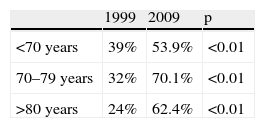
Regarding medical treatment, changes in pharmacological management were identified (Table 2). Firstly, the prescription of antiplatelets increased from 31.0% to 38.2%; however, this increase was mainly observed in patients aged under 70, and in those aged over 70 the rate of antiplatelets decreased (Table 3A). Secondly, a significant increase (p<0.01) in the number of patients being treated with OAC was also identified: 33.0% (95% CI: 32.0–34.0%) vs. 62.7% (95% CI: 59.9–65.5%), a relative increase of 90%; this rise was more evident in patients aged over 70 (Table 3B).
Medical treatments in the two studies.
| 1999 | 2009 | p | |
| Antiplatelets (%) | 31 (30.4–31.6) | 38.3 (37.4–39.2) | <0.01 |
| Diuretics (%) | 39 (38.1–39.9) | 5.5 (5.48–5.52) | <0.01 |
| ACEIs (%) | 28 (27.5–28.5) | 40.7 (36.7–41.7) | <0.01 |
| Statins (%) | 19 (18.8–19.2) | 52.7 (51.0–54.4) | <0.01 |
| CCBs (%) | 21 (20.7–21.3) | 34.9 (34.1–35.7) | <0.01 |
| Nitrates (%) | 15 (14.9–15.1) | 17.3 (14.1–14.5) | 0.04 |
| Beta-blockers (%) | 14 (13.9–14.1) | 41.5 (40.4–42.6) | <0.01 |
| Oral anticoagulants (%) | 28 (27.5–28.5) | 62.7 (60.2–65.2) | <0.01 |
| ARBs (%) | 10 (9.9–10.1) | 40.0 (39.0–41.0) | <0.01 |
| Insulin (%) | 4 (3.99–4.01) | 13.1 (13.0–13.2) | <0.01 |
| Oral antidiabetics (%) | 10 (9.9–10.1) | 30.7 (30.1–31.3) | <0.01 |
Results presented as percentages (95% CI) and mean (SD). ACEIs: angiotensin-converting enzyme inhibitors; ARBs: angiotensin receptor blockers; CCBs: calcium cannel blockers.
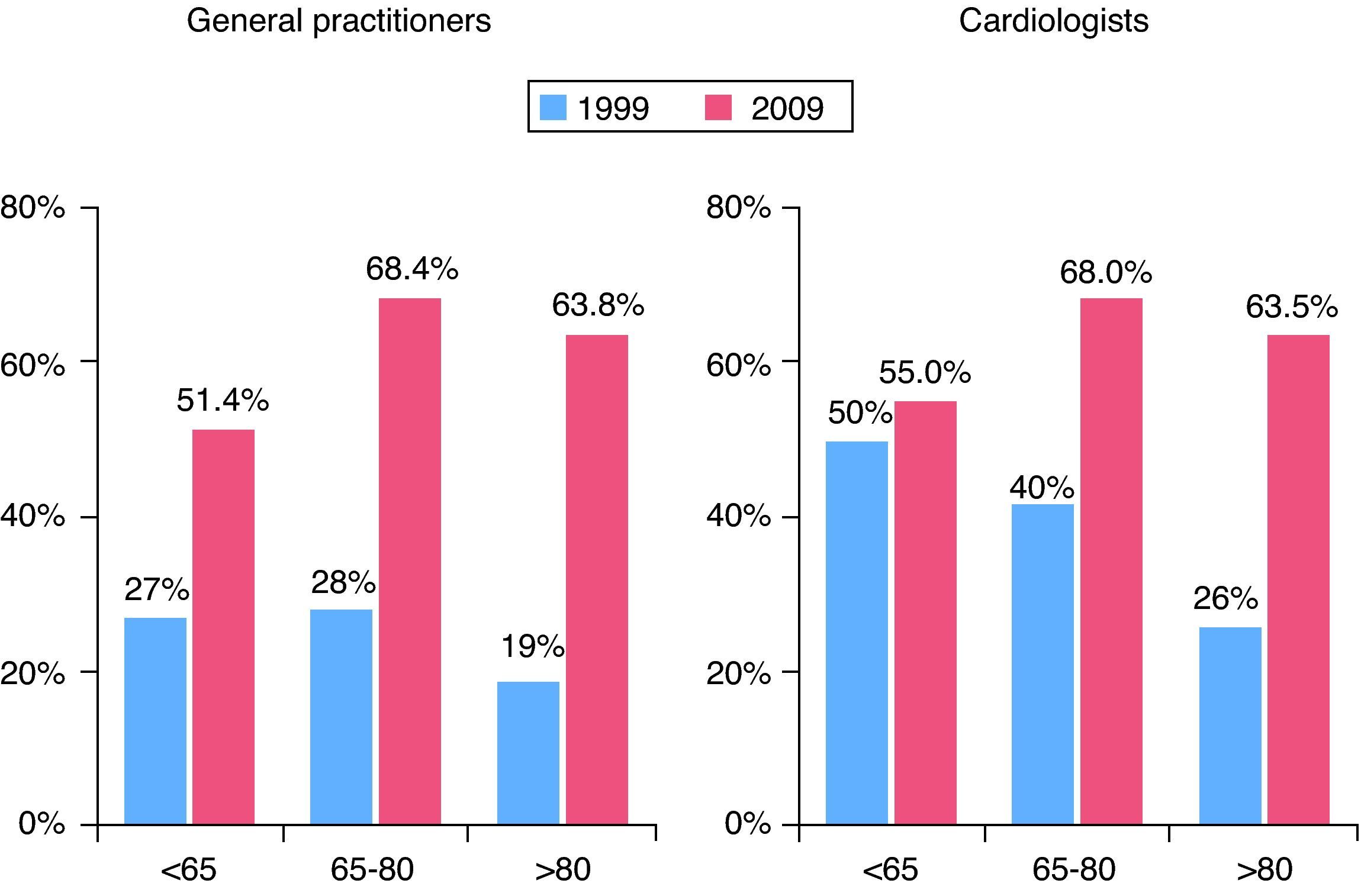
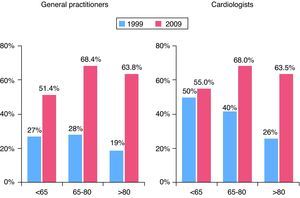
We also analyzed trends in the use of oral anticoagulants according to age and medical specialty. As shown in Figure 2, in the 1999 registry a decrease in oral anticoagulation was observed with increasing age; nevertheless, the reverse tendency was seen in 2009, with a trend for increased prescription of oral anticoagulation in older patients. The use of oral anticoagulation was greater in all age-groups in 2009 compared to 1999 (p=0.01). Furthermore, whereas in 1999 there were significant differences in the rate of oral anticoagulation depending on whether they were seen by primary care physicians or cardiologists, this difference disappeared in 2009.
The use of other treatments in patients with AF rose significantly between the two periods surveyed: prescription of angiotensin-converting enzyme inhibitors (ACEIs), angiotensin-receptor blockers (ARBs), calcium channel blockers (CCBs), nitrates and beta-blockers was higher in the 2009 study.
DiscussionOver the course of the study period, an increase in the prevalence of AF was observed, mainly due to a higher prevalence of AF in patients aged over 70, as well as more aggressive antithrombotic treatment and radical changes in the use of oral anticoagulants, reversing the decrease in their use in elderly patients seen in the first registry. Comparison of the two registries thus revealed significant shifts in the perception and treatment of patients with AF.
One possible explanation for the increase in AF prevalence is that it results from ascertainment bias related to the increased use of electrocardiography in the community. However, this was addressed and found to be an unlikely cause in the Rochester population,11 since over a 30-year period, the use of electrocardiograms increased only from 9% to 12%, as opposed to the two- to threefold increase in the prevalence of AF. Another hypothesis is that today's elderly are a sicker population: advances in preventive medicine and increasing socioeconomic prosperity have resulted in a population of elderly survivors with a higher prevalence of comorbidities including hypertension, diabetes, HF, CAD and prior cardiac surgery, in comparison with their counterparts who lived to a similar age 50 years ago.12,13 Nonetheless, when these risk factors are put into context with the size of the increase in AF prevalence, the relatively small increase in the prevalence of known comorbidities does not appear to offer more than a partial explanation.14 Therefore, these epidemiological studies need to be complemented with further analysis aimed at defining the molecular genetics of AF, in order to provide more insights into the structural and electrical phenotypes resulting from genetic mutations and their interactions with the environment. Otherwise, there is a danger that the burden of this disease could reach epidemic proportions in coming years.3
On the other hand, physicians should be aware that they are facing more complex patients, since the elderly have not only the highest risk of stroke among patients with AF, but also the highest risk of bleeding. Moreover, the present AF population exhibits a higher risk for thromboembolic events, due to the higher prevalence of hypertension, diabetes, previous stroke and HF. These epidemiological features indicate a need for new therapeutic strategies, including new oral anticoagulant agents (oral direct thrombin inhibitors such as dabigatran etexilate and AZD0837, and oral factor Xa inhibitors such as rivaroxaban, apixaban, edoxaban, betrixaban and YM150). These agents, with a safer drug profile, may provide a useful alternative to current vitamin K antagonists. Another factor increasing the need for safer agents is the wider indications for oral anticoagulation therapies in the current clinical guidelines for patients with AF.15,16 A recent analysis of the 2009 CARDIOTENS study reported that the current guidelines have increased candidates for OAC by 25%.6 This could be the reason for the significant increase in the rate of OAC prescription compared to 1999, especially in patients aged over 70. This increase could explain the decrease in the use of antiplatelets seen in patients aged over 70. Studies published in the last decade have shown that both aspirin monotherapy and dual antiplatelet therapy with clopidogrel are less effective than OAC and furthermore are associated with higher rates of bleeding.17,18 It is therefore encouraging that the awareness of physicians (both general practitioners and cardiologists) of the appropriate use of antithrombotic drug therapy in AF and of the results of recent clinical trials has improved over the last decade, to the extent that there are now no differences in the rate of OAC prescription according to the attending physician, as was the case in previous studies.19,20
It is noteworthy that the prevalence of hypertension in patients with AF also increased in the last decade. On the other hand, there has been progress in the rate of hypertension control (relative increase of 38.5%). This is important because of the emphasis on upstream therapies to slow or halt the progression of AF due to underlying cardiovascular disease and to AF itself. Such agents include ACEIs, ARBs, statins, n-3 (omega-3) polyunsaturated fatty acids, and possibly corticosteroids.15 As seen in this study, the recommendations reflect the evolution of medical therapeutics in the last 10 years, with a significant increase in the prescription rate of beta-blockers, ACEIs/ARBs and statins. Significant changes were also observed in the choice of ventricular rate control agents throughout the study period. In the 1990s, digoxin was the preferred agent for controlling ventricular rate, but during the study period the use of beta-blockers and CCBs increased significantly, due in part to the growing recognition that digoxin is particularly ineffective at controlling ventricular rate with effort.21 This is also likely to be related to the publication during this period of studies demonstrating the effectiveness of beta-blockers in patients with HF.22 To summarize, this comparative analysis of these two large observational, cross-sectional cohort studies has revealed long-term trends in the prevalence and clinical and pharmacological management of patients with AF. Mean age, prevalence of risk factors, and prevalence of AF were similar to those in previous national and international studies, reflecting standard clinical activity.23–27
Some limitations must be acknowledged, including those inherent to observational studies, which provide insufficient evidence to establish causal relationships. The fact that most patients were included by primary care physicians may mean that they are not representative of other areas of medicine. Another important limitation is that the investigators were not selected randomly from all physicians nationwide, but by randomly inviting those registered in community listings. Physicians participating in the study may therefore have been more motivated and more aware of the importance of these studies.
ConclusionsAF prevalence has increased over the last decade. This increase is due to the higher prevalence of AF in people over 70 years old. Moreover, the current AF population exhibits a higher risk profile for thromboembolic events because of the higher prevalence of hypertension, diabetes, CAD, LVH, previous stroke and HF. Regarding medical treatment, firstly more aggressive antithrombotic treatment has been observed, as well as radical changes in the use of oral anticoagulants, reversing the decreasing use in elderly patients observed in 1999. Furthermore, there are no longer differences in the rate of OAC prescription according to the attending physician (general practitioner or cardiologist). Secondly, there has also been considerable emphasis on upstream therapies in the general population with AF.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThe study presented here was funded by an unrestricted educational grant from Recordati Spain S.A. and was endorsed by the Hypertension Section and the Research Agency of the Spanish Society of Cardiology. Dr. Rodríguez-Mañero received a post-residency grant for international research from the European Heart Rhythm Association (EHRA Training Fellowship Program).
Conflicts of interestThe authors have no conflicts of interest to declare.
This work would not have not been possible without the invaluable contributions of the physicians who took part in the study presented here. The large number of participants does not permit the individual acknowledgments that we would like to give and that they well deserve.