The study examined the effects of treadmill walking with load carriage on derived measures of central pressure and augmentation index in young healthy subjects.
MethodologyFourteen male subjects (age 31.0 ± 1.0 years) volunteered in this study. Subjects walked 10 minutes on a treadmill at a speed of 5 km/h carrying no load during one session and a load of 10% of their body weight on both upper limbs in two water carboys with handle during the other session. Pulse wave analysis was performed at rest and immediately after exercise in the radial artery of the right upper limb by applanation tonometry.
ResultsThe main result indicates that walking with load carriage sharply increased augmentation index at 75 bpm (−5.5 ± 2.2 to −1.4 ± 2.2% vs. −5.2 ± 2.8 to −5.5 ± 2.1%, p<0.05), and also induced twice as high increments in central pulse pressure (7.4 ± 1.5 vs. 3.1 ± 1.4 mmHg, p<0.05) and peripheral (20.5 ± 2.7 vs. 10.3 ± 2.5 mmHg, p<0.05) and central systolic pressure (14.7 ± 2.1 vs. 7.4 ± 2.0 mmHg, p<0.05).
ConclusionsWalking with additional load of 10% of their body weight (aerobic exercise accompanied by upper limb isometric contraction) increases derived measures of central pressure and augmentation index, an index of wave reflection and arterial stiffness.
O presente estudo avaliou os efeitos de caminhar na passadeira rolante transportando uma carga adicional nos membros superiores em parâmetros derivados de pressão central e índice de aumentação de jovens aparentemente saudáveis.
Metodologia14 sujeitos do sexo masculino (idade de 31,0 ± 1,0 anos) participaram no estudo. Os sujeitos caminharam 10 minutos na passadeira rolante a uma velocidade de 5 km/h, sendo que numa sessão não transportaram carga adicional e noutra sessão transportando 10% do seu peso corporal nos membros superiores em dois garrafões de água. A análise da onda de pulso foi efetuada em repouso e imediatamente após o exercício na artéria radial do membro superior direito por tonometria de aplanação.
ResultadosOs principais resultados indicam que caminhar transportando peso nos membros superiores aumenta marcadamente o índice de aumentação a 75 batimentos por minuto (−5,5 ± 2,2 para −1,4 ± 2, 2% versus −5,2 ± 2,8 para −5.5 ± 2,1%, p<0,05), a pressão de pulso central (7,4 ± 1,5 versus 3,1 ± 1,4 mmHg, p<0,05), a pressão de pulso periférica (20,5 ± 2,7 versus 10,3 ± 2,5 mmHg, p<0,05) e a pressão sistólica central (14,7 ± 2,1 versus 7,4 ± 2,0 mmHg, p<0,05).
ConclusõesCaminhar transportando uma carga adicional de 10% do peso corporal nos membros superiores (exercício aeróbio acompanhado de contração isométrica dos músculos dos membros superiores) aumenta medidas derivadas da pressão central e o índice de aumentação, um índice de reflexão da onda e rigidez arterial.
In the last decade, arterial stiffness has emerged as an important predictor of cardiovascular and all-cause mortality in the context of cardiovascular diseases.1–3 Increased arterial stiffness induces several harmful hemodynamic consequences including increases in systolic blood pressure (SBP) and pulse pressure (PP),4 which are related to systolic and diastolic cardiac dysfunction at a central level,5 augmented cardiac load, and reduced coronary perfusion.6 In fact, arterial stiffness is an important factor in the balance between the myocardial blood supply and the demand, with implications to myocardial work capacity impacting on exercise capacity and cardiovascular risk.7
The “gold standard” non-invasive measure of aortic wall stiffness is the carotid-femoral pulse wave velocity (cf-PWV), also called aortic pulse wave velocity (PWV).8 Aortic PWV has been suggested as a strong and independent predictor of cardiovascular and all-cause mortality in subjects with coronary artery disease, renal disease, hypertension, or diabetes.3,8 Another measure related to arterial stiffness can be derived from the analysis of pulse wave in peripheral arteries, such as the radial artery, using applanation tonometry.3,9 This noninvasive method provides an index of pulse-wave reflection and arterial stiffness, called augmentation index (AIx), which reflects the degree of aortic pressure augmentation relative to central pulse pressure.3,9 AIx denotes the difference in amplitude between incident and reflected pulse waves expressed as a percentage of pulse pressure.9 Likewise aortic PWV, AIx has been shown to be an independent predictor of cardiovascular events and mortality in cardiovascular patients.2,10–12
Exercise training alone or incorporated in a cardiac rehabilitation program promotes positive effects on several aspects, including endothelial dysfunction, vascular wall inflammation, and arterial stiffness related indexes (e.g. aortic PWV and AIx).13–16 In contrast to chronic exercise, an acute bout of exercise increases transiently AIx both in healthy subjects.17,18 Also in cardiovascular disease patients,19 a single bout of aerobic exercise of moderate intensity increased proximal arterial stiffness expressed by increases in carotid systolic blood pressure, pulse pressure (PP) and PP amplification.
If the aerobic exercise is known to acutely increase PWV, central pressures and AIx, less is know regarding isodynamic exercise. In fact, the hemodynamic parameters and energy cost in isodynamic activities has been widely described in a variety of individuals,20–24 nevertheless, to our best knowledge, few studies exist exploring the acute effects of exercise combining static and dynamic muscle actions on arterial stiffness. This is a topic of particular interest considering that numerous tasks of daily living include isodynamic exercise, such as walking with backpack carriage or with hand load carriage, which combines dynamic and isometric muscle actions. External load carriage has applications in physical training, recreational activities, and the prevention and rehabilitation of cardiovascular diseases. Nonetheless, the impact of walking while carrying a load on the upper limbs (aerobic exercise plus upper limb isometric contractions) on derived measures of central pressure and AIx is poorly understood. Due to the lack of definite data regarding this particular kind of exercise, it was decided to perform the present study in healthy young subjects. Therefore, the present study was designed to assess the impact of treadmill walking with load carriage on derived measures of central pressure and AIx in young healthy subjects.
MethodsSubjectsFourteen healthy male volunteers (age 31.0 ± 1.0 years, weight 81.2 ± 3.1 kg, height 174.5 ± 1.2 cm, body mass index 26.6 ± 0.9 kg/m2) participated in this study. Participants were excluded according to the following criteria: athletes, smokers, on any medication, and previous history of hypertension, renal dysfunction or any known cardiovascular or metabolic disease as assessed by medical history. The local ethics committee approved the present study. All participants provided written informed consent and all procedures were conducted according to the Declaration of Helsinki.
ProceduresSubjects reported to the laboratory on two occasions: they were asked to walk for ten minutes on a treadmill (H/P/Cosmos Quasar 4.0 – Nussdorf, Germany) at a speed of 5 km/h carrying no load during one session and carrying a load of 10% of their body mass during the other. The load was carried on both upper limbs in two water carboys with handle. Both sessions were separated by one week, and the order of the protocols was randomly assigned.
The walking speed of 5 km/h was chosen because it is a comfortably walking speed for the majority humans. The duration of the walk and the weight of extra load was set to reproduce a real life situation such as the transport of groceries from supermarket to home.
Assessment procedures for pulse wave analysis were standardized according to the recommendations.8 In brief, all subjects were evaluated at the same time of day in a quiet room and the temperature in the two sessions was maintained at 22°C. Before sessions, subjects rested seated in a quiet environment for fifteen minutes. Subjects were told to avoid intense or exhaustive exercise 48 h prior to the beginning and during the study period. No meal or caffeine was allowed within three hours before measurements. Speaking and sleeping were not allowed during measurements. The same well-trained investigator performed all procedures.
MeasurementsHeight and weight were measured using a stadiometer and a scale, respectively. Body mass index was calculated as weight (kg) divided by height (m) squared. Peripheral SBP and diastolic blood pressure (DBP) were measured using an automatic device (Pressmate BP-10, Colin, Mediana Technologies Corporation, San Antonio, TX, USA). Patients sat down resting their right arm on a table so the brachial artery was level with the heart. Two measurements were then obtained and their average was recorded. If there was more than 5 mmHg of difference between the two readings, one more reading was obtained for average. Peripheral blood pressures were recorded before and immediately after each session. Peripheral mean BP was determined as DBP+[(SBP−DBP)/3].
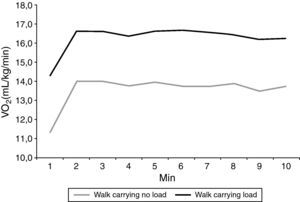
Heart rate (HR) was continuously measured during exercise via a telemetric system (Polar Electro Oy, Kempele, Finland). Oxygen uptake (VO2) was measured during exercise using a breath-by-breath metabolic system (Cosmed K4b2, Cosmed, Rome, Italy). The HR and metabolic variables were averaged at each 60-second interval and VO2 and HR at steady-state was determined for each test by manually extracting the metabolic steady-state data.25,26 The VO2 and HR values for each subject were obtained by averaging a minimum of three minutes of data.26
Pulse wave analysis was performed at baseline (after a period of 15-min rest) and immediately after each exercise session using the SphygmoCor (model SCOR-Px; Atcor Medical, Sydney, Australia) as previously described.9,17,18 In brief, subjects were seated with the forearm in supine position. The pulse on the right radial artery was initially found using the index finger. Then, the SphygmoCor probe was applied firmly onto the right radial artery applying gentle pressure to flatten but not occlude the radial artery. Once a strong and reproducible waveform was obtained, the probe was kept in this position, and subsequent waveforms were acquired for at least 10 seconds and saved for analysis. The SphygmoCor software generated an averaged central (aortic) waveform, which was used for the determination of aortic AIx. AIx is an indicator of wave reflection, expressing the degree of aortic pressure augmentation relative to central PP. The software also calculated central SBP, augmentation pressure, mean BP, aortic PP, and augmentation pressure. Since the AIx is affected by changes in heart rate, AIx at a HR of 75 beats per min (AIx@75) was also calculated. In order to obtain high-quality waveforms and to enhance the accuracy of measurements, only values whose operator index exceeded 90% were used.
Data analysisStatistical analysis was performed using SPSS version 17.0 (SPSS Inc., Chicago, IL). The normality of data distribution was tested with the Shapiro–Wilk test. Data were normally distributed and presented as means ± SE. The paired Student t-test was used to test for differences between exercise sessions in the VO2 and HR during exercise. A repeated-measures analysis of variance (exercise session X time) was used to analyze AIx@75 bpm, central and peripheral BP, augmentation pressure, aortic PP, and augmentation pressure values. When a significant interaction was observed, within-group comparisons between time points and between-group comparisons at each time point were performed using Bonferroni post hoc analysis. Effect size was measured using partial eta-squared. p<0.05 was considered indicative of statistical significance.
ResultsAt rest (e.g. before exercise sessions), there were no significant differences in any of the variables assessed (Table 1). Steady-state VO2 (16.5 ± 0.4 Vs.13.8 ± 0.4 mL/kg/min, p<0.05) and HR (115.0 ± 3.3 Vs. 99.1 ± 3.2 beats/min, p<0.05) were significantly higher during the exercise session carrying a load of 10% of subjects’ body weight in comparison to the session without carrying load. The evolution of VO2 during each session is provided in Figure 1.
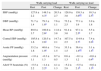
Comparison of peripheral and derived central hemodynamic parameters assessed after the exercise sessions.
| Walk carrying load | Walk carrying no load | |||||
| Rest | Post | Change | Rest | Post | Change | |
| SBP (mmHg) | 127.8 ± 2.2 | 148.3 ± 4.3a | 20.5 ± 2.7 | 128.0 ± 3.0 | 138.3 ± 3.6a,b | 10.3 ± 2.5b |
| DBP (mmHg) | 71.7 ± 1.4 | 79.3 ± 1.8a | 7.6 ± 1.1 | 73.2 ± 2.5 | 77.1 ± 1.9 | 3.9 ± 1.8 |
| Mean BP (mmHg) | 89.0 ± 3.7 | 100.8 ± 2.6a | 11.8 ± 3.8 | 91.4 ± 3.0 | 97.1 ± 2.5a | 5.5 ± 1.7 |
| Central SBP (mmHg) | 105.8 ± 1.6 | 120.5 ± 2.8a | 14.7 ± 2.1 | 107.5 ± 2.5 | 114.9 ± 2.7a | 7.4 ± 2.0b |
| Aortic PP (mmHg) | 33.2 ± 1.6 | 40.6 ± 1.9a | 7.4 ± 1.5 | 33.3 ± 1.5 | 36.4 ± 1.4a,b | 3.1 ± 1.4b |
| Augmentation pressure (mmHg) | −1.0 ± 1.1 | −0.3 ± 1.3 | 0.7 ± 0.5 | 0.6 ± 1.3 | −0.1 ± 1.2 | −0.6 ± 0.4b |
| AIx@75 beats/min (%) | −5.5 ± 2.2 | −1.4 ± 2.2a | 4.1 ± 1.3 | −5.2 ± 2.8 | −5.5 ± 2.1b | −0.6 ± 1.3b |
AIx: augmentation index; DBP: diastolic blood pressure; PP: pulse pressure; SBP: systolic blood pressure.
Both protocols increased peripheral SBP, peripheral mean BP, central SBP and aortic PP. Although, the repeated-measures ANOVA revealed a main effect of the exercise session on peripheral SBP [F(1,13)=10.210, p=0.007, η2p=0.440], central SBP [F(1,13)=7.626, p=0.016, η2p=0.370], and aortic PP [F(1,13)=7.150, p=0.019, η2p=0.355], indicating that the change induced by the exercise session was higher when walking carrying extra load (Table 1). A main effect of the exercise session was also observed in the augmentation pressure [F(1,13)=6.811, p=0.022, η2p=0.344]. Regarding AIx@75 bpm (Table 1), it was significantly elevated in comparison to baseline values only following the session carrying a load of 10% of the subjects’ body weight [F(1,13)=6.007, p=0.029, η2p=0.316].
DiscussionThe main finding of the present study was that a daily living task, such as walking while carrying a load on the upper limbs, induces an acute increase on derived measures of central pressure and AIx, an index of wave reflection and arterial stiffness, assessed by applanation tonometry. As expected, the session encompassing external load carriage produced a more intense physiologic stimulus compared to the walking without carriage session, expressed by the differences in VO2 and HR during sessions.
These results suggest that the isometric component of the upper limbs augments the arterial stiffness, since only the protocol encompassing load carriage significantly increased AIx@75 beats/min. These results are comparable with previous studies reporting increased AIx after isometric exercises.17,18 This increase seems to be related to the elevated sympathetic vasoconstrictor tone and circulatory arrest during isometric exercise.18 Nevertheless, mean arterial pressure was similar after both sessions, indicating that changes in blood pressure, which is a critical variable in the evaluation of arterial stiffness and related measures per se cannot fully explain the differences observed in AIx@75 beats/min. Lydakis et al.18 investigated the acute effects of isometric fatiguing handgrip on indices of central arterial stiffness. Subjects performed isometric handgrip at 40% of maximal voluntary contraction until they were unable to maintain that tension. The authors observed a significant increase in central SBP, central DBP, central PP, and AIx at the end of the isometric exercise. It has also been reported that an acute bout of resistance exercise, performed at 60% of the one repetition maximum, increased carotid-femoral pulse wave velocity and AIx@75 beats/min in young healthy men.27 The increase observed in AIx@75 beats/min in the present study is less pronounce comparetive to that observed by Yoon27 also in young healthy men. Collier et al.28 compared the acute effects of resistance exercise and aerobic exercise on arterial stiffness. They assessed PWV pre exercise, 40 and 60 minutes post exercise and found an increase in pulse wave velocity only after resistance exercise.
The present study has some limitations. It was not measured carotid-femoral pulse wave velocity, also called aortic PWV, which is considered the “gold standard” non-invasive measure of aortic wall stiffness.8 It was used pulse wave analysis and the generalized transfer function to generate central waveforms to assess the effects of isodynamic exercise on arterial stiffness in order to reduce the time elapsing between the end of the exercise and the assessment, as it is less time consuming. Nevertheless, Alx has been shown to be also an independent predictive value for cardiovascular events and mortality.2 Additionally, clinical significance of the present findings is yet to be determined, since this study was conducted in healthy young adults. Thus, the logical consequence of the present study will be the replication of its procedures and exercise protocols in subjects with conditions elevating arterial stiffness such as hypertension. This seems relevant since an inverse correlation between time to ischemia during treadmill exercise testing and arterial stiffness in coronary artery disease patients was reported.7
ConclusionIn conclusion, this study shows that an every day activity combining dynamic and isometric exercise, such as walking while carrying a load on the upper limbs induces an acute increase on derived measures of central pressure and AIx, an index of wave reflection and arterial stiffness, assessed by applanation tonometry. It should be emphasized that this increase was observed in young healthy male subjects. Nevertheless, in the absence of definitive data regarding the impact of isodynamic exercise in patients with elevated arterial stiffness, caution should be used when prescribing isodynamic exercise for those where increasing afterload may increase the risk of a cardiovascular event.
Conflict of interestThe authors have no conflict of interest to declare.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.