Correct diagnosis in wide QRS complex tachycardia remains a challenge. Differential diagnosis between ventricular and supraventricular tachycardia has important therapeutic and prognostic implications, and although data from clinical history and physical examination may suggest a particular origin, it is the 12-lead surface electrocardiogram that usually enables this differentiation.
Since 1978, various electrocardiographic criteria have been proposed for the differential diagnosis of wide complex tachycardias, particularly the presence of atrioventricular dissociation, and the axis, duration and morphology of QRS complexes. Despite the wide variety of criteria, diagnosis is still often difficult, and errors can have serious consequences. To reduce such errors, several differential diagnosis algorithms have been proposed since 1991. However, in a small percentage of wide QRS tachycardias the diagnosis remains uncertain and in these the wisest decision is to treat them as ventricular tachycardias.
The authors’ objective was to review the main electrocardiographic criteria and differential diagnosis algorithms of wide QRS tachycardia.
O diagnóstico correto de taquicardia de complexos largos permanece um desafio. A sua diferenciação entre taquicardia supraventricular e taquicardia ventricular tem grandes implicações terapêuticas e prognósticas e, embora alguns dados na história clínica e no exame físico nos possam sugerir uma determinada origem, é o eletrocardiograma de 12 derivações que permite habitualmente essa diferenciação.
Desde 1978, diversos critérios eletrocardiográficos têm sido propostos para o diagnóstico diferencial das taquicardias de complexos largos, nomeadamente a presença de dissociação aurículo-ventricular e a duração, o eixo e a morfologia dos complexos QRS. Apesar da grande diversidade de critérios, o diagnóstico revela-se frequentemente difícil, originando erros com consequências gravosas. Para diminuir a probabilidade de erros foram introduzidos desde 1991 vários algoritmos de diagnóstico diferencial. Contudo, apesar de os vários critérios e algoritmos de diagnóstico, continua a existir uma pequena percentagem de taquicardias de QRS largos que mantêm um diagnóstico incerto e em que o mais sensato é tratar como se fossem taquicardias ventriculares.
O objetivo dos autores foi rever os principais critérios e algoritmos eletrocardiográficos de diagnóstico diferencial de uma taquicardia de QRS largos.
Wide QRS complex tachycardia is defined as a heart rate of >100bpm and QRS duration of >120ms. It may be of supraventricular or ventricular origin, and differential diagnosis between the two has important therapeutic and prognostic implications.
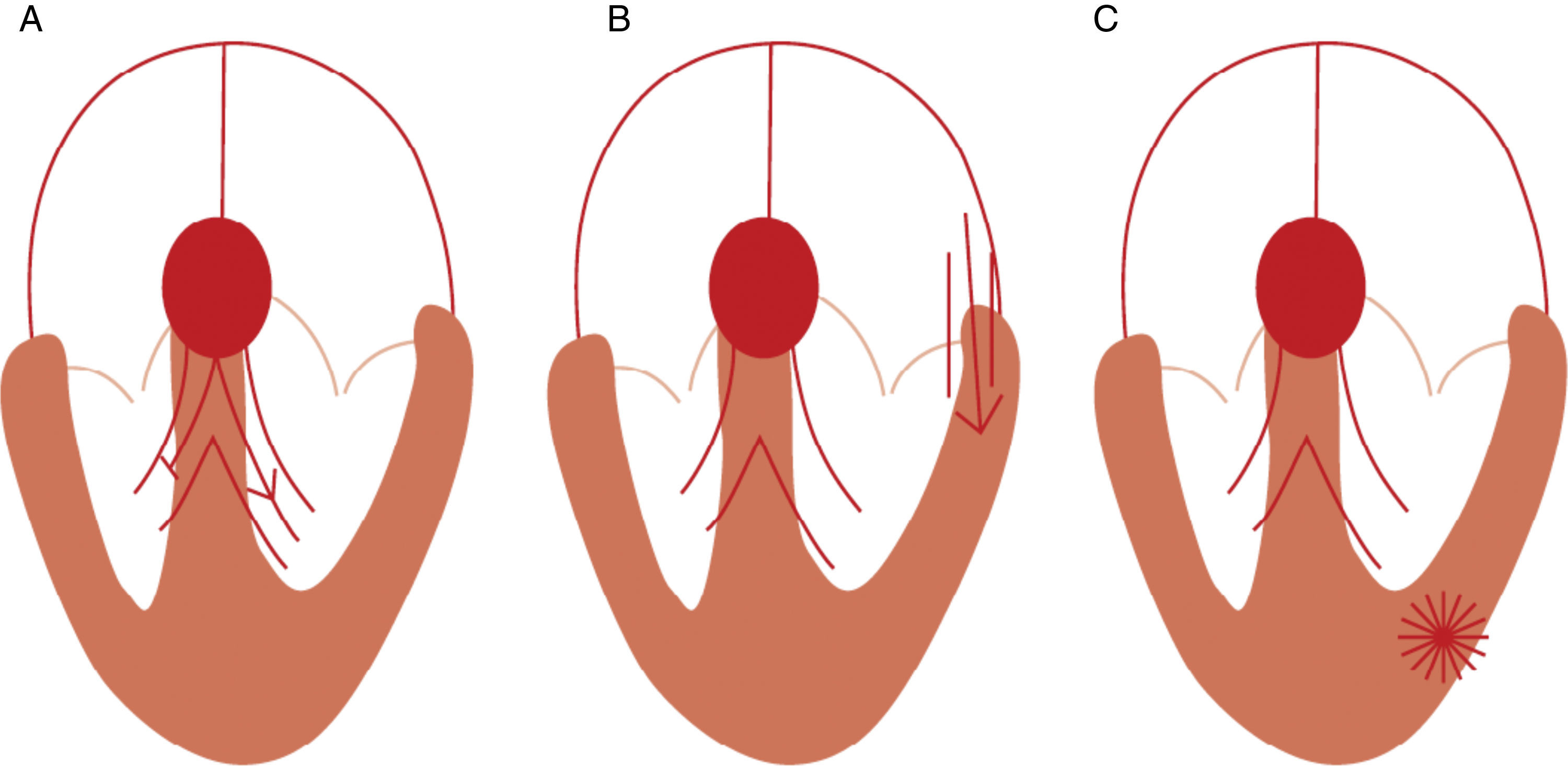
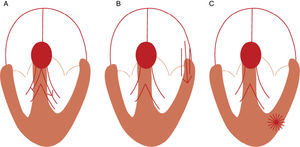
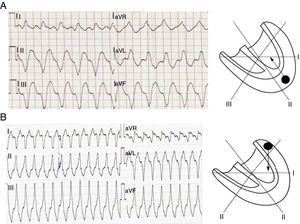
In the absence of a pacemaker rhythm, there are three possibilities to consider in wide QRS tachycardia (Figure 1):
- (A)
supraventricular tachycardia (SVT) with bundle branch block (BBB). BBB may be pre-existing or can occur when the refractory period of one of the bundle branches is reached because of the heart rate of the SVT, or due to retrograde invasion in one of the bundle branches.1 These causes of BBB can be found in patients with atrial tachycardia (AT), atrial flutter, atrial fibrillation (AF), atrioventricular (AV) nodal reentrant tachycardia or orthodromic AV reentrant tachycardia with AV conduction over the AV node and ventriculoatrial (VA) conduction over an accessory pathway;
- (B)
SVT with AV conduction via an accessory pathway. This may occur during AT, atrial flutter, AF, AV nodal reentrant tachycardia (less frequently), or antidromic AV reentrant tachycardia with AV conduction over an accessory pathway and VA conduction over the AV node or a second accessory pathway;
- (C)
ventricular tachycardia (VT).2
Mechanisms of wide QRS tachycardia. (A) Supraventricular tachycardia with bundle branch block; (B) supraventricular tachycardia with AV conduction via an accessory pathway; (C) ventricular tachycardia (adapted with permission from Wellens2).
Data from clinical history and physical examination may help identify the origin of the arrhythmia. VT is the most common cause of wide QRS tachycardia (around 80% of cases),3 and is strongly suggested by a history of heart disease (myocardial infarction [MI] or congestive heart failure), with a positive predictive value of 95%.4 A history of similar episodes in recent years suggests SVT.5
Physical findings that suggest AV dissociation, such as cannon A waves in the jugular venous pulse, variable intensity of S1, or variable arterial pressure unrelated to breathing, point towards a ventricular origin.6 On the other hand, if the tachycardia can be terminated by maneuvers such as the Valsalva maneuver, this strongly suggests a supraventricular origin (although some types of VT such as fascicular VT can also be terminated by the Valsalva maneuver). Another important aspect of physical examination is hemodynamic stability, which is crucial for treatment in the acute phase. However, it should be borne in mind that, although VT is often accompanied by hemodynamic compromise, wide QRS tachycardia in a hemodynamically stable patient is not necessarily of supraventricular origin and that ultimately it is functional cardiac reserve that determines hemodynamic status in a patient with tachycardia, whether SVT or VT.
Correct diagnosis in wide complex tachycardia remains a challenge despite the numerous criteria for differentiating between VT and SVT. However, accurate diagnosis is essential for treatment both in the acute phase and in the medium to long term.
Electrocardiographic criteria for differential diagnosis of wide QRS tachycardiaThe 12-lead surface electrocardiogram (ECG) is the most important tool for identifying the origin of tachyarrhythmias. Since 1978, various electrocardiographic criteria have been proposed for the differential diagnosis of wide complex tachycardias, most of them based on the presence of AV dissociation and the axis, duration and morphology of QRS complexes.
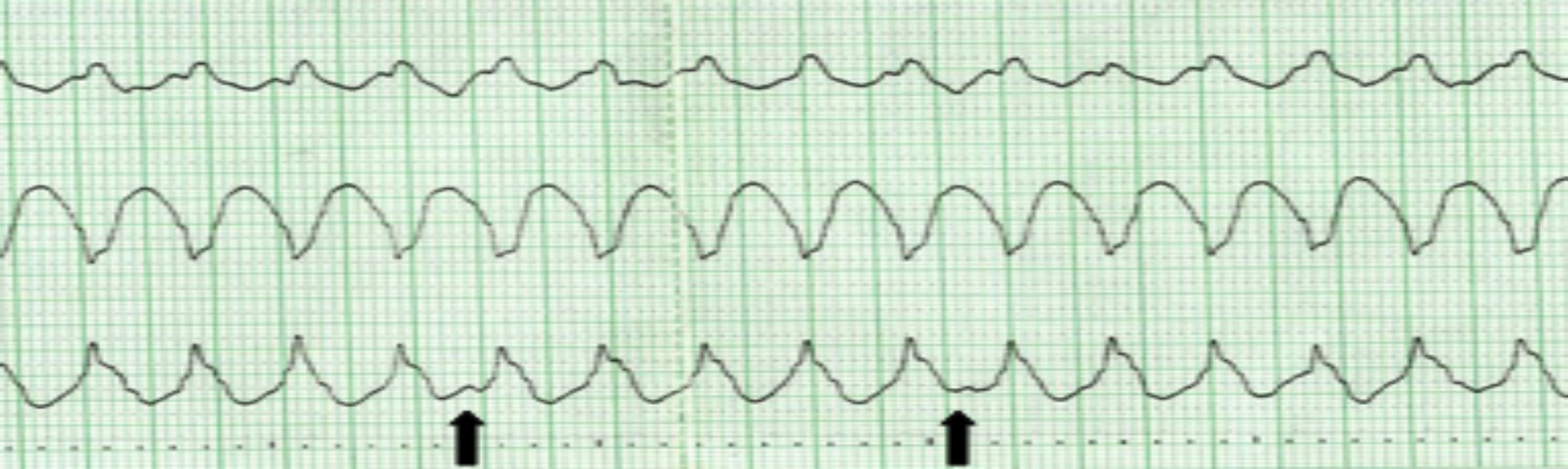
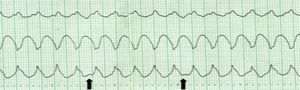
Importance of atrioventricular dissociationP waves can be difficult to distinguish in wide QRS tachycardia, but they may be detectable dissociated from the QRS complex, especially in slow VT (Figure 2). Similarly, conduction from atria to ventricles may occasionally occur, resulting in capture or fusion complexes (Figure 3). Such evidence of AV dissociation is an indication of VT.
QRS duration of more than 140ms with right bundle branch block (RBBB), or of more than 160ms with left bundle branch block (LBBB), suggests VT.1 However, since the site of origin of the tachycardia affects QRS duration, this may be shorter when the origin is in or close to the interventricular septum (IVS). On the other hand, in SVT the QRS may be longer than 140ms with RBBB and longer than 160ms with LBBB in the following situations: (1) in the presence of pre-existing BBB in the elderly with fibrosis in the bundle branch system and ventricular myocardium; (2) when AV conduction occurs over an accessory AV pathway; (3) when class IC drugs (especially flecainide) are used during SVT.2
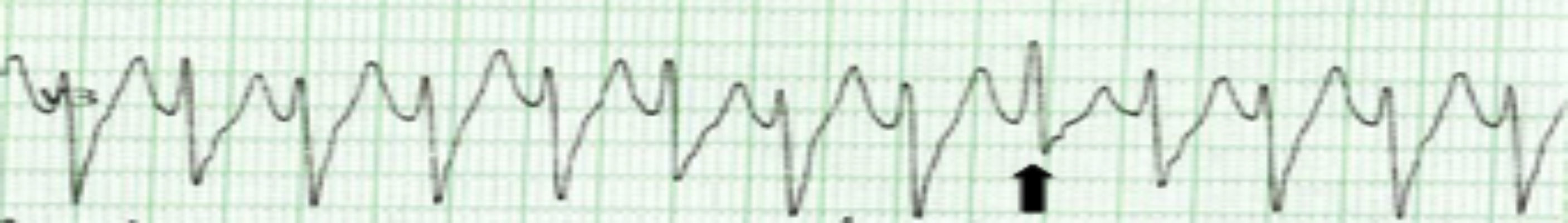
QRS axis in the frontal planeThe QRS axis provides important clues to the site of origin and etiology of tachycardia (Figure 4). When VT originates in the apical region of the ventricle, the axis of ventricular depolarization is directed superiorly and the QRS complexes in the inferior leads are negative. When VT has its origin in the basal area of the ventricle, an inferior axis is present and the QRS complexes are positive in the inferior leads. The presence of a superior axis in patients with RBBB-shaped wide QRS tachycardia suggests VT. This does not hold for an LBBB-shaped tachycardia.1 The presence of an inferior axis in LBBB-shaped wide QRS tachycardia argues for a VT arising in the outflow tract of the right ventricle.2
Determining the origin of ventricular tachycardia according to QRS axis. (A) In ventricular tachycardia with apical origin the axis of ventricular depolarization is directed superiorly, and so the QRS complexes are negative in DII, DIII and aVF; (B) a ventricular tachycardia with basal origin results in positive QRS complexes in DII, DIII and aVF (adapted with permission from Wellens2).
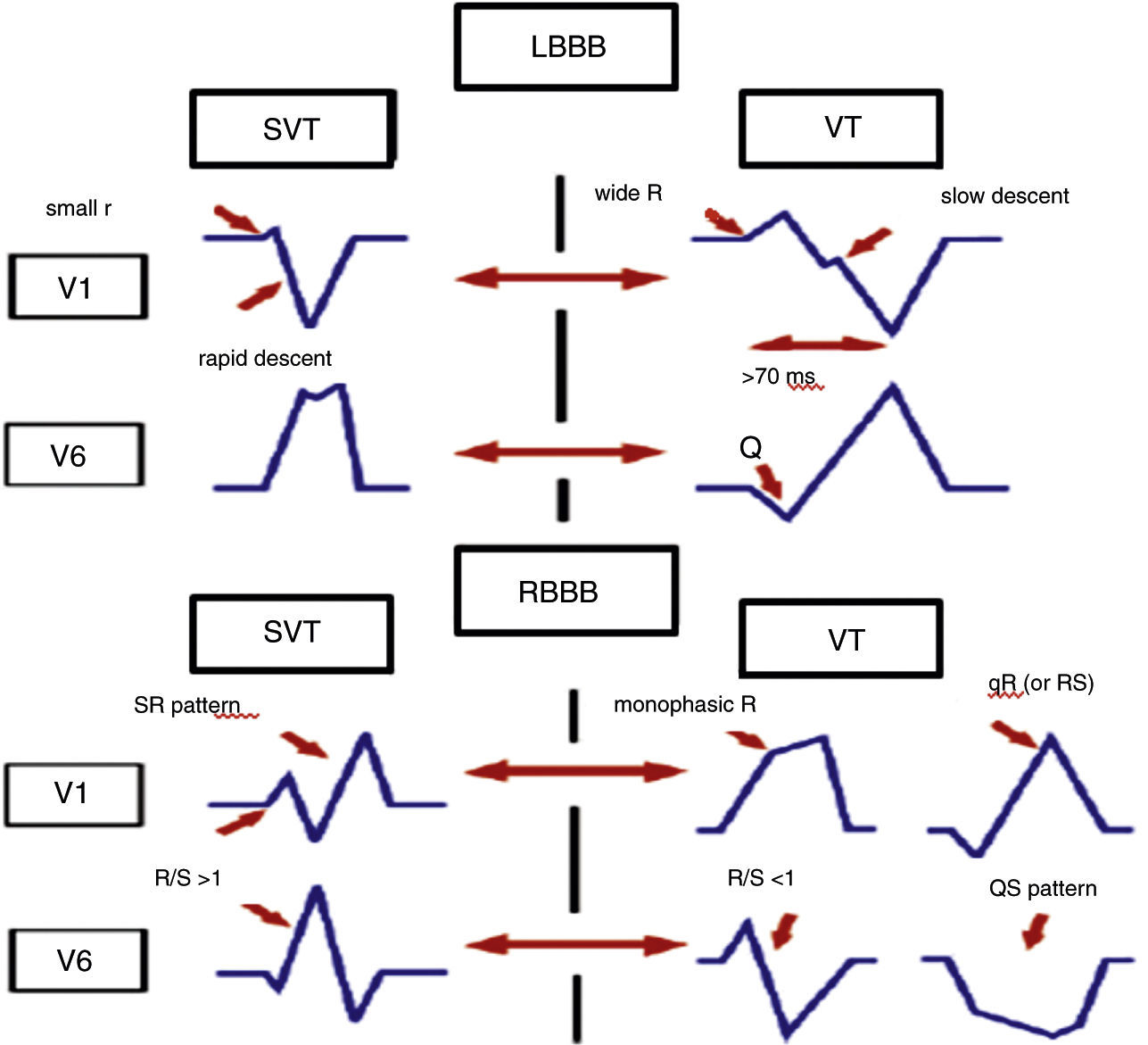
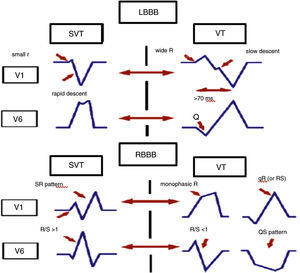
In RBBB-shaped tachycardia, the presence of a qR or R complex in lead V1 suggests a ventricular origin, while a three-phasic (RSR) pattern suggests a supraventricular origin.7 Lead V6 can also be very helpful in correctly differentiating RBBB-shaped tachycardia: when the R:S ratio is <1, a VT is very likely.1
LBBB-shaped tachycardia is suggestive of VT if lead V1 shows an initial positive QRS deflection of over 30ms, slurring or notching of the downstroke of the S wave, and an interval between the beginning of the QRS and the nadir of the S wave of 70ms or more.8 A qR pattern in lead V6 during LBBB-shaped tachycardia favors VT. In SVT with LBBB, lead V1 shows no or minimal initial positivity, a very rapid downstroke of the S wave, and a short interval between the beginning of the QRS and the nadir of the S wave (Figure 5).
Interval from onset QRS to nadir of S wave in precordial leadsAn RS interval of >100ms in one or more precordial leads is highly suggestive for VT,9 although this may also occur in SVT with AV conduction over an accessory pathway, SVT during administration of drugs that slow intraventricular conduction (particularly flecainide), and in SVT with pre-existing BBB, especially LBBB.
Concordant patternWhen all precordial leads show either negative or positive QRS complexes this is called negative or positive concordancy. Negative concordancy is diagnostic for VT arising in the apical area of the left ventricle. Positive concordancy means that in the horizontal plane ventricular activation starts left posteriorly. This can be found either in VT originating in the left posterior wall or during tachycardias using a left posterior accessory AV pathway for AV conduction.2
Presence of QR complexesA QR complex (but not QS) during wide complex tachycardia suggests an infarct scar.10 QR complexes are found in around 40% of patients with VT after MI.11
Value of the ECG during sinus rhythmThe ECG during sinus rhythm may show changes such as pre-existing BBB, ventricular pre-excitation or previous MI, which may be very helpful in correctly interpreting the ECG during wide QRS tachycardia.
The presence of AV conduction disturbances during sinus rhythm makes it very unlikely that a wide QRS tachycardia has a supraventricular origin.
Another important point is that, paradoxically, narrower QRS complexes during tachycardia than during sinus rhythm point to VT, which may be explained by its origin close to the IVS, making activation of the ventricles more closely synchronized and resulting in narrower QRS.
A wide range of criteria have been proposed for the differential diagnosis of wide QRS tachycardia, but even so errors are common and can have serious consequences12–14. Systematic analysis of the ECG following diagnostic algorithms based on predefined criteria will improve diagnostic accuracy in determining the etiology of wide complex tachycardias.
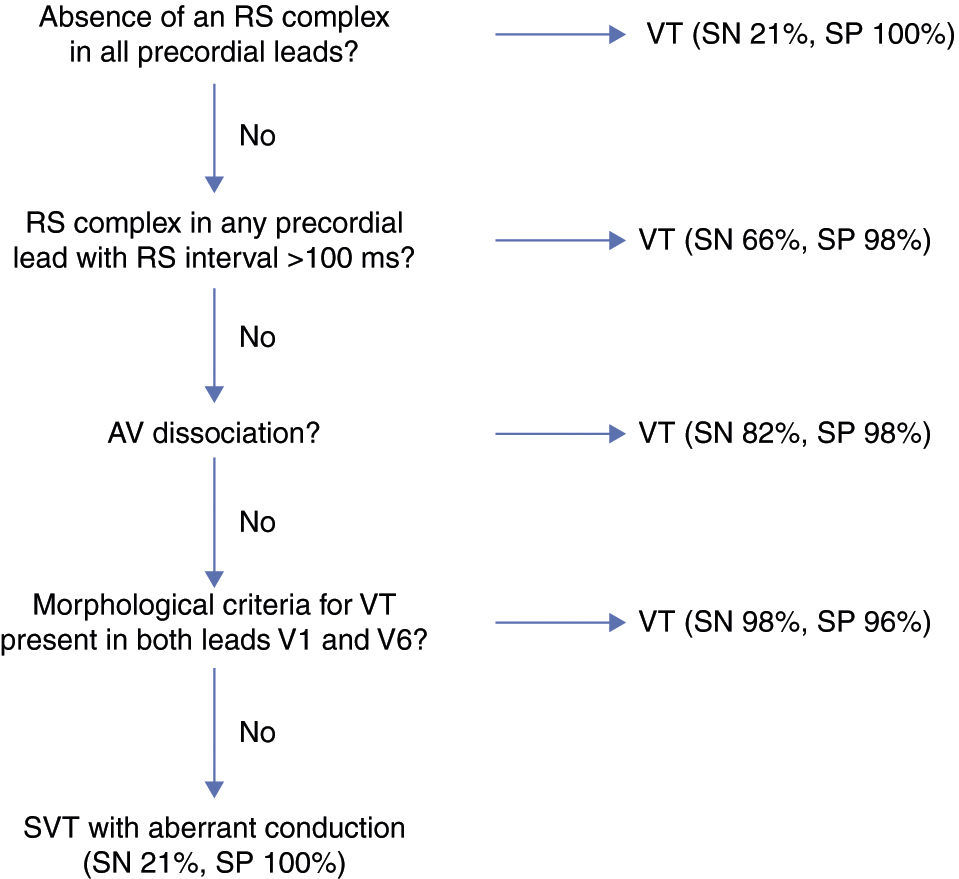
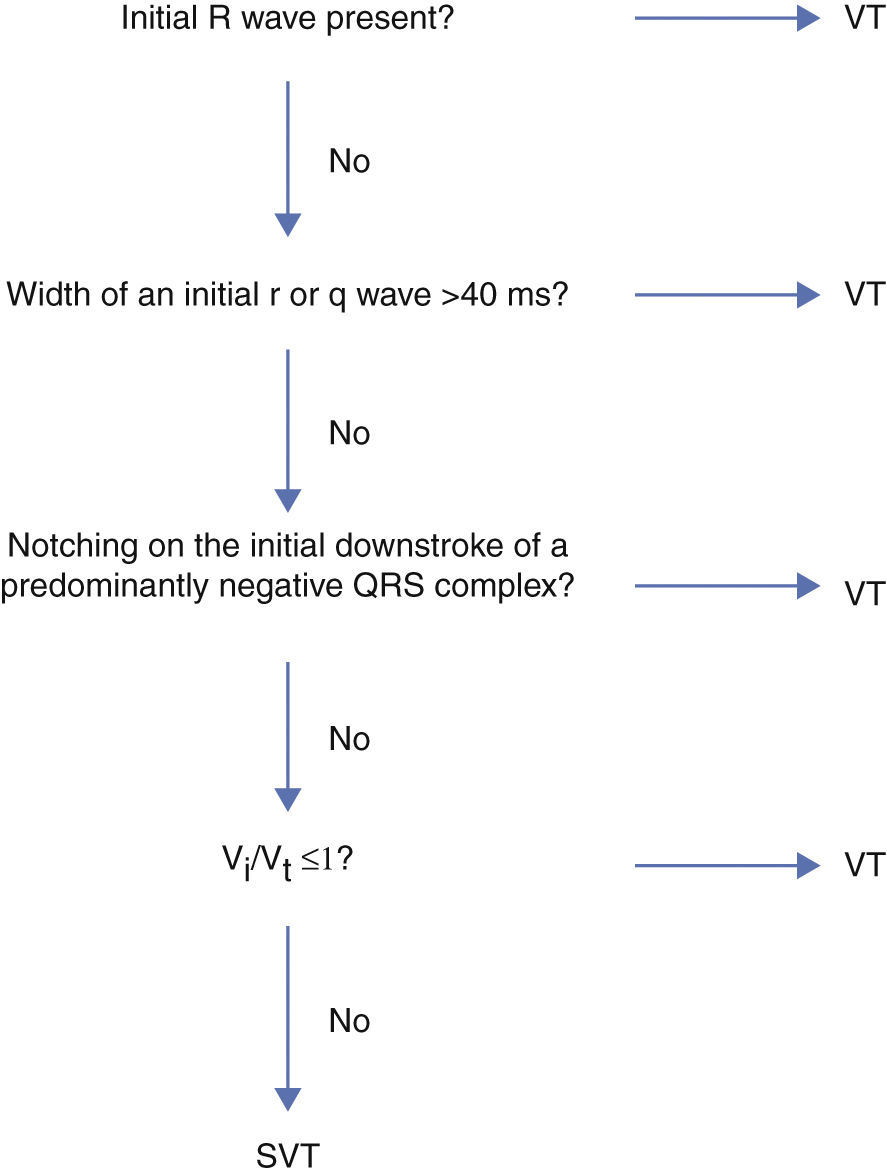
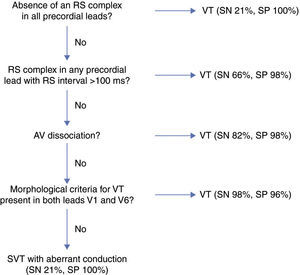
Algorithms for differential diagnosis of wide QRS tachycardiaIn 1991, Brugada et al.9 proposed an algorithm for the diagnosis of wide QRS tachycardia that consisted of four stepwise criteria (Figure 6):
- (1)
Absence of an RS complex in all precordial leads;
- (2)
RS complex in any precordial lead with RS interval >100ms;
- (3)
AV dissociation;
- (4)
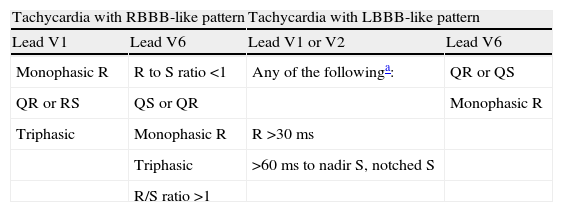
Morphological criteria for VT present in both leads V1 and V6 (Table 1).
Table 1.Morphological criteria for diagnosis of ventricular tachycardias used by Brugada et al.9
Tachycardia with RBBB-like pattern Tachycardia with LBBB-like pattern Lead V1 Lead V6 Lead V1 or V2 Lead V6 Monophasic R R to S ratio <1 Any of the followinga: QR or QS QR or RS QS or QR Monophasic R Triphasic Monophasic R R >30ms Triphasic >60ms to nadir S, notched S R/S ratio >1 LBBB: left bundle branch block; RBBB: right bundle branch block.
Algorithm proposed by Brugada et al.9 for the differential diagnosis of wide QRS tachycardia. SN: sensitivity; SP: specificity; SVT: supraventricular tachycardia; VT: ventricular tachycardia.
If the first criterion is negative, the algorithm moves on to the second, and so on. When one criterion is met, the algorithm halts and a diagnosis of VT is made.
In Brugada et al.’s study, the sensitivity of the four stepwise criteria for the diagnosis of VT was 0.987, and the specificity was 0.965, significantly reducing diagnostic errors.9
However, despite its innovative nature and its value, Brugada et al.’s study has certain limitations. It states that the algorithm has greater sensitivity and specificity than traditional criteria, but does not compare its diagnostic accuracy with them, and the fourth step uses morphological criteria that are difficult to apply in clinical practice. Furthermore, other authors15–17 report lower sensitivity and specificity than Brugada et al.
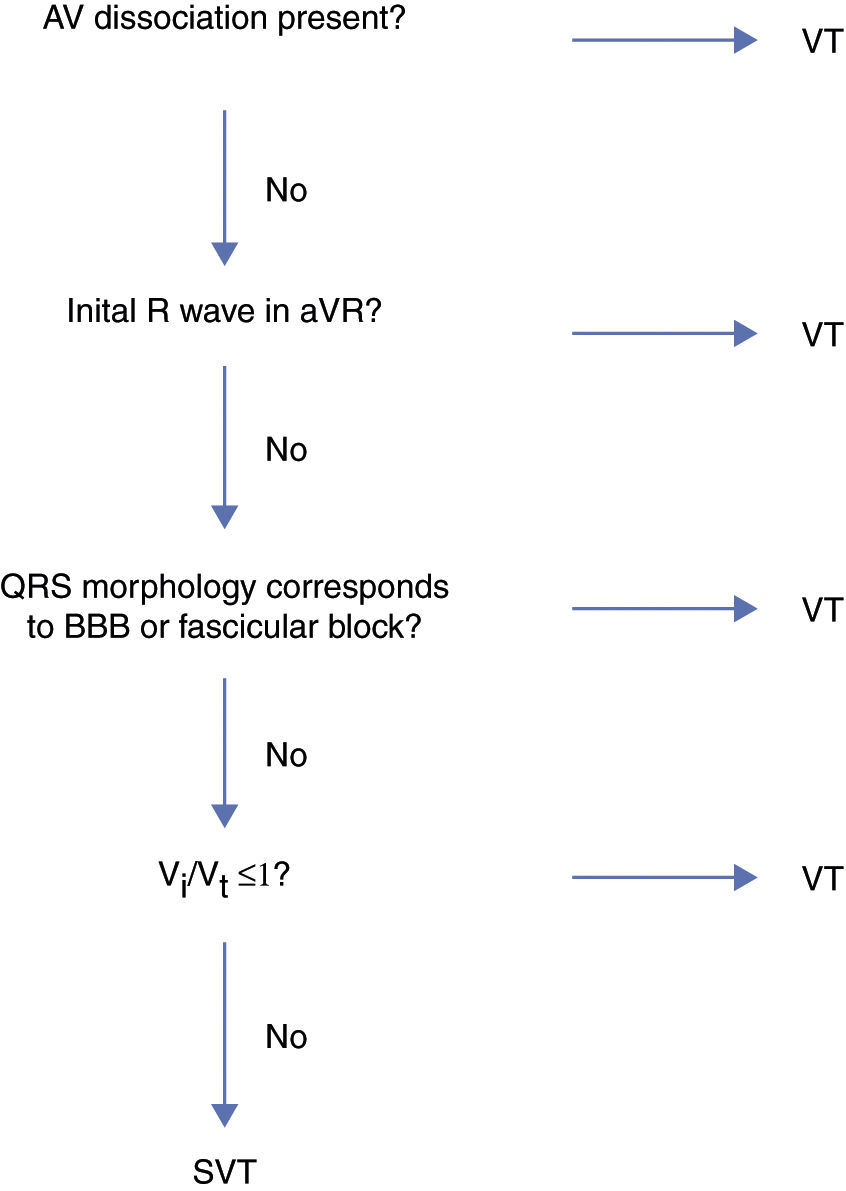
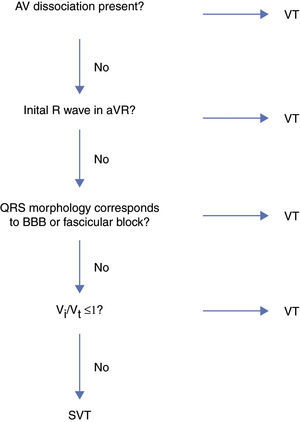
In 2007, Vereckei et al.18 proposed another algorithm for differential diagnosis of wide QRS tachycardia (Figure 7). This algorithm also consists of four steps:
- (1)
If AV dissociation is present, the diagnosis of VT is made and the analysis is stopped.
- (2)
If an initial R wave is present in lead aVR, the diagnosis of VT is made and the analysis is stopped.
- (3)
If the morphology of wide QRS tachycardia does not correspond to BBB or fascicular block, the diagnosis of VT is made and the analysis is stopped.
- (4)
In the last step, when the initial (vi) and terminal (vt) ventricular activation velocity ratio (vi/vt) is ≤1, the diagnosis of VT is made, and if the vi/vt is >1, the diagnosis is SVT.
This algorithm contains two new concepts compared to previous ones:
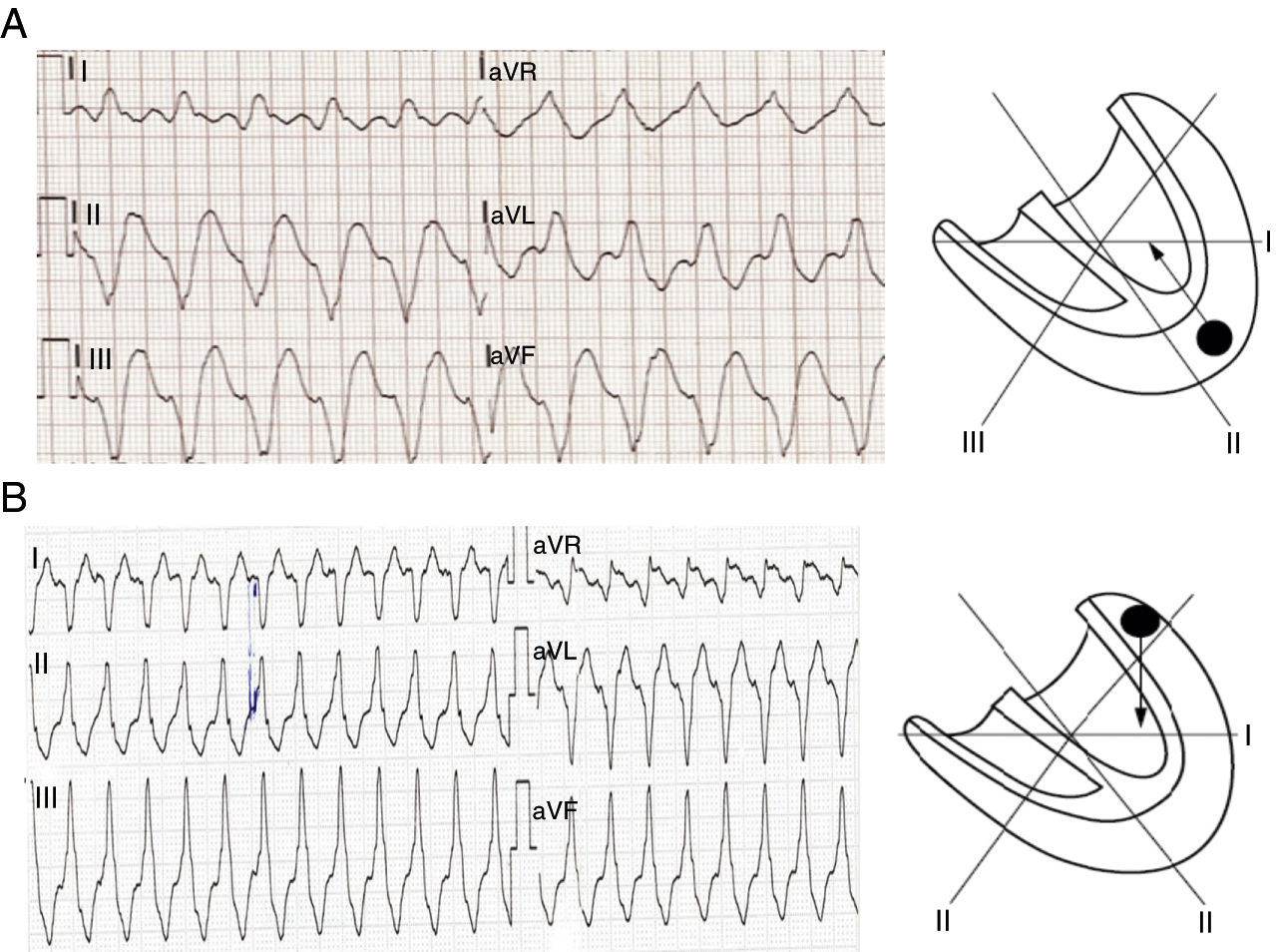
The vi/vt ratioDuring wide complex tachycardia due to SVT, the initial activation of the septum should be invariably rapid and the intraventricular conduction delay causing the wide QRS complex occurs in the mid to terminal part of the QRS. Thus, the conduction velocity of initial ventricular activation should be faster than that of the later or terminal ventricular activation during SVT with aberrant conduction or fixed BBB. During wide complex tachycardia due to VT, however, an initial slower ventricular spread of activation occurs until the impulse reaches the His-Purkinje system, after which the rest of the ventricular muscle is rapidly activated.18
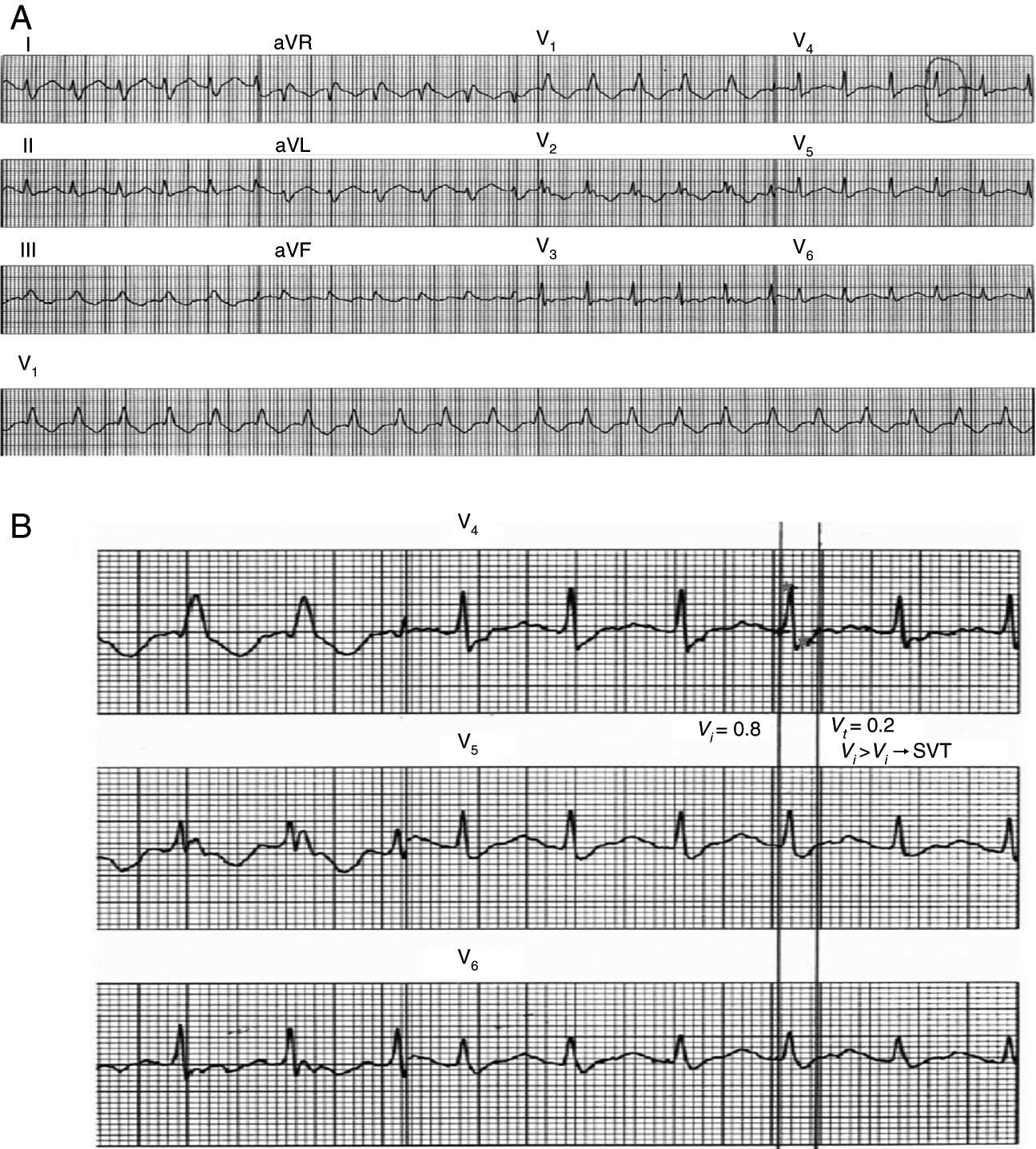
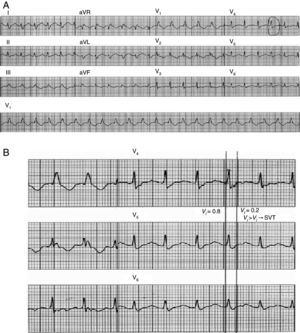
The vi/vt ratio is calculated (Figure 8) by measuring the voltage change on the ECG tracing during the first 40ms (vi) and the last 40ms (vt) of the same QRS complex. A vi/vt ratio of ≤1 is suggestive of VT and a vi/vt ratio of >1 of SVT.
Application of the vi/vt criterion. (A) 12-lead ECG trace of wide QRS tachycardia. vi is measured in a lead showing a biphasic or multiphasic QRS with the most rapid activation velocity. A QRS complex in this lead is selected in which the beginning and end of the complex are clearly visible. (B) Vertical lines mark the beginning and end of the selected QRS complex and small red stars mark the first and last 40ms of the complex. During the first 40ms, the impulse shifts vertically by 0.8mV and thus vi=0.8; during the last 40ms it shifts vertically by 0.2mV and so vt=0.2mV. The vi/vt ratio therefore suggests a diagnosis of supraventricular tachycardia (adapted with permission from Vereckei et al.18).
During SVT with BBB, the ventricular activation wavefront proceeds in a direction away from lead aVR, producing a negative QRS in aVR.19
In the population studied by Vereckei et al., the overall test accuracy of the new algorithm was superior to that of the Brugada criteria.18 This is probably due to the lower accuracy of the fourth Brugada criterion compared to the fourth Vereckei criterion. The new algorithm also had greater sensitivity and specificity than the Brugada criteria.
Like the Brugada criteria, the new algorithm is inherently unable to recognize certain forms of wide QRS tachycardia, including bundle branch reentrant VT, fascicular VT, and SVT involving an atriofascicular accessory pathway unless AV dissociation is present.18 A further limitation is that the initial R wave in aVR may also be seen in patients with left posterior hemiblock and MI,6 and the vi/vt ratio may be influenced by conditions such as anteroseptal MI, scarring at a late activated ventricular site, fascicular VT, and VT exit site close to the His-Purkinje system.19
When the algorithm is applied, care should be taken with placement of the precordial leads and use of antiarrhythmic medication, the presence of congenital heart disease, previous MI and transplantation should be taken into consideration. Although the Vereckei algorithm has been shown to be superior to the Brugada criteria in many cases, it is more time-consuming.
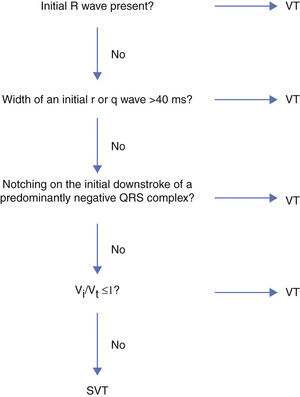
In 2008, Vereckei et al. proposed another new algorithm19 based on the direction and velocity of initial and terminal ventricular activation; it also consists of four steps, but uses the aVR lead only (Figure 9). Although the new algorithm does not contain any fundamentally new criteria, it is based on three novel concepts:
- (1)
selection of lead aVR exclusively for the differential diagnosis of wide QRS tachycardia;
- (2)
classification of VT into two main groups: VT arising from the inferior or apical region of the ventricle yielding an initial R wave in lead aVR, and VT arising from other regions and lacking an initial R wave in aVR but with slowing of the initial part of the QRS complex (this is in contrast to SVT that shows more rapid initial QRS forces);
- (3)
elimination of the AV dissociation criterion and morphological criteria used by all previous algorithms.
Vereckei et al. compared their new algorithm with their previous one and with the criteria proposed by Brugada et al. Although the criterion of AV dissociation is 100% specific, its sensitivity is low since it is difficult to detect on the ECG tracing and its omission did not affect the overall test accuracy of the new aVR algorithm. The algorithm using only the aVR lead was more accurate than that of Brugada et al., with greater sensitivity and specificity for diagnosis of SVT, while there was no statistically significant difference from Vereckei et al.’s previous algorithm.
The new algorithm's superiority over the Brugada criteria is due to the use of the initial R wave and the vi/vt ratio. Although the actual time needed for application of the three algorithms was not measured in the study, the impression of both observers was that the new aVR algorithm was less time-consuming to apply than Vereckei et al.’s previous algorithm and approximately as fast as the Brugada criteria.
The limitations of the new aVR algorithm derive partly from conditions that may influence the vi/vt ratio (see above). Another limitation of the study is the relatively small number of cases of VT occurring in the absence of structural heart disease.
In 2010 a new criterion was proposed, based on analysis of lead II.20 This lead was selected because it is easy to obtain and is found in most ECG rhythm strips recorded in urgent settings.
The rationale for this criterion is that conduction is slower in myocardial tissue than via the His-Purkinje system, and can thus be used to distinguish a ventricular from a supraventricular origin. The criterion is applied by measuring the interval from the beginning of the QRS complex to the peak of the R wave, whether the QRS complex is positive or negative.
In this study, an R-wave peak time of ≥50ms in lead II had sensitivity of 93%, specificity of 99% and positive predictive value of 98% in identifying VT. However, the study did not compare the new criterion with previous ones, and further studies are needed to validate its use.
Whatever criteria or algorithms are used, the real cause of wide QRS tachycardia is misdiagnosed in up to 10% of cases. A reasonable approach is to treat all regular wide QRS tachycardias as VT unless a diagnosis of SVT can be established, since it is better to be wrong in a few cases of SVT treated as VT than the reverse situation (e.g. intravenous verapamil injection may cause severe hypotension and/or VT acceleration and ventricular fibrillation).18
ConclusionDifferential diagnosis of wide QRS tachycardia has both short- and long-term implications. The ECG is the main tool for this, and over the years various criteria and algorithms have been proposed, from Brugada et al.’s innovative four-step algorithm to the algorithm based solely on the aVR lead proposed by Vereckei et al.
Correct application of these algorithms can greatly reduce the number of misdiagnoses. It is, however, important to recognize their limitations. Since most wide QRS tachycardias are VT, a reasonable approach is to treat doubtful cases as if they were VT.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sousa P, Pereira S, Candeias R, de Jesus I. Taquicardia de QRS largos – importância eletrocardiográfica no diagnóstico diferencial. Rev Port Cardiol. 2014;33:165–173.