Biomarkers in dilated cardiomyopathy (DCM) reflect various pathobiological processes, including neurohormonal activation, oxidative stress, matrix remodeling, myocyte injury and myocyte stretch. We assessed the role of biomarkers in clinical and echocardiographic parameters and in left ventricular (LV) reverse remodeling (LVRR).
MethodsIn this prospective study of 50 DCM patients (28 men, aged 59±10 years) with LV ejection fraction (LVEF) <40%, LVRR was defined as an increase of >10 U in LVEF after optimal medical therapy.
ResultsBaseline LVEF was 25.4±9.8% and LV end-diastolic diameter (LVEDD)/body surface area (BSA) was 34.2±4.5 mm/m2. LVRR occurred in 34% of patients within 17.6±15.6 months. No correlation was found between B-type natriuretic peptide (BNP), 25-hydroxyvitamin D (25(OH)D), CA-125, high-sensitivity C-reactive protein (hs-CRP), lipoprotein(a) [Lp(a)], noradrenaline, adrenaline, renin or aldosterone and LVRR. Patients in NYHA class III or IV, with pulmonary congestion or ankle edema, had higher CA-125, cystatin C, BNP and hs-CRP levels (p<0.05). CA-125 was correlated with BNP (r=0.61), hs-CRP (r=0.56) and uric acid (r=0.52) (all p=0.01). BNP correlated directly with LVEDD (r=0.49), LV volumes (r=0.51), pulmonary artery systolic pressure (PASP) (r=0.43) and E/e′ (r=0.31), and was inversely correlated with LVEF (r=-0.50) and e′ velocity (r=-0.32) (p<0.05). CA-125 was positively correlated with left atrial volume/BSA (r=0.46), E/A ratio (r=0.60) and PASP (r=0.49) (p<0.05).
ConclusionsNo correlation was found between biomarkers and LVRR, but CA-125, BNP and hs-CRP were predictors of clinical severity and congestion. BNP correlated with parameters of systolic and diastolic dysfunction, while CA-125 correlated with measures of diastolic dysfunction.
Os biomarcadores na miocardiopatia dilatada (DCM) refletem vários processos fisiopatológicos: ativação neuro-hormonal, stresse oxidativo, remodelagem da matriz extracelular, lesão e estiramento miocitários. Procurámos associar biomarcadores com parâmetros clínicos, ecocardiográficos e com a reversão da remodelagem do ventrículo esquerdo (LVRR).
MétodosEstudo prospetivo de 50 doentes com DCM (28 homens, idade 59±10 anos) com fração de ejeção ventricular esquerda (LVEF) <40%. A LVRR definiu-se como aumento>10 U da LVEF, após a terapêutica médica otimizada.
ResultadosA LVEF basal foi de 25,4±9,8% e o diâmetro do VE (LVD)/BSA de 34,2±4,5 mm/m2. A LVRR ocorreu em 34%, em 17,6±15,6 meses. Não houve correlação entre BNP, 25-OH-vit D, CA 125, hsCRP, Lp(a), noradrenalina, adrenalina, renina, aldosterona e LVRR. Doentes em classe NYHA (III-IV), com congestão pulmonar ou edema periférico apresentaram níveis mais elevados de CA 125, cistatina C, BNP e hsCRP (p<0,05). O CA 125 correlacionou-se com níveis de BNP (r=0,61), hsCRP (r=0,56) e ácido úrico (r=0,52) (p=0,01). O BNP relacionou-se diretamente com LVD (r=0,49), volume VE (r=0,51), PSAP (r=0,43), razão E/e′ (r=0,31); e inversamente com LVEF (r=-0,50) e vel. e′ (r=-0,32) (p<0,05). O CA 125 correlacionou-se com o volume AE/BSA (r=0,46), razão E/A (r=0,60) e PSAP (r=0,49) (p<0,05).
ConclusõesNão houve correlação entre biomarcadores e LVRR, contudo, o CA125, BNP e hsCRP foram preditores de gravidade clínica e de congestão. O BNP relacionou-se com parâmetros de disfunção sistólica e diastólica, enquanto o CA 125 se relacionou com medidas de disfunção diastólica.
Heart failure (HF) is a major public health burden and is often a clinically silent process, with progressive cardiac remodeling that eventually leads to symptomatic presentation late in the course of disease progression. The severity and prognosis of HF vary substantially, ranging from mild disease that is easily managed with neurohormonal blockade to advanced illness requiring mechanical support or heart transplantation.1 Physicians use biomarkers as additional tools to aid clinical diagnosis and treatment and to identify high-risk subjects.2
The progression of HF is complex and is driven by multiple biological processes, including inflammation, oxidative stress, neurohormonal activation, vascular remodeling, myocyte injury, and renal impairment.3 Current guidelines recommend testing B-type natriuretic peptide (BNP) or N-terminal pro-BNP (NT-proBNP).4
The progression of HF is associated with left ventricular (LV) remodeling, which manifests as gradual increases in LV end-diastolic and end-systolic volumes, wall thinning, and a change in chamber geometry to a more spherical, less elliptical shape, with a continuous decrease in LV ejection fraction (LVEF).5 When ventricular remodeling is advanced, it is self-sustaining, leading to disease progression, regardless of neurohormonal status.
However, in some situations, there may be LV reverse remodeling (LVRR), characterized by decreases in LV dimensions, normalization of LV shape and improvement of systolic function.
In this work, we set out to find associations between biomarkers and clinical severity and echocardiographic parameters. We also sought predictors of LVRR after optimal pharmacological therapy. We used available biomarkers that reflect diverse biological pathways in HF: adrenaline, noradrenaline, plasma renin, aldosterone and BNP (neurohormonal activation), high-sensitivity C-reactive protein (hs-CRP), cancer antigen CA-125 (inflammation), uric acid and lipoprotein(a) [Lp(a)] (oxidative stress), creatinine and cystatin C (renal function), and 25-hydroxyvitamin D [25(OH)D] (extracellular remodeling), in a cohort of HF outpatients.
MethodsWe included consecutive adult patients with dilated cardiomyopathy (DCM) followed in an HF outpatient clinic in a tertiary care center, diagnosed less than 24 months previously and with two values of LVEF of <40% more than one year apart. This is a biomarker substudy of a previously published work6 by the same authors. In this new cohort we excluded patients with atrial fibrillation, in order to avoid measurement errors in the assessment of LVEF. We also excluded DCM patients with secondary etiologies including ischemic, valvular, inflammatory and toxic cardiomyopathy.
At baseline, patients underwent clinical assessment of symptoms and signs of HF. Peripheral congestion (ankle edema) and pulmonary congestion were assessed, the latter by lung auscultation and chest X-ray. All patients underwent an electrocardiogram (ECG) and transthoracic echocardiogram and blood laboratory tests. Patients were managed according to current clinical practice guidelines4 and efforts were made to reach the recommended target doses for all therapies. During follow-up, periodic clinical assessment, laboratory tests and echocardiography were performed at three and six months. All patients gave their written informed consent. This study was performed in accordance with the recommendations of the Declaration of Helsinki7 and approved by the hospital's ethics committee.
Definition of left ventricular reverse remodelingLVRR was assessed once optimal medical therapy was reached and was defined as the occurrence in two subsequent echocardiograms, more than six months apart, of an absolute increase of 10 units of LVEF, together with a decrease in LV end-diastolic diameter (LVEDD), without worsening of mitral regurgitation, if present, in the absence of cardiac resynchronization therapy (CRT) or mechanical ventricular assistance. Patients who received CRT were considered not to have LVRR, so only echocardiographic parameters measured before implantation of a CRT device were considered in the analysis.
Transthoracic echocardiography protocolTransthoracic echocardiography was performed at baseline and during follow-up using a commercially available echocardiographic system (General Electric Vivid 7.0) with a 2.5 MHz transducer.
Chamber quantification parameters were measured according to the standards defined by the American Society of Echocardiography and the European Association of Echocardiography.8 LVEF was calculated by Simpson's biplane method; mitral and tricuspid regurgitation was measured by Doppler, scored on a scale from 0 to 4; and pulmonary artery systolic pressure (PASP) was calculated from tricuspid velocities. LV mass was calculated using the formula proposed by Devereux et al.9 The LV sphericity index was calculated as the ratio of dimensions in long-axis and short-axis views. Early diastolic (E) and atrial (A) wave velocities, E/A ratio, and E-wave deceleration time were measured using pulsed wave Doppler recording from apical 4-chamber view. Spectral pulsed-wave Doppler-derived early diastolic velocity (e′) was obtained from the septal mitral annulus, and the E/e′ ratio was calculated to obtain an estimate of LV filling pressure.
All data were stored digitally, and off-line data analysis was performed. To assess variability in interpretation, all echocardiograms were analyzed independently by two specialists in echocardiography, blinded to the study. Reproducibility of the measurements was calculated on the basis of standard error of the estimate; both inter- and intra-observer variation were ≤5% for follow-up LVEF.
Biomarker assessmentAll biomarkers were measured from plasma obtained at the time of study entry.
Blood samples were collected after a 30-min rest through a venous catheter and the first sample was rejected. Plasma catecholamines were determined by high-performance liquid chromatography (Gilson). BNP was measured by chemiluminescent immunoassay (Abbott). Plasma renin activity and aldosterone was determined by radioimmunoassay. hs-CRP was measured by nephelometry (Vista, Siemens). CA-125 and 25(OH)D were determined by chemiluminescence (Abbott and Roche, respectively).
Statistical analysisAll values are reported as mean ± SD, median ± interquartile range, or percentages, according to the characteristics of the data. Differences between subjects in each arm were assessed using the chi-square test for categorical variables and the Student's t test or Mann-Whitney test for continuous variables, as appropriate. A two-tailed p<0.05 was considered to indicate statistical significance.
A paired Student's t test was used to assess changes from baseline. The relationships between biomarkers and echocardiography parameters were analyzed by Spearman's correlation test. Data were analyzed using the SPSS 23.0 statistical package (IBM SPSS Inc., Chicago, IL, USA).
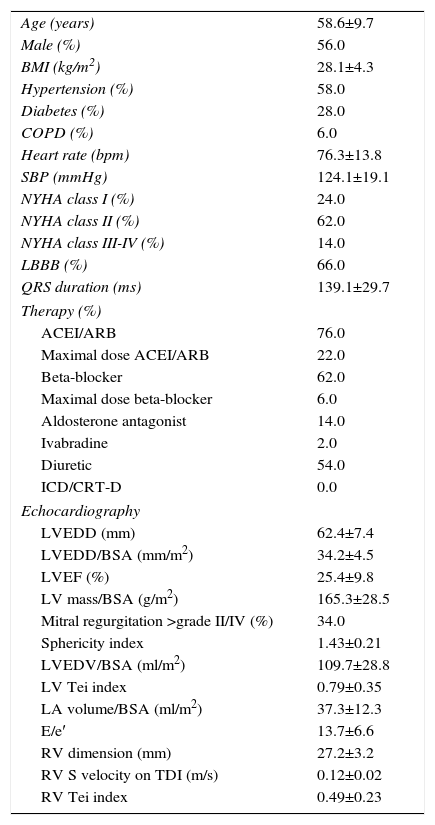
ResultsWe studied 50 patients, 28 men (56%), aged 59±10 years and followed for 39±22 months. The majority of patients (62%) were in New York Heart Association (NYHA) class II. At baseline, mean LVEF was 25.4±9.8%, LVEDD was 62.4±7.4 mm, LVEDD/body surface area (BSA) was 34.2±4.5 mm/m2 and grade >II/IV mitral regurgitation was present in 34% of patients. Table 1 details the patients’ baseline characteristics.
Baseline characteristics of the study population (n=50).
| Age (years) | 58.6±9.7 |
| Male (%) | 56.0 |
| BMI (kg/m2) | 28.1±4.3 |
| Hypertension (%) | 58.0 |
| Diabetes (%) | 28.0 |
| COPD (%) | 6.0 |
| Heart rate (bpm) | 76.3±13.8 |
| SBP (mmHg) | 124.1±19.1 |
| NYHA class I (%) | 24.0 |
| NYHA class II (%) | 62.0 |
| NYHA class III-IV (%) | 14.0 |
| LBBB (%) | 66.0 |
| QRS duration (ms) | 139.1±29.7 |
| Therapy (%) | |
| ACEI/ARB | 76.0 |
| Maximal dose ACEI/ARB | 22.0 |
| Beta-blocker | 62.0 |
| Maximal dose beta-blocker | 6.0 |
| Aldosterone antagonist | 14.0 |
| Ivabradine | 2.0 |
| Diuretic | 54.0 |
| ICD/CRT-D | 0.0 |
| Echocardiography | |
| LVEDD (mm) | 62.4±7.4 |
| LVEDD/BSA (mm/m2) | 34.2±4.5 |
| LVEF (%) | 25.4±9.8 |
| LV mass/BSA (g/m2) | 165.3±28.5 |
| Mitral regurgitation >grade II/IV (%) | 34.0 |
| Sphericity index | 1.43±0.21 |
| LVEDV/BSA (ml/m2) | 109.7±28.8 |
| LV Tei index | 0.79±0.35 |
| LA volume/BSA (ml/m2) | 37.3±12.3 |
| E/e′ | 13.7±6.6 |
| RV dimension (mm) | 27.2±3.2 |
| RV S velocity on TDI (m/s) | 0.12±0.02 |
| RV Tei index | 0.49±0.23 |
ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; BMI: body mass index; BSA: body surface area; COPD: chronic obstructive pulmonary disease; ICD/CRT-D: implantable cardioverter-defibrillator/cardiac resynchronization therapy device; LA: left atrial; LBBB: left bundle branch block; LV: left ventricular; LVEDD: left ventricular end-diastolic diameter; LVEDV: left ventricular end-diastolic volume; LVEF: left ventricular ejection fraction; NYHA: New York Heart Association; RV: right ventricular; SBP: systolic blood pressure; TDI: tissue Doppler imaging.
On the ECG, 66% had left bundle branch block (LBBB), 22% had LV hypertrophy criteria and all were in sinus rhythm.
At the beginning of the study, 76% of patients were being treated with angiotensin-converting enzyme inhibitors (ACEIs)/angiotensin receptor blockers (ARBs), 62% with beta-blockers and 14% with aldosterone receptor antagonists (Table 1).
At the end of follow-up, 94% of the patients were being treated with ACEIs/ARBs, 98% with beta-blockers and 60% with aldosterone antagonists. Optimal recommended doses of ACEIs/ARBs were reached in 42% and optimal doses of beta-blockers were reached in 48%. Only 4% needed urgent transplantation or died (two deaths), 22% were hospitalized for worsening HF and 40% received an implantable cardioverter-defibrillator (ICD). At the end of follow-up only 15 patients had LBBB and LVEF ≤35%. Four (8%) received a cardiac resynchronization therapy device (CRT-D); the others did not receive a CRT-D because of NYHA class I, technical problems, patient refusal, transient LVEF recovery, presence of LV diverticulum or old age.
Prevalence and prognostic value of left ventricular reverse remodelingLVRR occurred in 34% of patients within 17.6±15.6 months (mean time to first echocardiogram to show LV recovery). Patients with LVRR had a final LVEF of 48.9±7.9% (Δ LVEF of 22.4%), and had a significant decrease (p<0.05) in LVEDD (53.5±6.7 mm; Δ LVEDD of ±-7.2 mm), LVEDD/BSA (28.3±3.0 mm/m2), LV end-systolic diameter (LVESD)/BSA (20.5±0.6 mm/m2), LV diastolic volume (145.5±32.7 ml), LV systolic volume (73.6±25.2 ml), LV mass (233.9±68.8 g); and an increase (p<0.05) in sphericity index (1.57±0.18), and only 5.9 patients (n=1) had final ≥grade II/IV mitral regurgitation.
The initial LVEF of patients who recovered LV function was 24.9±9.0% and was not significantly different (p=0.58) from the 26.5±11.2% of those who did not recover.
Patients with LVRR had lower BNP at the end of follow-up (143.5±137.5 vs. 36.9±34.3 pg/ml, p<0.01) and fewer major cardiac events (death or HF hospitalization) (5.9% vs. 33.3; p=0.03) compared to those who did not have LVRR.
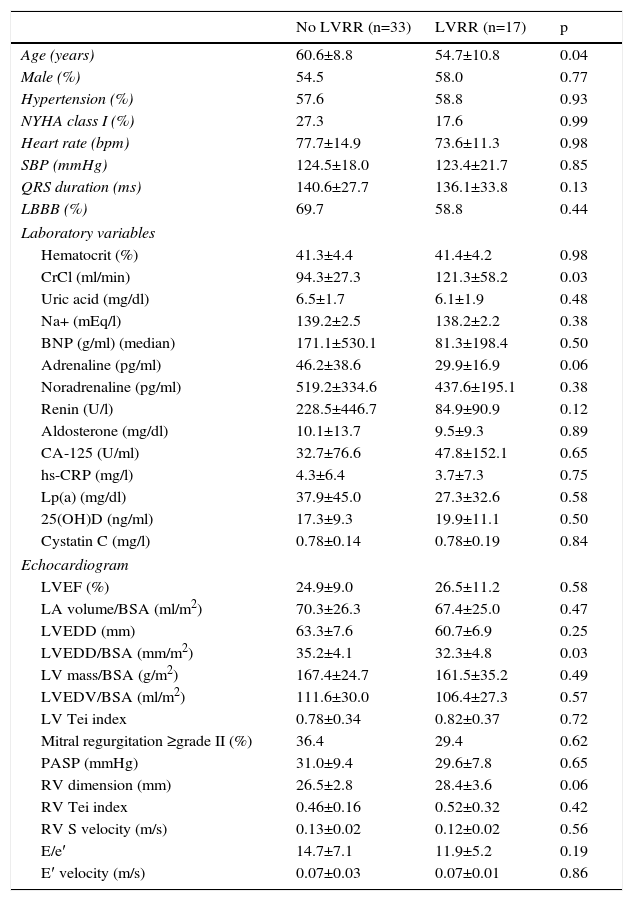
Predictors of left ventricular reverse remodelingBaseline predictors of LVRR are detailed in Table 2. Patients who recovered LV function were younger (60.6±8.8 vs. 54.7±10.8 years, p=0.04) and had a lower LVEDD/BSA ratio (35.2±4.1 vs. 32.3±4.8 mm/m2), p=0.03) and higher creatinine clearance (94.3±27.3 vs. 121.3±58.2, p=0.03). No association was found between levels of 25(OH)D, CA-125, hs-CRP, Lp(a), noradrenaline, adrenaline, renin or aldosterone and reverse remodeling.
Predictors of left ventricular reverse remodeling.
| No LVRR (n=33) | LVRR (n=17) | p | |
|---|---|---|---|
| Age (years) | 60.6±8.8 | 54.7±10.8 | 0.04 |
| Male (%) | 54.5 | 58.0 | 0.77 |
| Hypertension (%) | 57.6 | 58.8 | 0.93 |
| NYHA class I (%) | 27.3 | 17.6 | 0.99 |
| Heart rate (bpm) | 77.7±14.9 | 73.6±11.3 | 0.98 |
| SBP (mmHg) | 124.5±18.0 | 123.4±21.7 | 0.85 |
| QRS duration (ms) | 140.6±27.7 | 136.1±33.8 | 0.13 |
| LBBB (%) | 69.7 | 58.8 | 0.44 |
| Laboratory variables | |||
| Hematocrit (%) | 41.3±4.4 | 41.4±4.2 | 0.98 |
| CrCl (ml/min) | 94.3±27.3 | 121.3±58.2 | 0.03 |
| Uric acid (mg/dl) | 6.5±1.7 | 6.1±1.9 | 0.48 |
| Na+ (mEq/l) | 139.2±2.5 | 138.2±2.2 | 0.38 |
| BNP (g/ml) (median) | 171.1±530.1 | 81.3±198.4 | 0.50 |
| Adrenaline (pg/ml) | 46.2±38.6 | 29.9±16.9 | 0.06 |
| Noradrenaline (pg/ml) | 519.2±334.6 | 437.6±195.1 | 0.38 |
| Renin (U/l) | 228.5±446.7 | 84.9±90.9 | 0.12 |
| Aldosterone (mg/dl) | 10.1±13.7 | 9.5±9.3 | 0.89 |
| CA-125 (U/ml) | 32.7±76.6 | 47.8±152.1 | 0.65 |
| hs-CRP (mg/l) | 4.3±6.4 | 3.7±7.3 | 0.75 |
| Lp(a) (mg/dl) | 37.9±45.0 | 27.3±32.6 | 0.58 |
| 25(OH)D (ng/ml) | 17.3±9.3 | 19.9±11.1 | 0.50 |
| Cystatin C (mg/l) | 0.78±0.14 | 0.78±0.19 | 0.84 |
| Echocardiogram | |||
| LVEF (%) | 24.9±9.0 | 26.5±11.2 | 0.58 |
| LA volume/BSA (ml/m2) | 70.3±26.3 | 67.4±25.0 | 0.47 |
| LVEDD (mm) | 63.3±7.6 | 60.7±6.9 | 0.25 |
| LVEDD/BSA (mm/m2) | 35.2±4.1 | 32.3±4.8 | 0.03 |
| LV mass/BSA (g/m2) | 167.4±24.7 | 161.5±35.2 | 0.49 |
| LVEDV/BSA (ml/m2) | 111.6±30.0 | 106.4±27.3 | 0.57 |
| LV Tei index | 0.78±0.34 | 0.82±0.37 | 0.72 |
| Mitral regurgitation ≥grade II (%) | 36.4 | 29.4 | 0.62 |
| PASP (mmHg) | 31.0±9.4 | 29.6±7.8 | 0.65 |
| RV dimension (mm) | 26.5±2.8 | 28.4±3.6 | 0.06 |
| RV Tei index | 0.46±0.16 | 0.52±0.32 | 0.42 |
| RV S velocity (m/s) | 0.13±0.02 | 0.12±0.02 | 0.56 |
| E/e′ | 14.7±7.1 | 11.9±5.2 | 0.19 |
| E′ velocity (m/s) | 0.07±0.03 | 0.07±0.01 | 0.86 |
25(OH)D: 25-hydroxyvitamin D; BNP: natriuretic brain peptide; CrCl: creatinine clearance; hs-CRP: high-sensitivity C-reactive protein; LA: left atrial; Lp(a): lipoprotein(a); LVEDV: left ventricular end-diastolic volume; LVEF: left ventricular ejection fraction; LVVR: left ventricular reverse remodeling; PASP: pulmonary artery systolic pressure. Other abbreviations as in Table 1.
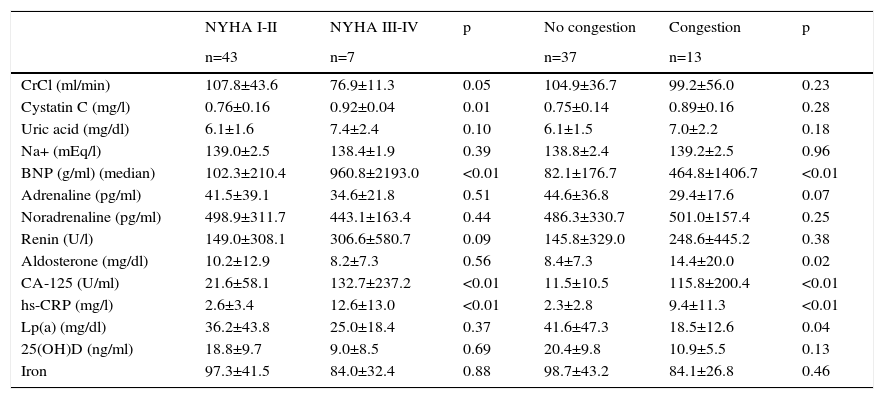
Patients who presented at baseline with worse NYHA class (III/IV) had higher levels of CA-125 (21.6±58.1 vs. 116.0±255.3 U/ml), cystatin C (0.76±0.16 vs. 0.92±0.05 mg/l), BNP (257.5±391.0 vs. 968.5±950.1 pg/ml) and hs-CRP (2.6±3.4 vs. 10.9±13.4 mg/l) (p<0.05) (Table 3).
Biomarkers at clinical presentation.
| NYHA I-II | NYHA III-IV | p | No congestion | Congestion | p | |
|---|---|---|---|---|---|---|
| n=43 | n=7 | n=37 | n=13 | |||
| CrCl (ml/min) | 107.8±43.6 | 76.9±11.3 | 0.05 | 104.9±36.7 | 99.2±56.0 | 0.23 |
| Cystatin C (mg/l) | 0.76±0.16 | 0.92±0.04 | 0.01 | 0.75±0.14 | 0.89±0.16 | 0.28 |
| Uric acid (mg/dl) | 6.1±1.6 | 7.4±2.4 | 0.10 | 6.1±1.5 | 7.0±2.2 | 0.18 |
| Na+ (mEq/l) | 139.0±2.5 | 138.4±1.9 | 0.39 | 138.8±2.4 | 139.2±2.5 | 0.96 |
| BNP (g/ml) (median) | 102.3±210.4 | 960.8±2193.0 | <0.01 | 82.1±176.7 | 464.8±1406.7 | <0.01 |
| Adrenaline (pg/ml) | 41.5±39.1 | 34.6±21.8 | 0.51 | 44.6±36.8 | 29.4±17.6 | 0.07 |
| Noradrenaline (pg/ml) | 498.9±311.7 | 443.1±163.4 | 0.44 | 486.3±330.7 | 501.0±157.4 | 0.25 |
| Renin (U/l) | 149.0±308.1 | 306.6±580.7 | 0.09 | 145.8±329.0 | 248.6±445.2 | 0.38 |
| Aldosterone (mg/dl) | 10.2±12.9 | 8.2±7.3 | 0.56 | 8.4±7.3 | 14.4±20.0 | 0.02 |
| CA-125 (U/ml) | 21.6±58.1 | 132.7±237.2 | <0.01 | 11.5±10.5 | 115.8±200.4 | <0.01 |
| hs-CRP (mg/l) | 2.6±3.4 | 12.6±13.0 | <0.01 | 2.3±2.8 | 9.4±11.3 | <0.01 |
| Lp(a) (mg/dl) | 36.2±43.8 | 25.0±18.4 | 0.37 | 41.6±47.3 | 18.5±12.6 | 0.04 |
| 25(OH)D (ng/ml) | 18.8±9.7 | 9.0±8.5 | 0.69 | 20.4±9.8 | 10.9±5.5 | 0.13 |
| Iron | 97.3±41.5 | 84.0±32.4 | 0.88 | 98.7±43.2 | 84.1±26.8 | 0.46 |
25(OH)D: 25-hydroxyvitamin D; BNP: natriuretic brain peptide; Congestion: pulmonary congestion or ankle edema; CrCl: creatinine clearance; hs-CRP: high-sensitivity C-reactive protein; Lp(a): lipoprotein(a).
Patients with pulmonary congestion or ankle edema also had higher levels of CA-125, BNP and hs-CRP (p<0.01) (Table 3).
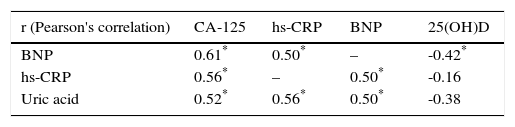
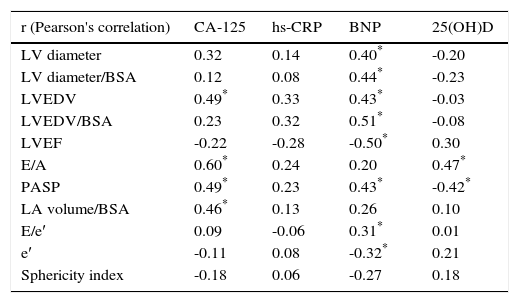
Correlations between biomarkers and with echocardiographic parametersThere was a significant correlation between four biomarkers: CA-125, BNP, hs-CRP and uric acid. BNP also correlated negatively with 25(OH)D (r=-0.43, p<0.05) (Table 4).
We found some correlations between biomarkers and echocardiographic variables (Table 5). BNP correlated directly with LV dimensions (r=0.49), LV volumes (r=0.51), PASP (r=0.43) and measures of diastolic dysfunction (E/e′) and was inversely correlated with LVEF (r=-0.50) and e′ velocities (r=-0.32) (p<0.05).
Correlations between biomarkers and echocardiographic parameters.
| r (Pearson's correlation) | CA-125 | hs-CRP | BNP | 25(OH)D |
|---|---|---|---|---|
| LV diameter | 0.32 | 0.14 | 0.40* | -0.20 |
| LV diameter/BSA | 0.12 | 0.08 | 0.44* | -0.23 |
| LVEDV | 0.49* | 0.33 | 0.43* | -0.03 |
| LVEDV/BSA | 0.23 | 0.32 | 0.51* | -0.08 |
| LVEF | -0.22 | -0.28 | -0.50* | 0.30 |
| E/A | 0.60* | 0.24 | 0.20 | 0.47* |
| PASP | 0.49* | 0.23 | 0.43* | -0.42* |
| LA volume/BSA | 0.46* | 0.13 | 0.26 | 0.10 |
| E/e′ | 0.09 | -0.06 | 0.31* | 0.01 |
| e′ | -0.11 | 0.08 | -0.32* | 0.21 |
| Sphericity index | -0.18 | 0.06 | -0.27 | 0.18 |
CA-125 correlated with LA volume/BSA (r=0.46), E/A ratio (r=0.60) and PASP (r=0.49) (<0.05).
There was a marginal correlation between hs-CRP and LVEF (r=-0.28, p=0.05), and LV diastolic volume/BSA (r=0.32, p=0.05).
Levels of 25(OH)D were only correlated with PASP (r=-0.42) and E/A ratio (r=0.20) (p<0.05).
DiscussionOne of the most important areas of biomarker research is the role of biomarker profiling to better characterize the phenotype of patients who might best respond to therapeutic interventions, whether drug or device therapies.10 The newly-defined HF with recovered LVEF represents a distinct HF phenotype with biochemical properties and natural history that differ from the traditional HF population.11 Predictors of LVRR probably distinguish patients in whom LVEF may recover with medical therapy only from patients who may require cardiac devices or more aggressive strategies, including heart transplantation. Patients who have recovered LVEF do not, in theory, have indications for ICD or CRT therapy, thus complicating the timing of implantation of these devices.
Data now suggest that biomarkers may also be useful to predict or monitor LVRR. A new clinical score, the ST2-R2 score, contains five clinical variables (non-ischemic etiology, absence of LBBB, HF duration, LVEF and beta-blocker treatment) and a remodeling biomarker, soluble toll-like receptor 2 (ST2). A significant relationship was observed between ST2-R2 scores and changes in LVEF, indexed LV sizes, and percentage reduction in LV end-systolic volume index; a similar trend was observed with diastolic parameters.11
Our study set out to find predictors of LVRR. In our population LVRR occurred in one third of DCM patients, who were younger and had better renal function and smaller LVEDD. These results are consistent with other studies. In a large study, LVRR was found in 89 of 242 idiopathic DCM patients (37%) and baseline predictors were higher systolic blood pressure and the absence of LBBB.12 Binkley et al. showed that patients who recovered LV function were younger, had higher systolic blood pressure, lower serum creatinine level, shorter QRS interval, a lower prevalence of diabetes and history of hypertension, were more frequently female and had a lower prevalence of ischemic cardiomyopathy.13
In our population LVRR was also associated with lower BNP at the end of follow-up and with favorable outcome and reduced rate of cardiac events. In a recent study with elderly HF patients, intensified medical therapy led to improvement in LVEF and to reverse remodeling. NT-proBNP guided therapy was associated with a greater improvement in LVEF than symptom-guided therapy in both patients aged 60 to 74 and in those aged ≥75 years.14
We found no association between BNP, 25(OH)D, CA-125, hs-CRP or Lp(a) and LV reverse remodeling. As expected, patients with poorer functional class, pulmonary congestion, or ankle edema had higher BNP levels. Atrial natriuretic peptide and BNP are produced in response to myocardial stretch due to pressure or volume overload.15 In the ICON study, increasing severity of HF, as measured by NYHA functional class16 and symptom severity, correlated directly with increasing BNP concentrations.17 In our study, BNP also correlated with LV dimensions, LV volumes, LVEF, PASP and measures of diastolic dysfunction (E/e′ and e′ velocities). Since BNP is primarily synthesized by cardiomyocytes, it is not surprising that the highest levels are secreted by the LV. Studies have demonstrated that BNP and NT-proBNP levels correlate positively with LV dimensions, volumes, and mass and are inversely related to LVEF; the strongest correlations have been reported for BNP with LV diastolic wall stress consistent with stretch-mediated BNP secretion.18,19 BNP levels increase with greater severity of overall diastolic dysfunction, correlating with indices of filling pressure as well as with indices of compliance and myocardial relaxation.20,21
Serum CA-125, a high molecular weight glycoprotein, is a tumor marker widely used in patients with ovarian cancer.22 Recently, increased serum CA-125 levels, in parallel with catecholamines and natriuretic peptides, have also been documented in patients with HF.23 However, little is known about the biologic role of this substance: whether it simply reflects increased activation of the cytokine pathway or is an active substance actually responsible for myocardial and/or peripheral dysfunction. In our population, CA-125 was not a predictor of LVRR, but did predict more severe presentation as shown by worse functional class and pulmonary and peripheral congestion. It also correlated with measures of diastolic dysfunction (LA volume, E/A ratio and PASP), as well as with BNP levels, hs-CRP and uric acid, suggesting a potential pathogenic link between inflammatory activation and this marker of systemic congestion. Kouris et al. showed that patients in NYHA classes III and IV had significantly higher mean CA-125 values than patients in class II; serum CA125 levels correlated weakly with PASP and renal function.24 A study analyzing CA-125 levels and LV dysfunction in patients on hemodialysis showed they were positively correlated with pro-BNP and C-reactive protein (CRP) levels, as well as with LVEDD, LVESD and LV mass index.25
CRP is a plasma protein that participates in the systemic response to inflammation, an important mechanism in the progression of HF. A landmark review showed that CRP concentrations were higher than normal in 70% of HF patients, and were directly related to severity of HF.26 In a recent study of patients with acute HF, both hs-CRP and NT-proBNP were independent predictors of 12-month mortality.27 In our patients, hs-CRP was associated with clinical severity and marginally correlated with measures of systolic dysfunction (LVEF and LVEDV/BSA). In a previous study, CRP levels increased in parallel with NYHA class and were also related to higher readmission and mortality rates.28
Functional vitamin D receptors are present in cardiac cells and their activation affects gene expression, proliferation and contraction of cardiomyocytes. Vitamin D may thus contribute to the development of cardiac hypertrophy and fibrosis.29 In our population, 25(OH)D was not a predictor of LVRR and was only correlated with PASP and E/A. In a study of subjects with HF, LVEDD, LVESD, LVEDV and LVESV were significantly larger and fractional shortening was lower in patients with 25(OH)D <25 nmol/l than with 25(OH)D ≥25 nmol/l (p<0.05); log values of 25(OH)D were negatively correlated with LVEDD and LVEDV (r=-0.28; p<0.05).29
In a recent study of ambulatory patients with chronic HF, Ky et al.30 tested the hypothesis that a group of seven biomarkers (BNP, soluble fms-like tyrosine kinase receptor, hs-CRP, ST2, cardiac troponin I, uric acid and creatinine) could be combined into a multimarker score that would predict risk of adverse outcome, defined as death, cardiac transplantation or ventricular assist device placement. Patients in the highest tertile of the multimarker score had a 13.7-fold increased risk of adverse outcomes compared with the lowest tertile.
The approximate cost per patient of the biomarkers that we used is currently around €100. In-hospital care is responsible for ∼60% of HF-related costs and median hospitalization cost is €9475,4 but in many cases costs are much higher due to frequent comorbidities and need for intensive care. If the use of biomarkers succeeds in preventing just one hospitalization, this could be a highly cost-effective strategy.
Study limitationsIn our center, high-sensitivity troponin I has only been available since last year, so measurements at initial assessment are not available. However, plasma samples have been frozen in liquid nitrogen and a study with emerging biomarkers is ongoing. Due to the small population it was not possible to perform a multimarker score.
ConclusionsIn our population, LVRR occurred in one third of DCM patients, especially in younger patients, with better renal function and smaller LVEDD. We can postulate that patients with long-standing disease and larger LV diameters may not recover LV function. CA125, BNP and hs-CRP were predictors of clinical severity but not of reverse remodeling. BNP correlated with parameters of systolic and diastolic dysfunction, while CA-125 correlated with measures of diastolic dysfunction.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.