Coronary heart disease is the leading cause of death in women worldwide and several studies have shown that they are under‐represented in cardiac rehabilitation therapy. The objectives of this study were to assess the prevalence of women in a cardiac rehabilitation program and to assess their response to this intervention.
MethodsThis is a retrospective study of 858 patients who attended an exercise‐based cardiac rehabilitation program after an acute coronary syndrome or elective percutaneous coronary intervention, between January 2008 and December 2012. The patients were analyzed by gender, and the impact of the intervention on cardiovascular risk factors and NT‐proBNP was studied. In a subgroup of 386 patients the impact on functional capacity, resting heart rate, chronotropic index and heart rate recovery was also analyzed.
ResultsOnly 24% of the 858 patients who attended the program were women. Women showed statistically significant improvements in all cardiovascular risk factors, NT‐proBNP, functional capacity and heart rate recovery (p<0.05) after the program. There were also improvements in resting heart rate and chronotropic index, but these were not statistically significant (p=0.08 and p=0.40, respectively) and when the improvements in these two parameters were compared between genders, there was no statistically significant difference (p=0.33 and p=0.17, respectively).
ConclusionsOnly 24% of the patients attending the program were women. We found that they benefited from cardiac rehabilitation therapy, with significant improvements in cardiovascular risk factors and in most of the prognostic markers studied.
A doença coronária representa a principal causa de morte das mulheres no mundo e diversos estudos documentam uma sub‐representação destas na terapêutica de reabilitação cardíaca. Os objetivos deste estudo foram descrever a prevalência das mulheres num programa de reabilitação cardíaca e avaliar a resposta deste subgrupo a esta intervenção.
MétodosEstudo retrospetivo constituído por doentes que frequentaram um programa de reabilitação cardíaca baseado no exercício, após síndrome coronária aguda ou intervenção coronária percutânea eletiva, entre janeiro de 2008 e dezembro de 2012. Os 858 doentes foram divididos pelo género e estudou‐se o impacto desta terapêutica sobre os fatores de risco cardiovascular e NT‐proBNP, e numa subpopulação de 386 doentes sobre a capacidade funcional, frequência cardíaca em repouso, índice cronotrópico e recuperação cronotrópica.
ResultadosDos 858 doentes que frequentaram o programa apenas 24% eram mulheres. Verificou‐se de forma estatisticamente significativa que após o programa as mulheres apresentaram uma melhoria de todos os fatores de risco cardiovascular, NT‐proBNP, capacidade funcional e recuperação cronotrópica (p < 0,05). Em relação à frequência cardíaca em repouso e ao índice cronotrópico observou‐se uma melhoria, mas esta não foi estatisticamente significativa (p = 0,08; p = 0,40). No entanto, quando comparada a melhoria destes dois parâmetros entre géneros, esta não teve significado estatístico (p = 0,33; p = 0,17).
ConclusõesApenas 24% dos doentes a frequentarem o programa eram mulheres. Verificamos que estas beneficiaram do programa de reabilitação cardíaca com melhoria significativa dos fatores de risco cardiovascular e da maioria dos marcadores de prognóstico estudados.
Cardiovascular disease is the leading cause of death worldwide,1 and coronary heart disease (CHD) is the most common form. Although traditionally associated with male gender, CHD is also highly prevalent in women,2 and is in fact the leading cause of death among women in Europe (23%), surpassing other more high‐profile diseases such as breast cancer (3%).3
However, the interest shown by health authorities in CHD in women is due not only to its high prevalence in this patient group, but also to the troubling fact that various studies have demonstrated that women are under‐represented in treatments with prognostic impact in CHD, particularly drug therapy and revascularization.4–9
Cardiac rehabilitation programs (CRPs), another therapeutic modality with proven prognostic impact in CHD,10–13 are underused in both sexes,14 but particularly in women. Several studies have shown that the level of participation in CRPs is consistently lower in female CHD patients.15–18
The objectives of this study were to assess the prevalence of women in our CRP and the clinical impact of this intervention in this patient subgroup.
MethodsStudy designWe performed a retrospective analysis of 858 patients with CHD who attended a CRP at Hospital de Santo António, Porto, after an acute coronary syndrome or elective percutaneous coronary intervention (PCI), between January 2008 and December 2012. Patients who attended at least 80% of the CRP sessions were included. A subgroup of 386 patients for whom data were available on exercise testing during the program was analyzed with regard to the parameters assessed by this exam.
Cardiac rehabilitation programThe CRP at our center is coordinated by a cardiologist and a physiatrist, and also includes specialists in vascular surgery, psychiatry, urology and endocrinology, as well as physiotherapists, nutritionists, nurses and social workers. Patients are referred following hospitalization in a cardiology ward or from cardiology outpatient clinics.
The program is organized in separate, sequential phases in accordance with international guidelines.19 Phases I and II were included in this study.
Phase I begins during hospitalization, and includes educating patients about their disease and control of cardiovascular risk factors; they are also encouraged to regain mobility in the ward, depending on their clinical condition.
Phase II takes place in the Cardiovascular Prevention and Rehabilitation Unit of our center on an outpatient basis, beginning 1–2 weeks after hospital discharge. An initial clinical assessment is performed by the specialist in physical medicine and rehabilitation, focusing on the cardiopulmonary, musculoskeletal and neurological systems. Patients are then referred for laboratory tests aimed at guiding strategies to control cardiovascular risk factors and for exercise testing to stratify cardiac risk with a view to prescribing an exercise program in accordance with international guidelines.19 Patients can also be referred for consultations in vascular surgery, endocrinology, psychiatry, urology, smoking cessation and nutrition depending on clinical indications. This is followed by 8–12 weeks (depending on the patient's clinical situation and response) of health education sessions for the patient and their relatives and supervised exercise sessions. The latter are held in groups of nine patients, with continuous telemetry and heart rate (HR) monitoring, under the supervision of the cardiologist and/or physiatrist, in accordance with current guidelines.19 The exercise sessions are held twice weekly, each lasting approximately 60 minutes, and include a warm‐up period, aerobic training, strength training (using dumbbells, exercise balls and other strength training equipment), a cool‐down period and flexibility exercises. The aerobic component occupies most of the session (40 minutes), using a treadmill and arm and leg ergometers. The intensity of each exercise is determined on the basis of the patient's exercise HR calculated by the Karvonen formula19 (50–80% of HR reserve determined during exercise testing), complemented by the patient's rating of perceived exertion on the Borg scale.19,20 In addition, patients are encouraged to exercise during the rest of the week at the same level of intensity as that prescribed for the supervised sessions in terms of training HR and Borg scale and aimed at achieving the target values recommended in international guidelines for weekly energy expenditure. Patients are re‐assessed at the end of phase II through repeat laboratory tests and exercise testing.
Study variablesCharacterization of the study populationThe study population was analyzed by gender in terms of the following parameters: age, reason for referral to the CRP (myocardial infarction or elective PCI), cardiovascular risk factors (hypertension, dyslipidemia, diabetes, smoking and overweight/obesity), left ventricular systolic function (assessed qualitatively by transthoracic echocardiography, with dysfunction classified as mild, moderate or severe), N‐terminal pro‐brain natriuretic peptide (NT‐proBNP), quantified by the central laboratory of our hospital and expressed in pg/ml, and medication (aspirin, clopidogrel, statins, beta‐blockers, angiotensin‐converting enzyme [ACE] inhibitors and angiotensin receptor blockers [ARBs]).
Parameters of response to cardiac rehabilitation programThe response to the CRP was analyzed according to gender in terms of the effect of the intervention on control of cardiovascular risk factors21–24 and on prognostic markers of CHD (NT‐proBNP, exercise capacity and autonomic nervous system [ANS] regulation, the latter two in a subgroup of 386 patients only).25–31 This was assessed by comparing the results of laboratory tests and exercise testing on initial assessment with those at the end of phase II (after 3 months).
Cardiovascular risk factorsDetermination of metabolic profile included measurement of total cholesterol (TC), low density lipoprotein cholesterol (LDL‐C), high density lipoprotein cholesterol (HDL‐C) and triglycerides (TG), and body mass index (BMI) was calculated. In diabetic patients, fasting blood glucose and hemoglobin A1C (HbA1C) were also assessed. Laboratory tests were performed on blood samples collected after 12 hours’ fasting.
NT‐proBNPNT‐proBNP levels were measured.
Functional capacityFunctional capacity was assessed based on metabolic equivalents (METs) obtained during exercise testing.
Autonomic nervous system regulationThe following parameters from exercise testing were analyzed: resting HR, chronotropic index and HR recovery.
The chronotropic index was calculated using the following equation: [(peak exercise HR − resting HR)/(220‐age)‐resting HR] × 100, expressed as a percentage.
HR recovery was assessed as the difference between peak exercise HR and HR after one minute of the recovery period, expressed in beats per minute (bpm).
Statistical analysisQualitative variables were presented as percentages and compared by the chi‐square test, and quantitative variables as means ± standard deviation and compared by the Student's t test. Values of p<0.05 were considered statistically significant. The statistical analysis was performed using Stata® version 12.0.
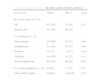
ResultsCharacteristics of the study populationThe study population consisted of 858 patients, of whom 24% were women (Table 1). Most patients were referred to the CRP following a diagnosis of myocardial infarction (69% of women and 68% of men). Female patients were significantly older (62±11 years vs. 60±11 years, p=0.01) and presented a higher prevalence of cardiovascular risk factors, particularly hypertension (70% vs. 57%, p<0.001), dyslipidemia (83% vs. 72%, p=0.001) and diabetes (37% vs. 28%, p=0.04). There was a higher percentage of smokers among men (36% vs. 22%, p<0.001). The prevalence of overweight and obesity was similar in both sexes (68%). Women presented higher baseline NT‐proBNP (1050±1759 pg/ml vs. 660±881 pg/ml, p<0.001) and more frequently had left ventricular systolic dysfunction (40% vs. 28%, p=0.01).
Characteristics of the study population.
| M (76%, n=651) | F (24%, n=207) | p | |
| Age (years) | 60±11 | 62±11 | 0.01 |
| Reason for referral, % (n) | |||
| MI | 68 (443) | 69 (143) | 0.85 |
| Elective PCI | 32 (208) | 31 (64) | |
| CV risk factors, % (n) | |||
| Hypertension | 57 (371) | 70 (145) | <0.001 |
| Dyslipidemia | 72 (469) | 83 (172) | 0.001 |
| Diabetes | 28 (182) | 37 (77) | 0.04 |
| Smoking | 36 (234) | 22 (46) | <0.001 |
| Overweight/obesity | 68 (443) | 68 (141) | 0.98 |
| LV systolic dysfunction, % (n) | 28 (182) | 40 (83) | 0.01 |
| NT‐proBNP (pg/ml) | 660±881 | 1050±1759 | <0.001 |
CV: cardiovascular; F: female; LV: left ventricular; M: male; MI: myocardial infarction; NT‐proBNP: N‐terminal pro‐brain natriuretic peptide; PCI: percutaneous coronary intervention.
As shown in Table 2, virtually all patients were medicated with dual antiplatelets, statins, beta‐blockers and ACE inhibitors or ARBs at the start of phase II. In our study population, the proportion of women under pharmacological therapy was similar to men for all drug classes.
Pharmacological therapy according to gender.
| M (76%, n=651) | F (24%, n=207) | p | |
| Aspirin, % (n) | 99 (645) | 97 (201) | 0.85 |
| Clopidogrel, % (n) | 93 (605) | 93 (193) | 0.98 |
| Statins, % (n) | 98 (638) | 97 (201) | 0.76 |
| Beta‐blockers, % (n) | 91 (592) | 90 (186) | 0.80 |
| ACEIs/ARBs, % (n) | 91 (592) | 89 (184) | 0.50 |
ACEIs: angiotensin‐converting enzyme inhibitors; ARBs: angiotensin receptor blockers; F: female; M: male.
Analysis of the subgroup of 386 patients with exercise test data in terms of the variables previously studied in the overall study population showed similar results (Tables 3 and 4). Changes in dosage of beta‐blockers in this subgroup during phase II of the program (0–3 months) were analyzed; no statistically significant differences were found between the sexes (an increase in 9±7% of women and in 9±6% of men, and a decrease in 1±0.8% of women and in 1±0.6% of men, p=0.62). The changes were made by the attending cardiologist in outpatient consultations. Beta‐blocker therapy was not begun in any patient during phase II of the CRP.
Characteristics of the subgroup with exercise test data.
| M (78%, n=301) | F (22%, n=85) | p | |
| Age (years) | 59±10 | 60±11 | 0.42 |
| Reason for referral, % (n) | |||
| MI | 65 (196) | 72 (61) | 0.25 |
| Elective PCI | 35 (105) | 28 (24) | |
| CV risk factors, % (n) | |||
| Hypertension | 56 (169) | 67 (57) | 0.06 |
| Dyslipidemia | 73 (220) | 85 (72) | 0.02 |
| Diabetes | 25 (75) | 32 (27) | 0.19 |
| Smoking | 34 (102) | 26 (22) | 0.17 |
| Overweight/obesity | 68 (205) | 66 (56) | 0.65 |
| LV systolic dysfunction, % (n) | 29 (87) | 37 (32) | 0.15 |
| NT‐proBNP (pg/ml) | 636±52 | 742±102 | 0.35 |
CV: cardiovascular; F: female; LV: left ventricular; M: male; MI: myocardial infarction; NT‐proBNP: N‐terminal pro‐brain natriuretic peptide; PCI: percutaneous coronary intervention.
Pharmacological therapy in the subgroup with exercise test data.
| M (78%, n=301) | F (22%, n=85) | p | |
| Aspirin, % (n) | 100 (301) | 99 (84) | 0.60 |
| Clopidogrel, % (n) | 93 (280) | 96 (82) | 0.30 |
| Statins, % (n) | 97 (292) | 95 (81) | 0.43 |
| Beta‐blockers, % (n) | 93 (280) | 90 (77) | 0.50 |
| ACEIs/ARBs, % (n) | 90 (271) | 86 (73) | 0.22 |
ACEIs: angiotensin‐converting enzyme inhibitors; ARBs: angiotensin receptor blockers; F: female; M: male.
Analysis of the impact of the CRP on control of cardiovascular risk factors reveals that both female and male patients showed significant improvements in all lipid profile parameters and in BMI (Table 5), and diabetic patients of both sexes presented a significant decrease in fasting blood glucose and HbA1C.
Changes in cardiovascular risk factors and NT‐proBNP levels during the program in male and female patients.
| 0 months | 3 months | p | |
| TC (mg/dl) | |||
| M | 176±42 | 153±34 | <0.001 |
| F | 186±36 | 167±37 | <0.001 |
| LDL‐C (mg/dl) | |||
| M | 109±35 | 87±28 | <0.001 |
| F | 114±30 | 95±30 | <0.001 |
| HDL‐C (mg/dl) | |||
| M | 38±10 | 42±11 | <0.001 |
| F | 45±11 | 49±12 | <0.001 |
| TG (mg/dl) | |||
| M | 155±100 | 123±60 | <0.001 |
| F | 144±73 | 121±54 | <0.001 |
| BMI (kg/m2) | |||
| M | 26.7 | 25.9 | <0.001 |
| F | 27.5 | 26.6 | 0.04 |
| Fasting blood glucose (mg/dl) | |||
| M | 131±49 | 114±35 | <0.001 |
| F | 147±63 | 119±45 | <0.001 |
| HbA1C (%) | |||
| M | 6.7±1.4 | 6.2±1.0 | <0.001 |
| F | 7.3±1.7 | 6.8±1.5 | 0.03 |
| NT‐proBNP (pg/ml) | |||
| M | 660±881 | 345±526 | <0.001 |
| F | 1050±1759 | 466±508 | <0.001 |
BMI: body mass index; F: female; HbA1C: hemoglobin A1C; HDL‐C: high density lipoprotein cholesterol; LDL‐C: low density lipoprotein cholesterol; M: male; NT‐proBNP: N‐terminal pro‐brain natriuretic peptide; TG: triglycerides; TC: total cholesterol.
Improvements in metabolic parameters were similar for both sexes, with the exception of a more marked fall in fasting blood glucose in female patients with diabetes (Table 6).
Changes in cardiovascular risk factors and NT‐proBNP during the program according to gender.
| M | F | p | |
| Δ TC (mg/dl) | −23±41 | −19±40 | 0.37 |
| Δ LDL‐C (mg/dl) | −22±33 | −19±33 | 0.46 |
| Δ HDL‐C (mg/dl) | 4±9 | 4±10 | 0.85 |
| Δ TG (mg/dl) | −32±82 | −23±56 | 0.16 |
| Δ BMI (kg/m2) | −0.8±1.0 | −0.8±1.2 | 0.49 |
| Δ Fasting blood glucose (mg/dl) | −17±33 | −28±52 | 0.01 |
| Δ HbA1C (%) | −0.5±0.9 | −0.5±0.8 | 0.78 |
| Δ NT‐proBNP (pg/ml) | −318±621 | −476±739 | 0.02 |
BMI: body mass index; F: female; HbA1C: hemoglobin A1C; HDL‐C: high density lipoprotein cholesterol; LDL‐C: low density lipoprotein cholesterol; M: male; NT‐proBNP: N‐terminal pro‐brain natriuretic peptide; TG: triglycerides; TC: total cholesterol; Δ: variation.
Both female and male patients showed a significant decrease in NT‐proBNP (from 660±881 pg/ml to 345±526 pg/ml in men and from 1050±1759 pg/ml to 466 ± 508 pg/ml in women, p<0.001) (Table 5). The degree of improvement in this marker of ventricular dysfunction was significantly greater in women (476±739 pg/ml vs. 318±621 pg/ml, p=0.02) (Table 6).
Functional capacityThere was a significant improvement in functional capacity following phase II of the CRP in both men and women (from 9.1±2.2 METs to 10.6±2.1 METs in men and from 7.6±1.7 METs to 8.7±1.8 METs in women, p<0.001) that was similar for both sexes (Tables 7 and 8).
Changes in exercise test parameters during the program in male and female patients.
| 0 months | 3 months | p | |
| Functional capacity (METs) | |||
| M | 9.1±2.2 | 10.6±2.1 | <0.001 |
| F | 7.6±1.7 | 8.7±1.8 | <0.001 |
| Resting HR (bpm) | |||
| M | 63±12 | 61±11 | 0.03 |
| F | 69±13 | 66±10 | 0.08 |
| Chronotropic index (%) | |||
| M | 69±18 | 75±18 | <0.001 |
| F | 65±17 | 68±18 | 0.40 |
| HR recovery (bpm) | |||
| M | 23±9 | 26±12 | <0.001 |
| F | 20±9 | 23±9 | 0.005 |
bpm: beats per minute; F: female; HR: heart rate; M: male; METs: metabolic equivalents.
Changes in exercise test parameters during the program according to gender.
| M | F | p | |
| Δ Exercise capacity (METs) | 1.5±1.2 | 1.2±1.1 | 0.08 |
| Δ Resting HR (bpm) | −2±10 | −3±10 | 0.33 |
| Δ Chronotropic index (%) | 5±13 | 3±13 | 0.17 |
| Δ Heart rate recovery (bpm) | 4±11 | 3±9 | 0.82 |
bpm: beats per minute; F: female; HR: heart rate; M: male; METs: metabolic equivalents; Δ: variation.
Female patients presented a significant improvement in heart rate recovery (from 20±9 bpm to 23±9 bpm, p=0.005), and resting HR showed a tendency to fall after the CRP (from 69±13 bpm to 66±10 bpm, p=0.08); there was a non‐significant increase in chronotropic indices (from 65±17% to 68±18%, p=0.40) (Table 7).
Male patients showed a significant improvement in all parameters: resting HR (from 63±12 bpm to 61±11 bpm, p=0.03), chronotropic index (from 69±18% to 75±18%, p<0.001) and HR recovery (from 23±9 bpm to 26±12 bpm, p<0.001) (Table 7).
However, comparison of the degree of change in resting HR and chronotropic index during the CRP revealed no significant differences between the sexes (Table 8).
DiscussionOur study confirmed that women are under‐represented in CRPs, since only 24% of patients in our program were female despite the fact that the percentage of women with CHD is higher than this.32
In our study, women with CHD were significantly older and presented more cardiovascular risk factors than men, in agreement with current evidence.16,33,34 In addition, they presented more severe CHD, as reflected in the greater proportion of female patients with left ventricular dysfunction, higher NT‐proBNP levels and lower baseline function capacity, also as described in the literature.34 Women attending CRPs thus have a higher cardiac risk from the outset.
With regard to pharmacological therapy, we found no differences between the sexes for the various drug classes prescribed, unlike in some previously published studies.4–7
As regards the impact of the CRP on cardiovascular risk factors, there was an improvement in all metabolic parameters in both women and men. Furthermore, the reduction in fasting blood glucose was more marked in female patients with diabetes, and there was a significant and more marked reduction in the prognostic marker NT‐proBNP in women. This may be due to the fact that women present worse blood glucose control and left ventricular function at the start of the CRP, and are thus likely to derive greater benefit from the intervention.
Functional capacity and ANS regulation were analyzed in a subgroup of 386 patients, who had similar characteristics to those of the overall study population. The same differences were observed in both sexes, although without statistical significance for most parameters, due to the smaller sample size.
With regard to the impact of the CRP on ANS regulation, although a high percentage of patients in our sample were taking beta‐blockers, it should be remembered that the literature has consistently confirmed that the prognostic value of the chronotropic parameters assessed is independent of these drugs.30,35–37 In order to compare HR parameters between the sexes at different times during the program, it was necessary to analyze the distribution of beta‐blocker use in the two groups, as well as changes over time. In our sample, the percentages of men and women medicated with beta‐blockers prior to phase II of the CRP did not differ significantly, nor did changes in dosage of the drug. We can thus state that use of beta‐blockers was not a confounding variable.
We found that women improved significantly in functional capacity and HR recovery. Although they also showed improvement by the end of the program in the other markers of autonomic function (resting HR and chronotropic index), this was not statistically significant, unlike in men. This may be due to the small number of women in the study population, the sample not being sufficiently large for results to have statistical significance. Another possible explanation is the higher proportion of diabetic patients in the female group, in whom ANS regulation may have been affected. Nevertheless, no significant differences were found between the two sexes on analysis of improvements in resting HR and chronotropic index.
This study demonstrates that even though women derive considerable benefit from CRPs, they are under‐represented in such programs, which leads us to conclude that they are not receiving appropriate treatment.
There appear to be various reasons for this discrepancy. The traditional view that CHD is a disease of men may contribute to physicians adopting a less aggressive approach to women with CHD. This is also reflected in the fact that women are less aware of the disease38 and are less often treated than men.4–9 There thus appears to be a tendency on the part of attending physicians to refer female patients less to CRPs.17
The fact that women tend to present CHD at older ages and thus with more comorbidities may also explain their lower attendance on such programs. Older women are known to have a higher prevalence of arthritis, osteoporosis and urinary incontinence.34,39,40 In addition, during evaluation for CRPs, women present lower self‐esteem and are more frequently diagnosed with depression, which may mean they are less motivated to attend such programs.34,39
There may be sociocultural reasons for the differences observed between the sexes. Women are generally more involved in domestic tasks, which could mean they have less time available to attend a CRP40,41; the fact that they also tend to exercise less on a regular basis may also be a contributing factor.42
The main limitations of the study are its retrospective design and the lack of a control group of patients not attending a CRP with whom to compare the variables assessed. Another limitation was the small size of the patient subgroup used to analyze functional capacity and ANS regulation, which could explain the lack of statistical significance found in some of these parameters in women. It would also have been useful to include data on coronary anatomy from cardiac catheterization in the characteristics of the study population, since this could have influenced the parameters assessed. It would also have been interesting to prolong follow‐up after the end of phase II of the program, so as to assess whether the impact on cardiovascular risk factors and prognostic markers is maintained over time.
ConclusionsOnly 24% of the patients attending our CRP were women. They were older than the men and presented more cardiovascular risk factors and probably more severe CHD. Women unquestionably benefited from the CRP, showing significant improvements in control of cardiovascular risk factors and in most of the prognostic markers studied.
It is essential that physicians, patients and society at large recognize the under‐representation of women in CRPs, so that appropriate measures can be taken to increase their access to this intervention and thus enjoy its proven benefits.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Anjo D, Santos M, Rodrigues P, et al. Os benefícios da reabilitação cardíaca na doença coronária: uma questão de género? Rev Port Cardiol. 2014;33:79–87.