Syncope is a common symptom that leads to 1% of admissions to hospital emergency departments, and is associated with high costs to the health system. The cardiology department of Faro Hospital has had a syncope unit since July 2007. The aim of this study is to analyze its results in terms of etiological diagnosis and treatment of syncope, using diagnostic flowcharts based on European Society of Cardiology (ESC) guidelines.
MethodsWe conducted a retrospective study of all patients referred to the syncope unit of Faro Hospital between July 2007 and August 2011. We analyzed demographic data, characteristics of syncopal episodes, diagnostic methods, etiology of syncope and treatment. The percentages of syncope of cardiac and uncertain etiology were compared with data from other international syncope units. Statistical analysis was performed using SPSS version 13.0.
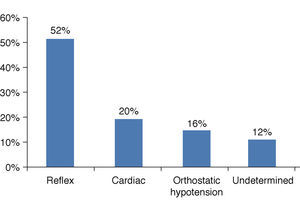
ResultsOf the 304 patients referred to the syncope unit for loss of consciousness, 245 (80.7%) had syncope. Most had reflex syncope (52.2%), 20% had cardiac syncope, 15.6% had orthostatic hypotension, and in 12% of cases etiology remained undetermined. The percentages of cardiac and undetermined etiology were similar to data published by other syncope units.
ConclusionsThe Faro Hospital syncope unit obtained similar results to those published by other international syncope units through application of diagnostic flowcharts for etiological diagnosis of syncope. The flowcharts presented can be of value for the proper application of ESC guidelines on syncope.
A síncope é um sintoma frequente, que motiva 1% das admissões no Serviço de Urgência de um Hospital, estando associada a custos elevados para o Sistema de Saúde. O Serviço de Cardiologia do Hospital de Faro dispõe de uma Unidade de Síncope desde julho de 2007. Pretende-se analisar os resultados obtidos no diagnóstico etiológico e tratamento da síncope, utilizando organigramas de decisão baseados nas Guidelines da European Society of Cardiology (ESC).
Material e métodosFoi realizado um estudo retrospetivo de todos os pacientes referenciados à Unidade de Síncope do Hospital de Faro entre julho de 2007 e agosto de 2011. Foram avaliados os dados demográficos, as características dos episódios de síncope, os meios complementares de diagnóstico utilizados, a etiologia da síncope e o respetivo tratamento. Foi também comparada a percentagem de síncope de etiologia cardíaca e indeterminada com dados de outras Unidades de Síncope Internacionais. Para análise estatística, foi utilizado o SPSS 13.0.
ResultadosDos 304 pacientes referenciados por perda de conhecimento à Unidade de Síncope, 245 (80,7%) apresentaram síncope. A maioria dos pacientes apresentou síncope reflexa (52,2%), 20% apresentou síncope cardíaca, 15,6% hipotensão ortostática e, em 12% dos casos, a síncope permaneceu indeterminada. As percentagens de etiologia de síncope cardíaca e indeterminada são sobreponíveis aos dados publicados por outras Unidades de Síncope.
ConclusõesA Unidade de Sincope do Hospital de Faro através da aplicação de organigramas na investigação etiológica de síncope, obteve resultados equivalentes aos publicados por outras Unidades de Síncope Internacionais. Os organigramas apresentados poderão ser uma mais-valia para a correta aplicação das Guidelines da ESC.
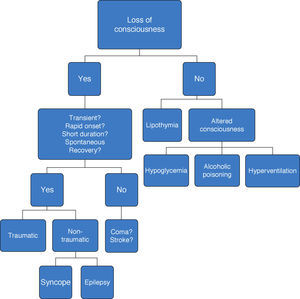
Syncope is defined as loss of consciousness due to transient global cerebral hypoperfusion characterized by rapid onset, short duration, and spontaneous complete recovery.1
The estimated incidence of syncope in the Framingham study was 6.2 per 1000 person-years,2 but lifetime prevalence can reach 50% in certain populations.3,4 However, only a small proportion of these individuals go to a hospital emergency department (ED). In the United States, 1-6% of ED patients have suffered syncope,4–8 while in the Netherlands this figure is 0.7% according to Ganzeboom et al.9 It is estimated that around 1% of ED admissions in Europe are for syncope,1 and of these, 40% of patients are hospitalized10–13; mean hospital stay is 5.5 days (interquartile range 3-9 days),14 entailing high costs.15 Establishing the etiology of syncope also has important prognostic implications, and the diagnostic process should therefore be rapid and accurate.
The European Society of Cardiology (ESC) first published guidelines on management (diagnosis and treatment) of syncope in 2001,3 and an updated version was issued in 2009.1 The latter contains a diagnostic flowchart for initial assessment of a patient with loss of consciousness for differential diagnosis of syncope with other situations with which it may be confused (Figure 1).
It is estimated that initial assessment based on clinical history, physical examination and electrocardiography (Table 1) can determine the etiology of syncope in 23-50% of cases.12,16
Factors associated with probable etiology of syncope on initial evaluation.
| Cardiovascular | Presence of structural heart disease |
| Family history of unexplained sudden death or channelopathy | |
| During exertion, or supine | |
| Abnormal ECG | |
| Sudden onset palpitation followed by syncope | |
| ECG findings suggesting arrhythmic syncope | |
| Neurogenic | Absence of structural heart disease |
| Long history of recurrent syncope | |
| After sudden unpleasant sight, sound, smell or pain | |
| Prolonged standing or crowded, hot places | |
| Nausea, vomiting associated with syncope | |
| During a meal or post-prandial | |
| With head rotation or pressure on carotid sinus | |
| After exertion | |
| Orthostatic hypotension | After standing up |
| After changes in hypotensive medication |
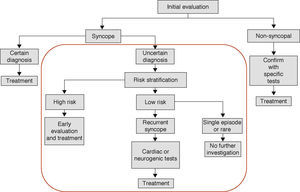
In patients with syncope of uncertain etiology after initial assessment, the 2009 guidelines recommend risk stratification and further investigation of high-risk patients and those at low risk with recurrent syncope, in order to differentiate those who should be further investigated from those who need no further exams (a single syncopal episode in a low-risk patient) (Figure 2).
The ESC guidelines define the high-risk criteria which require prompt hospitalization or intensive evaluation (Table 2). However, the guidelines do not provide flowcharts for investigation of syncope. We consider these essential to facilitate the rapid determination of etiology, and so diagnostic flowcharts have been developed, refined and applied based on the recommendations in the guidelines and the four-year experience of the syncope unit.
High risk criteria in patients with syncope according to European Society of Cardiology guidelines, version 2009.
| High risk criteria which require prompt hospitalization or intensive evaluation |
| Severe structural or coronary artery disease |
| Heart failure or low left ventricular ejection fraction |
| Previous myocardial infarction |
| Clinical or ECG features suggesting arrhythmic syncope |
| Syncope during exertion or supine |
| Palpitation at the time of syncope |
| Family history of sudden cardiac death |
| Non-sustained ventricular tachycardia |
| Bifascicular block (LBBB or RBBB combined with left anterior or left posterior fascicular block) |
| Inadequate sinus bradycardia or sinoatrial block in absence of negative chronotropic medications or physical training |
| Pre-excited QRS complex |
| Brugada ECG pattern |
| ECG findings suggestive of arrhythmogenic right ventricular cardiomyopathy |
| Important comorbidities |
| Severe anemia |
| Electrolyte disturbance |
LBBB: left bundle branch block; RBBB: right bundle branch block.
The aim of this study is to analyze the results of etiological diagnosis and treatment of syncope in the Faro Hospital syncope unit, using diagnostic flowcharts based on the ESC guidelines.
MethodsWe conducted a retrospective study based on a prospective registry of all patients referred to the syncope unit due to a supposed syncopal episode, between July 2007 and August 2011.
Description of the syncope unitFaro Hospital has had a syncope unit since July 2007. It has two sections: one for hospitalized patients in the cardiology department and one in the outpatient building, where most patients are assessed. Patients observed in the hospital's ED who present the criteria described in Table 2 are admitted to the cardiology department, where they are kept under ECG surveillance and diagnostic exams appropriate to the clinical situation are performed, which usually includes repeat 12-lead ECG, routine laboratory tests and transthoracic echocardiogram. When the etiology of the syncope is established, patients are treated accordingly; in cases of uncertain etiology, patients are discharged within 24 hours of admission and referred for outpatient assessment.
Patients who do not meet the criteria for admission are referred directly for outpatient assessment.
The syncope unit also receives patients referred by other hospitals and primary care centers. The unit's protocol follows diagnostic flowcharts based on the ESC guidelines, adapted to the local situation. Syncope due to orthostatic hypotension is not included in the flowcharts since in most cases the diagnosis is established on initial evaluation and does not require further investigation.
Diagnostic flowchartsIf the etiology of syncope remains unclear after initial evaluation, patients are divided into three groups: those with suspected cardiac syncope; those with suspected reflex syncope; and those for whom the available data does not enable them to be classified in either of these groups (syncope of uncertain etiology).
The decision algorithms are not applied to patients diagnosed on initial evaluation, who are immediately referred for appropriate treatment.
Cases in which etiology could not be determined after application of the flowcharts are classified as syncope of undetermined etiology.
The proposed flowcharts for suspected cardiac and reflex syncope and syncope of uncertain etiology are presented below.
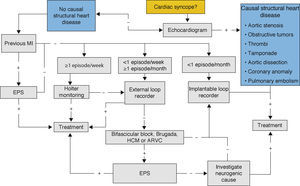
Flowchart for suspected cardiac syncopeIn syncope of suspected cardiac etiology, correct diagnosis of the cause is essential in order to determine prognosis and to implement appropriate therapy.
The flowchart is aimed at rationalizing investigation of the etiology of syncope, thereby reducing costs (Figure 3).
Echocardiography is important in patients with suspected cardiac syncope as it is a non-invasive, readily available exam that can detect structural heart disease as a potential cause, including severe aortic stenosis, thrombi or obstructive cardiac tumors, cardiac tamponade, aortic dissection and congenital anomalous origin of the coronary arteries (class I recommendation, level of evidence B).1 If none of these is found, etiological investigation should continue.
An arrhythmic cause should be excluded through ECG monitoring, the duration and type being determined by the frequency of syncopal episodes. In patients who present at least one episode a week, 24-48-hour Holter monitoring should be performed (class I recommendation, level of evidence B);1 if this is not diagnostic, it should be followed by use of an external loop recorder (Figure 3).
In patients with more than one episode a month, an external loop recorder would be the initial choice due to its three-week recording capacity (class IIa recommendation, level of evidence B).1 If etiology remains uncertain, an implantable loop recorder is indicated, or electrophysiological study if appropriate.
In patients with less than one episode a month, an implantable loop recorder is recommended with battery longevity of up to three years (class I recommendation, level of evidence B).1 Once etiology has been determined, appropriate treatment is instituted.
Syncope without evidence of rhythm disturbances excludes a cardiac etiology, but is still relevant in diagnostic terms. In such cases, a neurogenic etiology should be considered, or the diagnosis of syncope may need to be reconsidered.
Electrophysiological study may be indicated in certain patients with high arrhythmogenic risk, including those with ischemic heart disease (class I recommendation, level of evidence B), bundle branch block (class IIa, level of evidence B), syncope preceded by sudden and brief palpitations (class IIb, level of evidence B) or ECG alterations suggestive of Brugada syndrome, arrhythmogenic right ventricular cardiomyopathy or hypertrophic cardiomyopathy (class IIb recommendation, level of evidence C).1
If the etiology remains uncertain, neurogenic causes should be investigated (Figures 3 and 4).
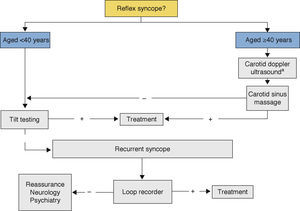
Decision tree for suspected reflex syncope. a Should only be applied in patients with previous transient ischemic attack or stroke within the past three months or with carotid bruits.1
Exercise testing should be performed in patients who have experienced episodes of syncope during or shortly after exertion (class I recommendation, level of evidence C).1
Flowchart for suspected reflex syncopeIn patients with suspected reflex syncope, it is important to direct the investigation according to the patient's age (Figure 4), and we use a cut-off of 40 years, as in the 2009 guidelines.
For patients aged <40 years, reflex syncope can be confirmed through tilt testing if necessary (class I recommendation, level of evidence B).1 In cases of recurrent syncope with negative tilt test, an external or implantable loop recorder should be used to enable accurate diagnosis and appropriate treatment.
For patients aged ≥40 years, carotid sinus massage should be performed (class I recommendation, level of evidence B),1 preceded by carotid Doppler ultrasound to exclude atherosclerotic plaques in patients with previous transient ischemic attack or stroke within the past three months or with carotid bruits.1 If carotid sinus massage is negative, tilt testing should be performed; if this is also negative, then an external or implantable loop recorder should be used for appropriate diagnosis and treatment.
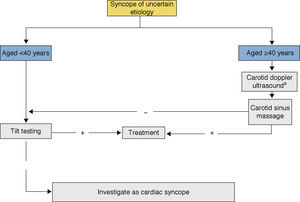
Flowchart for syncope of uncertain etiologyIn patients with syncope of uncertain etiology, neurogenic causes should be investigated first, followed by cardiogenic causes (Figure 5). In individuals aged ≥40 years, besides excluding a neurogenic cause, orthostatic hypotension should be considered, and tilt testing may provide useful data.
Decision tree for syncope of uncertain etiology following initial evaluation. a Should only be applied in patients with previous transient ischemic attack or stroke within the past three months or with carotid bruits.1
Of the 304 patients referred to the syncope unit, 25 (8.2%) presented loss of consciousness of neurological cause, 34 (11.1%) had no loss of consciousness, and 245 (80.7%) were genuine cases of syncope.
The characteristics of these 245 patients were analyzed, including demographic data, characteristics of the syncopal episodes, diagnostic methods, etiology and treatment. In order to determine which factors were associated with cardiac and undetermined etiology, a correlational analysis was performed using the chi-square test for dichotomous and categorical variables and one-way ANOVA for continuous variables, with a level of significance of 95%. Independent predictors of cardiac syncope and syncope of undetermined etiology were then identified through multivariate logistic regression analysis. SPSS version 13.0 was used for the statistical analysis.
ResultsThe characteristics of the patients and syncopal episodes, and the diagnostic methods used to determine etiology, are shown in Table 3.
Baseline characteristics, syncopal episodes and diagnostic exams.
| Baseline characteristics of patients with syncope (n=245) | |
| Male | 126 (51.4%) |
| Mean age (years) | 58±23 |
| Previous history | |
| Tachyarrhythmia | 23 (9.4%) |
| Ischemic heart disease | 16 (6.5%) |
| Stroke/TIA | 15 (6.1%) |
| Bradyarrhythmia | 7 (2.9%) |
| Severe valve disease | 6 (2.4%) |
| Family history of syncope | 27 (11%) |
| Cardiovascular alterations on physical examination | 24 (9.8%) |
| ECG alterations | 59 (24.1%) |
| Frequency of syncope | |
| Recurrent syncope | 189 (77.1%) |
| Single syncopal episode | 56 (22.9%) |
| Position at time of syncope | |
| Standing | 192 (78.4%) |
| Seated | 51 (20.8%) |
| Supine | 2 (0.8%) |
| Presence of trauma | 128 (52.2%) |
| Diagnostic exams | |
| Echocardiogram | 177 (72.2%) |
| Holter ECG monitoring | 150 (61.2%) |
| Exercise test | 48 (19.6%) |
| Tilt test | 39 (15.9%) |
| Carotid ultrasound | 31 (12.7%) |
| Implantable loop recorder | 30 (12.2%) |
| External loop recorder | 29 (11.8%) |
| ABPM | 17 (6.9%) |
| Carotid sinus massage | 7 (2.9%) |
| Stress echocardiogram | 4 (1.6%) |
| Cranial CT/MRI | 4 (1.6%) |
| Electroencephalogram | 3 (1.2%) |
ABPM: ambulatory blood pressure monitoring; CT: computed tomography; MRI: magnetic resonance imaging; TIA: transient ischemic attack.
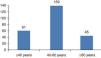
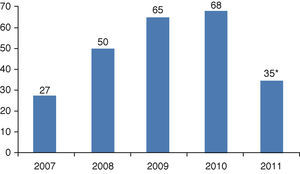
There has been a progressive increase in the number of patients referred to the syncope unit over the four-year study period (to August only in 2011) (Figure 6), a reflection of growing awareness of the unit in the region.
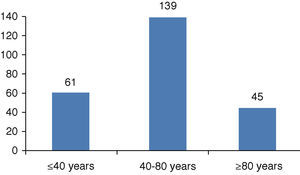
Of the patients assessed for syncope, 51.4% were male. Mean age was 58±23 years (minimum 8, maximum 93); most were in the 40-80 age-group (Figure 7), with 24.9% aged ≤40 years and 18.4% aged ≥80 years.
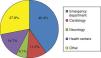
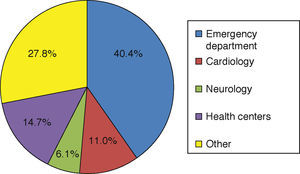
The majority of patients (40.4%) were referred to the unit from the ED (Figure 8), with a significant number from the cardiology and neurology departments; in the latter case, the high number may be due to the fact that differential diagnosis of loss of consciousness can be difficult. The number of referrals from primary health centers was lower than expected, which may be due to patients disregarding symptoms and their physicians thus being unaware of them.
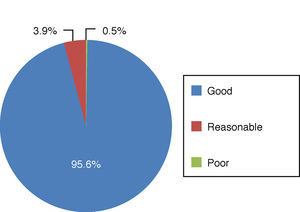
The patients had undergone several diagnostic exams, most prior to referral to the syncope unit (Table 3), but it was decided to include all exams in the analysis, despite the bias that this may introduce. Of patients who had undergone transthoracic echocardiography, 95.6% presented good left ventricular systolic function; only two (0.8%) had alterations considered sufficient to explain their syncopal episodes – one with severe aortic stenosis and the other with hypertrophic cardiomyopathy and high intraventricular gradient (Figure 9).
Of the four patients (1.6%) who underwent dobutamine stress echocardiography, two (50%) presented alterations that could explain syncope.
Exercise testing was performed in 19.6% of patients, alterations suggestive of ischemia being detected in 5.9% of these cases.
Ambulatory blood pressure monitoring was performed in 6.9% of patients, of whom 52% had levels compatible with hypertension and 10% presented periods of symptomatic hypotension.
Carotid Doppler ultrasound was performed in 12.7% of the study population, of whom 8.8% presented >50% stenosis. Carotid sinus massage was performed in only 2.9% of patients, and was positive in two.
Tilt testing, performed in 15.9% of patients, was positive in 76.9% (30.8% mixed response, 17.9% cardioinhibitory response, and 28.2% vasodepressor response).
24-48-hour Holter ECG monitoring was performed in 61.2% of patients, of whom 82.7% had no significant alterations, 12% presented bradyarrhythmia and 5.3% presented tachyarrhythmia. External loop recorders were used in 29 patients (11.8%), which revealed tachyarrhythmia in two (6.9%) and bradyarrhythmia in one (3.4%); the findings were relevant for diagnosis in a further six patients (20.6%), who presented no significant alterations despite the occurrence of syncope.
Implantable loop recorders were used in 30 patients (12.2%), which detected episodes of bradyarrhythmia in 30% and of tachyarrhythmia in 3.3% of cases. One patient (3.3%) had symptoms with no relevant ECG alterations. The exam was negative in 20%, and 13 cases (43.3%) are still under investigation.
Cranial computed tomography and/or magnetic resonance imaging to exclude neurological disease was performed in four patients (1.6%), one of whom had alterations that could explain loss of consciousness. Electroencephalography was performed in three patients (1.2%), and was negative in all of them.
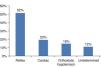
With regard to etiology (Figure 10), the majority of patients (52.2%, n=128) presented reflex syncope, 49 (20%) cardiac syncope, and 38 (15.6%) orthostatic hypotension. Etiology remained undetermined in 30 (12.2%) after diagnostic tests, 13 of whom are still under investigation by means of implantable loop recorders.
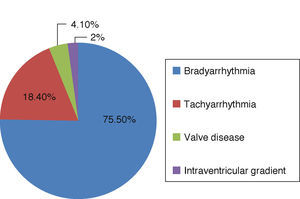
In most patients with cardiac syncope, the underlying mechanism was bradyarrhythmia (Figure 11).
The factors associated with syncope of cardiac etiology were male gender (p=0.011), age ≥40 years (p<0.001), absence of prodromes (p=0.002) and ECG alterations (p<0.001). However, only age ≥40 years (p=0.040), male gender (p=0.032) and ECG alterations (p<0.001) were independent predictors.
The cause remained undetermined in 12.2% of cases. The factors associated with uncertain etiology were non-recurrent syncope (p=0.015), absence of prodromes (p<0.001) and presence of trauma (p=0.040). However, only absence of prodromes was an independent predictor (p<0.001).
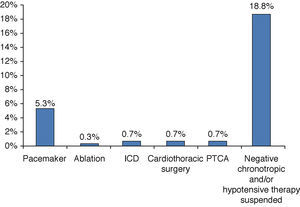
With regard to cardiological treatment, only a small percentage of patients required an invasive approach (Figure 12).
DiscussionThe ESC guidelines recommend the creation of syncope units that can establish a rapid and accurate etiological diagnosis, thus reducing the costs of hospitalization and diagnostic exams. Most syncope units, unlike ours, operate within EDs.
The authors present decision algorithms based on the ESC guidelines and their own four-year experience. In our syncope unit, an etiological diagnosis was obtained in 88% of patients and a diagnosis of cardiac syncope in 20%. These percentages were compared with those from other syncope units cited in the ESC guidelines, so as to gauge our results.
The SEEDS study by Shen et al.,17 a prospective single-center study of a syncope unit within an ED, was designed to assess its efficacy in reducing admissions and improving diagnostic performance in patients with intermediate risk of cardiovascular disease. Of 3502 patients assessed, only 103 were considered at intermediate risk. Diagnostic exams were performed in the syncope unit or within 72 hours of discharge. The study demonstrated a reduction in hospitalizations and total hospital stay, and an increase in etiological diagnosis. The overall diagnostic rate was 82% and the rate of cardiac syncope was 6%.
The EGSYS-2 study by Brignole et al.18 was a prospective multicenter study aimed at improving diagnosis and reducing costs in patients presenting with syncope in EDs and managed in accordance with ESC guidelines. The study showed that a guideline-based approach reduced hospitalizations, hospital stay and the number of exams per patient and improved diagnostic rates. The rate of syncope of undetermined etiology was 5% and that of cardiac syncope was 13%.
A study by Ammirati et al.,19 with both retrospective and prospective components, of 102 patients observed during hospitalization and as outpatients, demonstrated the benefits of a syncope unit. The diagnostic rate was 82%, with 6% having cardiac syncope.
Chen et al.20 analyzed 987 syncope patients referred to an electrophysiological center; rates of undetermined and cardiac etiology were 20% and 37%, respectively.
In a prospective study by Alboni et al.21 of 341 patients, a diagnosis of cardiac etiology was made in 23% and of undetermined etiology in 18%.
Despite differing methodologies, the results from our syncope unit are comparable to those of other European units that have shown benefits in terms of reduced hospitalizations and costs and in improved diagnostic accuracy.
Of the 245 patients assessed in the syncope unit, a diagnosis of cardiac syncope was established in 49 cases (20%), which is within the range reported by other specialist syncope centers (6-37%).1,17–21 However, it should be noted that our data did not include patients who remained hospitalized in the cardiology department following a diagnosis of cardiovascular disease that explained the symptoms, and thus the above percentage is less than the true figure.
With regard to syncope of undetermined etiology, it should be remembered that the elderly constitute a particular population in this respect, given their reduced functional capacity and ability to provide detailed clinical information. Unless there are highly suggestive signs of cardiac etiology, only noninvasive exams that do not require the patient's cooperation are performed. A substantial proportion (33%) of those with syncope of undetermined cause fell into this group. Furthermore, 43% of patients with uncertain etiology are still under investigation by means of implantable loop recorders, and the diagnostic rate is expected to be over 90%. Nevertheless, the percentage of patients with uncertain etiology was similar to that reported by other European syncope units.1
Our findings concerning predictors of cardiac and uncertain etiology differ somewhat from those presented in the ESC guidelines, which may be due to the small number of patients in our study.
With regard to the diagnostic exams used, the discrepancy between the percentage of patients undergoing tilt testing (15.9%) and of those diagnosed with reflex syncope (64.4%) may appear surprising, but is due to the fact that tilt testing is unnecessary in most cases of reflex syncope, since it is only indicated when the etiology is presumed to be neurogenic but doubts remain after initial evaluation. The same applies to carotid sinus massage.
Study limitationsThe study has certain limitations. The fact that the flowcharts were adjusted over the four-year period under analysis means that not all patients were managed according to the same protocol. No comparison was made with a group of patients in whom the diagnostic protocol was not applied. Only patients referred to the syncope unit were analyzed and thus did not include those admitted to the cardiology department, which limits any comparison with other studies. The decision algorithms presented require validation by similar studies in other centers, which we hope will follow publication of our methodology.
ConclusionThe diagnostic flowcharts are designed to simplify etiological investigation of syncope, which in the authors’ opinion can be of value for the proper application of ESC guidelines on syncope. The flowcharts presented were developed on the basis of the ESC guidelines and refined through experience of their application in our hospital's syncope unit, with the aim of facilitating etiological investigation of syncope, particularly in cases of uncertain etiology following initial assessment.
Their application has provided similar results to those reported internationally by other syncope units.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sousa P, Marques N, Faria R, et al. Unidade de Síncope – Experiência de um centro com base em organigramas de decisão para síncope de etiologia incerta após a avaliação inicial. Rev Port Cardiol. 2013;32:581–591.









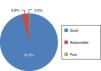




 50%; reasonable: LVEF 30-50%; poor: LVEF <30%.'/>
50%; reasonable: LVEF 30-50%; poor: LVEF <30%.'/>