Sudden cardiac arrest survivors continue to be a challenge for cardiologists. An appropriate initial diagnostic approach is crucial for planning a successful therapeutic strategy. We report the case of a 62-year-old woman who suffered an out-of-hospital cardiac arrest due to third-degree atrioventricular (AV) block. Despite suspected acute coronary syndrome, the coronary angiogram proved inconclusive, while cardiac magnetic resonance imaging ruled out other differential diagnoses such as acute myocarditis. The reversible nature of the AV block rendered permanent pacing unnecessary.
Os sobreviventes de uma paragem súbita cardíaca ainda constituem um desafio para os cardiologistas. Uma abordagem de diagnóstico inicial apropriada é crucial para o planeamento de uma estratégia terapêutica bem sucedida. Apresentamos o caso de uma mulher de 62 anos que sofreu uma paragem cardíaca fora do hospital devida a bloqueio auriculoventricular de terceiro grau. Apesar de suspeita clínica inicial de síndrome coronária aguda, a angiografia coronária foi inconclusiva enquanto a ressonância magnética foi decisiva para excluir outros diagnósticos diferenciais, tais como miocardite aguda. A natureza reversível do bloqueio auriculoventricular evitou a implantação de um pacemaker permanente.
We report the case of a 62-year-old woman, born in Cuba, who had been living in Spain for 5 years at the time of the event. She had a long-standing history of hypertension, dyslipidemia and was an active smoker.
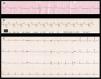
The woman in question was walking down the street when she suddenly suffered a witnessed cardiac arrest. Basic cardiopulmonary resuscitation (CPR) maneuvers were performed for 15 minutes following medical instructions provided by telephone. The emergency outpatient services then started advanced CPR, after registering pulseless electrical activity on the initial electrocardiogram (ECG). Spontaneous circulation eventually returned and the ECG showed a third-degree AV block (Figure 1A).
The patient was transferred to our hospital under neurological sedation and invasive mechanical ventilation. She was also receiving intravenous inotropic agents and transcutaneous pacemaker stimulation. The patient was admitted to the Coronary Unit where mild therapeutic hypothermia was induced after a temporary transvenous pacemaker was implanted. A blood test revealed neutrophilic leukocytosis, increased acute phase reactants and elevated myocardial damage markers (Troponin I peak 21 ng/ml [normal threshold <0.05 ng/ml]), while the ECG showed a pacemaker-stimulated ventricular rhythm with AV dissociation (Figure 1B).
A transthoracic echocardiogram was suboptimal due to a poor acoustic window, so a transesophageal echocardiogram was performed, revealing mildly reduced left ventricular function with akinesia of the mid and basal segments of the interventricular septum.
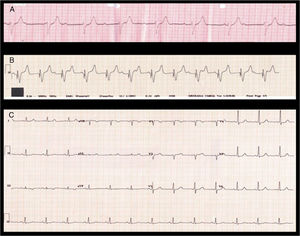
On suspicion of acute coronary syndrome (ACS), a coronary angiogram was performed. The patient was diagnosed with diffuse triple-vessel coronary artery disease, but no severe obstructive lesions were reported (Figure 2).
The patient's family stated that she had not suffered previous episodes of chest pain, but mentioned that she had had flu-like symptoms in the week prior to admission. Given the data obtained thus far, acute viral myocarditis was thought to perhaps be the trigger behind the high-grade AV block and cardiac arrest, so corticosteroids were administered empirically.
During her hospital stay, good neurological status was confirmed by a sedation window, which enabled early extubation after normothermia was achieved. After 72 hours, AV conduction was recovered, initially with complete right bundle branch block, albeit with further QRS narrowing until complete normalization (Figure 1C).
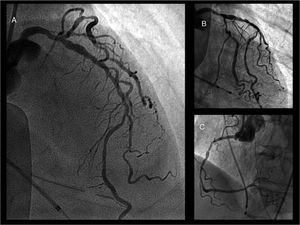
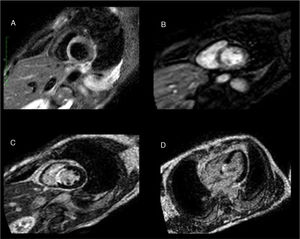
Finally, cardiac magnetic resonance (CMR) imaging was performed, confirming abnormal interventricular septum contractility. An increased short inversion time inversion recovery signal intensity was also observed, indicating edema. Moreover, a subendocardial perfusion defect, alongside transmural delayed enhancement at the same level with no viability, confirmed the diagnosis of acute septal myocardial infarction (Figure 3).
Cardiac magnetic resonance: A) Increased short inversion time inversion recovery signal intensity, indicating septal edema. B) Subendocardial perfusion defect in the same area. C and D) Transmural delayed enhancement at the same level with no viability, confirming the diagnosis of acute septal myocardial infarction.
The coronary angiogram was reviewed and the absence of the first septal branch of the left coronary artery was corroborated, with its occlusion being assumed to be the trigger behind the AV block and cardiac arrest.
Standard treatment for ACS was initiated and the indication for permanent pacing was referred to the Heart Team, who ultimately decided against implantation owing to the ischemic etiology of the transient AV block, which had already been resolved. The patient then completed a cardiac rehabilitation program and has remained asymptomatic ever since.
DiscussionThis particular case shows how difficult a differential diagnosis of ACS and acute viral myocarditis can be, especially if associated with cardiac arrest. Neither the patient's demographic characteristics, blood test results, ECG nor echocardiogram allowed us to be sure of the diagnosis. Moreover, even though the most common cause of cardiac arrest is ischemic heart disease, here the initial coronary angiogram was inconclusive.
In patients with suspected ACS but no coronary obstructive lesions on the coronary angiogram, CMR may prove very useful, since it can detect subtle and reversible coronary events (distal or small arteries, vasospasm).1 CMR enables an accurate differential diagnosis of ACS and myocarditis. Unlike myocarditis, ACS is accompanied by decreased myocardial perfusion in anatomically delimited vascular segments, in addition to characteristic subendocardial or transmural late gadolinium enhancement.2
Another point of discussion is the indication for permanent pacing. When transient, third-degree AV block secondary to ACS has no indication for permanent pacing.3 In this case, where the AV block involved cardiac arrest, the decision was even more important due to its potential prognostic implications. Despite the diagnosis of ACS, for which the patient did not undergo reperfusion therapy, the ECG at discharge did not reveal marked electrical conduction abnormalities besides the QS wave shown in V1 and V2 (Figure 1C). However, care must be taken with an ECG alteration such as this, since placing ECG leads higher up on the chest wall can generate this finding even without the presence of a myocardial infarction.
A similar situation occurs during percutaneous alcohol septal ablation for the treatment of hypertrophic obstructive cardiomyopathy. A high percentage of these patients require a temporary pacemaker in the early post-ablation period, but ultimately less than 10% require permanent pacing due to persistent AV blockage.4
In conclusion, this case allows us to assess the importance of the differential diagnosis of ACS and acute myocarditis. On the one hand, CMR can provide important information to distinguish between both etiologies, while on the other, it is important to highlight that an AV block related to ACS involving the septum does not always require permanent pacing as long as the patient fully recovers AV conduction after the acute phase.
Conflicts of interestThe authors have no conflicts of interest to declare.