Streptococcus agalactiae endocarditis is a rare clinical entity that is generally characterized by acute onset, the presence of large vegetations, rapid valvular destruction and frequent complications, particularly embolization. Mortality is high with medical therapy alone. The authors present a case report of S. agalactiae endocarditis in a young patient treated by prompt surgery. The literature is reviewed.
A endocardite a Streptococcus agalactiae é uma entidade clínica rara. A sua apresentação clínica geralmente tem ínicio agudo, com presença de vegetações de grandes dimensões, rápida destruição valvular e complicações frequentes, nomeadamente embolização. A mortalidade permanece elevada quando é apenas adotada terapêutica médica. Os autores apresentam um caso clínico de uma doente jovem com Endocardite a Streptococcus Agalactiae tratada com uma estratégia cirúrgica precoce e faz-se uma revisão da literatura considerada pertinente.
Streptococcus agalactiae endocarditis is a rare clinical entity, the incidence of which has nevertheless increased in recent years,1 particularly among elderly patients and those with chronic immunosuppressive diseases including alcoholism, diabetes, cancer and HIV infection.2Around 2–9% of cases of S. agalactiae bacteremia present as endocarditis.3–5
The clinical profile of endocarditis caused by this microorganism remains relatively unknown due to lack of data in the literature.
Case reportWe present the case of a 22-year-old woman who went to the emergency department of her local hospital with fever, dry cough, epistaxis, prostration and myalgia of eight days’ evolution, together with recent-onset but progressively worsening dyspnea. There was no known relevant personal history, including drug use or immunodeficiency.
On physical examination the patient was somnolent, tachypneic (respiratory rate: 40cpm), tachycardic (heart rate: 127bpm), normotensive, febrile (axillary temperature: 37.8°C), with hepatosplenomegaly and bilateral ankle edema. Laboratory tests showed normocytic normochromic anemia (hemoglobin: 9.1g/dl), severe thrombocytopenia (11×103/μl), elevated infectious parameters (leukocytes: 11.2×103/μl, neutrophils: 84.5% and C-reactive protein: 17.89mg/dl), and slightly elevated alkaline phosphatase and gamma-glutamyltransferase; blood gas analysis showed alterations compatible with severe hypoxemic respiratory failure. Renal function, coagulation and urinary sediment tests revealed no significant abnormalities.
The chest X-ray showed a bilateral diffuse interstitial pattern.
In the emergency department respiratory failure worsened requiring assisted ventilation. Sepsis originating in the respiratory tract was considered a possibility and the patient was admitted to an intensive care unit and empirical antibiotic and supportive therapy were begun.
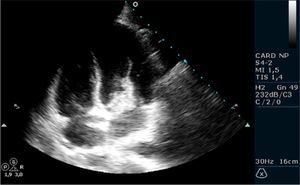
On the second day of hospitalization, following detection of a grade II/VI systolic murmur at the left sternal border and given the context of fever syndrome, transthoracic echocardiography was performed. This revealed a large (30mm maximum diameter), pedunculated, highly mobile vegetation adhering to the atrial side of the mitral valve anterior leaflet and causing moderate to severe mitral regurgitation (Figures 1 and 2); pulmonary artery systolic pressure was estimated at 15mmHg. Transesophageal echocardiography was performed to better characterize the regurgitation mechanism and to exclude perivalvular complications, and confirmed the presence of a large vegetation and severe mitral regurgitation due to the vegetation interfering with valve leaflet coaptation, but excluded abscess, fistula, pseudoaneurysm or perforation.
Blood cultures identified S. agalactiae, highly susceptible to penicillin, and antibiotic therapy was adjusted accordingly.
As pregnancy was suspected, beta-HCG measurement was requested, which was positive (45mIU/ml). The patient was observed by the gynecology department; pelvic ultrasound showed no gestational sac, and the findings were therefore interpreted as recent miscarriage.
Head, abdominal and chest computed tomography excluded septic embolization, and viral serology excluded HIV infection.
In view of the size of the vegetation, high embolic risk and severe mitral regurgitation, the patient was transferred to a surgical center, where a 27-mm St. Jude mitral prosthesis was implanted and the valve annulus was reconstructed using a pericardial patch; there were no postoperative complications.
DiscussionS. agalactiae is a beta-hemolytic gram-positive bacterium that colonizes the female genital tract, the throat and the rectum. It is a frequent cause of neonatal and puerperal infections.7Endocarditis is a rare form of presentation of systemic S. agalactiae infection. The typical patient with S. agalactiae endocarditis in the pre-antibiotic era was a young pregnant woman with mitral disease.3–5
According to the literature, S. agalactiae endocarditis is characterized by acute onset, the presence of large vegetations, rapid valvular destruction and frequent complications.7 One possible complication is systemic embolization, some series reporting a rate of almost 50%, and it is often the first manifestation of the disease. It is thought that vegetation size may be a factor in this high rate of embolic phenomena.4,5,8
The aggressive nature of its clinical course resembles staphylococcal endocarditis more than that caused by other forms of streptococci such as S. viridans.7 However, in contrast to staphylococcal endocarditis, S. agalactiae endocarditis has been rarely observed in patients with prosthetic valves,4,5 only five cases being reported in the last 40years.6
In general, S. agalactiae is penicillin-susceptible (MIC ≤0.1μg/ml),2,5 but its serotypes are slightly more resistant to penicillin that other streptococci, and so maintaining aminoglycoside therapy for 4–6 weeks may be indicated.9,10
In older series in the literature, mortality was 20% with a combined medical and surgical strategy, and 40–50% with medical therapy alone.4,5 In a more recent series of nine patients, Rollán et al. reported overall mortality of 56%, and 33% with prompt surgical treatment; no patient receiving medical therapy alone survived. The authors therefore recommend an early surgical approach.7
This case report draws attention to a rare cause of endocarditis, the incidence of which is growing, and which, as our case illustrates, is usually associated with large vegetations, rapid valvular destruction leading to severe regurgitation, and high embolic risk. Medical therapy alone may be insufficient, and prompt surgery should be considered to improve prognosis.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Machado, C., et al. Endocardite a Streptococcus agalactiae. Rev Port Cardiol 2012. http://dx.doi.org/10.1016/j.repc.2012.01.017.