Cardiogenic shock is a state of inadequate tissue perfusion due to cardiac dysfunction, most commonly caused by acute myocardial infarction. Mortality rates for patients with cardiogenic shock remain frustratingly high, ranging from 50% to 80%. This high mortality can be counteracted by urgent revascularization and these patients benefit from a prompt invasive procedure. We present an unusual case of a patient admitted for an acute anterior infarction and presumable subsequent cardiogenic shock. The urgent coronary angiography revealed an acute stent thrombosis in the anterior descending coronary artery, but the aortography showed that the original cause of shock was actually an abdominal aneurysm rupture. The stent thrombosis and acute anterior infarction were in fact a complication of a hypoperfusion state due to hypovolemic shock.
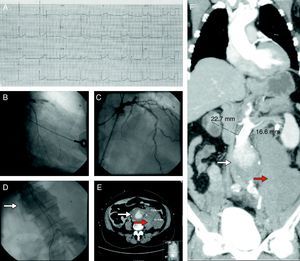
Case reportA 68-year-old man with hypertension, dyslipidemia and ischemic heart disease, with a previous infarction in 2001 when he underwent percutaneous angioplasty of the anterior descending coronary artery, presented at our emergency room with shock, after being found at home unconscious. The patient was confused but was able to report abdominal/dorsal pain (poorly localized) previous to the syncope. The electrocardiogram showed an anterior myocardial infarction (Figure 1, panel A) and the echocardiogram confirmed impaired contractility in the anterior descending artery myocardial territory. Along with fluids and pharmacological therapy, the patient underwent coronary angiography that revealed acute stent thrombosis in the proximal segment of the anterior descending coronary artery (Figure 1, panel B). TIMI 3 flow was reestablished immediately after thrombus aspiration (Figure 1, panel C). Arterial access was obtained via the femoral artery and during the progression of the catheter an abdominal aorta enlargement was suspected. The aortogram confirmed the presence of an abdominal aneurysm with slow flow and subtraction images suggestive of thrombus (Figure 1, panel D, arrow). Computed tomography was promptly performed and confirmed the presence of a ruptured abdominal aneurysm (Figure 1, panels E and F, white arrows) surrounded by a large retroperitoneal hematoma (Figure 1, panels E and F, red arrows). The patient underwent urgent vascular surgery with successful immediate results. The postoperative period was long with multiple complications (infection and abdominal reintervention for correction of bowel perforation due to ischemic colitis). Despite the severity of the initial clinical picture and subsequent complications, all of the latter were promptly and completely resolved and the patient was discharged asymptomatic after 43 days of hospital stay. At nine-month follow-up he was asymptomatic, with preserved left ventricular ejection fraction, completely autonomous and in good general health. This case report highlights the need to observe the patient as a whole, and demonstrates that good results can be achieved, even in serious medical conditions, with expert diagnosis and immediate treatment.
(Panel A) Electrocardiogram showing ST-segment elevation in leads V1–V4 compatible with an anterior myocardial infarction. (Panel B) Coronary angiography showing acute stent thrombosis in the proximal segment of the anterior descending coronary artery. (Panel C) Coronary angiography after thrombus aspiration showing reestablishment of TIMI 3 flow in the anterior descending coronary artery. (Panel D) Aortography revealing an abdominal aneurysm with slow flow and subtraction images suggestive of thrombus (white arrow). (Panels E and F) Computed tomography imaging showing a ruptured abdominal aneurysm (white arrow) surrounded by a large retroperitoneal hematoma (red arrow).
The authors have no conflicts of interest to declare.