Accurate risk stratification is an important step in the initial management of acute coronary syndrome (ACS), and current guidelines recommend the use of risk scores, such as the Global Registry of Acute Coronary Events risk score (GRACE RS). Recent studies have suggested that abdominal obesity is associated with cardiovascular events in patients with ACS. However, little is known about the additional value of abdominal obesity beyond risk scores. The aim of our study was thus to assess whether waist circumference, a surrogate of abdominal adiposity, adds prognostic information to the GRACE RS.
MethodsThis was a retrospective cohort study of ACS patients admitted consecutively to a cardiac care unit between June 2009 and July 2010. The composite of all-cause mortality or myocardial reinfarction within six months of index hospitalization was used as the endpoint for the analysis.
ResultsA total of 285 patients were studied, 96.1% admitted for myocardial infarction (with or without ST elevation) and 3.9% for unstable angina. At the end of the follow-up period, 10 patients had died and the composite endpoint had been reached in 27 patients (9.5%). More than 70% of the study population were obese or overweight, and abdominal obesity was present in 44.6%. The GRACE RS showed poor predictive accuracy (area under the curve 0.60), and most of the GRACE variables did not reach statistical significance in multivariate analysis. The addition of waist circumference to the GRACE RS did not improve its discriminatory performance.
ConclusionAbdominal obesity does not add prognostic information to the GRACE RS to predict six-month mortality or myocardial reinfarction.
A estratificação do risco é um aspeto fundamental da abordagem inicial em doentes com síndrome coronária aguda (SCA) e atualmente as normas de orientação clínica recomendam o uso de modelos de risco, como o Global Registry of Acute Coronary Events Risk Score (GRACE-RS). Estudos recentes sugerem que a obesidade abdominal está associada com eventos cardiovasculares em doentes com ACS. Contudo, pouco é conhecido sobre valor adicional da obesidade abdominal comparativamente com um modelo de risco. Consequentemente, o objetivo do estudo foi avaliar se o perímetro abdominal, um marcador da adiposidade abdominal, acrescenta informação ao GRACE-RS.
MétodosEstudo de coorte retrospetivo de doentes admitidos de forma consecutiva com SCA num hospital português, entre junho de 2009 e julho de 2010. A ocorrência de morte ou re-enfarte do miocárdio no período de seis meses foi utilizada como endpoint.
ResultadosForam estudados 285 doentes, 96,1% com enfarte do miocárdio (com ou sem elevação do segmento-ST) e 3,9% com angina instável. No final do follow-up, 10 doentes morreram e o endpoint foi atingido em 27 (9,5%) dos doentes. Mais de 70% da população era obesa ou apresentava excesso de peso, e 44,6% apresentavam obesidade abdominal. O GRACE-RS apresentou um baixo poder discriminatório (AUC = 0,60), sendo que na análise multivariada a maioria das variáveis GRACE não atingiu a significância estatística. A introdução do perímetro abdominal no GRACE-RS não melhorou o seu poder discriminatório.
ConclusãoA medição da obesidade abdominal não acrescenta informação prognóstica ao GRACE-RS preditor da morte ou re-enfarte aos seis meses de seguimento clínico.
Acute coronary syndrome (ACS) is the leading cause of death in industrialized countries and is thus a major health problem.1,2
Obesity is a growing epidemic and a global healthcare challenge.3,4 It is associated with cardiovascular mortality and with advanced coronary artery disease (CAD).3–6 However, obesity is heterogeneous in terms of metabolic profile and risk implications.7 In this regard, abdominal obesity is increasingly recognized as an important risk factor for cardiovascular disease as well as a major correlate of atherogenic and metabolic abnormalities.7–10 Visceral fat accumulation is a better marker of the cardiometabolic risk associated with obesity than body mass index (BMI).8,11 Adipose tissue is known to be an active endocrine organ. Due to its metabolic activity and anatomic location, abdominal fat secretes large quantities of adipokines and inflammatory cytokines directly into the portal circulation that contribute to the proinflammatory and prothrombotic state of visceral obesity, which may be responsible for the higher attributed risk in abdominally obese subjects.9 Moreover, abdominal obesity is the most prevalent feature of the metabolic syndrome, which is predictive of cardiovascular mortality.12–14 Metabolic syndrome is highly prevalent in ACS patients, and therefore the associated cardiometabolic risk should be assessed in this population.
Direct measures of abdominal obesity, such as waist circumference (WC), might help to better assess fat location and thus improve understanding of obesity-related risk.15 At the population level, increased WC has been independently related to all-cause mortality, myocardial infarction (MI) and CAD risk.16 Although the link between abdominal adipose depot and mortality has been extensively demonstrated in the general population, this relationship appears more complex in ACS patients and requires further clarification. Despite the prevalence of abdominal obesity, few studies have addressed its impact on prognosis after ACS. Recent evidence has demonstrated that elevated WC is associated with increased mortality in patients with CAD.3 It may thus be hypothesized that assessment of WC could improve risk prediction in ACS patients. However, to be a useful tool to predict risk in ACS, it has to demonstrate incremental utility beyond that of an established risk model.17
Clinical management of ACS patients should be guided by a risk estimate.18,19 ACS covers a large spectrum of clinical conditions and for this reason patients are heterogeneous in terms of risk profile for recurrent events. Risk stratification enables tailoring of aggressive medical therapies or invasive procedures towards higher-risk individuals.20,21 Evidence and current guidelines suggest that the benefit of more intensive treatment is related to individual patients’ risk of clinical events.22
To optimize risk assessment, several prognostic factors must be simultaneously taken into account. Risk scores are critical for this purpose. Several risk scores developed in the past decade are currently available to help clinicians with risk stratification. Of those, the Global Registry of Acute Coronary Events (GRACE) risk score (GRACE RS) is probably the most accurate, robust and widespread clinical tool.1 The GRACE RS can be used to estimate the risk of mortality or the combined risk of mortality or MI at admission or at six months. Although the GRACE RS has been extensively evaluated and validated in ACS patients, accurate risk stratification is a difficult and complex task. Little is known about the additional value of abdominal obesity for risk stratification beyond other prognostic variables already used in practice.23 The purpose of the present study was to assess the incremental prognostic value of WC beyond the GRACE RS in a cohort of consecutive patients admitted to a cardiac care unit (CCU) with a diagnosis of ACS.
MethodsStudy populationThe present study is a retrospective cohort study involving 464 patients consecutively admitted for ACS in a CCU of a Portuguese university hospital between June 2009 and July 2010.
Study protocol and data collectionBaseline characteristics were collected prospectively by department clinicians in an internal database. The GRACE RS predicting six-month mortality or MI from hospital admission was retrospectively calculated for each patient using the web calculator (available at http://umassed.org/grace/). Patients without recorded WC measurement, those for whom not all prognostic data required for the GRACE RS calculation was available, and those without complete follow-up at six months from admission, were excluded. The final study population thus included 285 individuals. Some data on the variables studied were missing. The study protocol was approved by the institution's ethics committee.
Definitions of variables of interestThe WC measures were performed using a stretch-resistant tape at the midpoint between the iliac crest and the lower costal arch. For practical purposes, increased WC was defined according to the clinical standard cutoffs of the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) of >88 cm for women and >102 cm for men.
Elevated cardiac enzymes were defined as CK-MB more than double the upper limit of the hospital's normal ranges or as positive troponin I. ST-segment deviation was defined as ST-segment elevation or depression ≥1 mV, seen in any location on the admission ECG. Killip class was recorded at hospital admission. All admission laboratory tests were collected within 24 hours of clinical presentation.
Patients received evidence-based medication and underwent cardiac procedures in a nonrandomized manner according to the physician's criteria and local routines. Standard definitions for in-hospital complications and outcomes were used. Standard pharmacological treatments in accordance with the guidelines were continued at discharge.
Study endpointThe study endpoint was defined as the composite of all-cause mortality or hospitalization for MI within six months of the index diagnosis. Follow-up information was collected by telephone contacts. Medical records were reviewed to identify or confirm clinical events.
Statistical analysisContinuous variables are presented as means (standard deviation) or as medians (interquartile range). Categorical variables are expressed as frequencies (percentage). Pearson's chi-square test or Fisher's exact test were used to compare proportions of categorical variables. The Student's t test or the Mann–Whitney U test was used, as appropriate, to compare differences in continuous variables.
To assess the additional value of WC beyond the GRACE RS, the following procedures were applied: (A) individual variables of the GRACE RS alone (model 1) or associated with WC (model 2) were entered as covariates in binary regression analysis; (B) the predicted probabilities for each model were obtained; (C) these probabilities were used to construct receiver operating characteristic (ROC) curves and the area under the curve (AUC) for each model was calculated to assess discrimination; (D) finally, the two AUCs were compared using the method proposed by Hanley and McNeil.
The GRACE RS was dichotomized according to the best cutoff point on the ROC curve. The dichotomized GRACE RS was related to the endpoint using Pearson's chi-square test.
The statistical analysis was performed with SPSS® 19.0 (SPSS Inc., Chicago, Illinois) and with MedCalc® 12.0.4.0 (Mariakerke, Belgium). All statistical tests were two-sided, and a value of p<0.05 was taken as statistically significant.
ResultsPopulation characteristicsA total of 285 patients were studied. Their mean age was 63±13 years and 78.9% were males; 57.5% were admitted for ST-segment elevation MI (STEMI), 38.6% for non-STEMI (NSTEMI), and the remainder for unstable angina. The median time from symptom onset to CCU admission was 7.0 (103) hours.
As reported in Table 1, the majority of patients had systemic hypertension and dyslipidemia. Diabetes was present in 25.6%, and 48.4% reported current or previous smoking; 14.0% had previous MI and 17.2% previous angina. Chronic renal failure was present in 4.9% of patients.
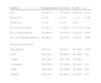
Baseline demographic and clinical characteristics of the study population.
| Variable | Total population | No events | Events | p |
| Age (years) | 62.9 (13.1) | 62.3 (13) | 68.3 (11.8) | 0.023 |
| Male | 225 (78.9) | 205 (79.5) | 20 (74.1) | 0.514 |
| BMI (kg/m2) | 27.6 (0.2) | 27.6 (4.2) | 27.2 (3.2) | 0.568 |
| Waist circumference (cm) | 27.6 (4.1) | 98.5 (11) | 98.7 (6.9) | 0.926 |
| High-risk WC (ATP III) | 127 (44.6) | 114 (44.2) | 13 (48.1) | 0.155 |
| High-risk WC (IDF) | 207 (72.6) | 185 (71.7) | 22 (81.5) | 0.278 |
| Medical history | ||||
| Systemic hypertension | 183 (64.2) | 163 (63.2) | 20 (74.1) | 0.261 |
| Diabetes | 73 (25.6) | 63 (24.4) | 10 (37.0) | 0.153 |
| Dyslipidemia | 155 (54.4) | 137 (53.1) | 18 (66.7) | 0.178 |
| Previous smoking | 54 (18.9) | 53 (20.5) | 1 (3.7) | 0.034 |
| Current smoking | 84 (29.5) | 77 (29.8) | 7 (25.9) | 0.671 |
| Previous angina | 49 (17.2) | 43 (16.7) | 6 (22.2) | 0.467 |
| Previous MI | 40 (14.0) | 35 (13.6) | 5 (18.5) | 0.481 |
| History of chronic renal failure | 14 (4.9) | 7 (2.7) | 3 (11.1) | 0.058 |
| Event classification | ||||
| STEMI | 164 (57.5) | 152 (58.9) | 12 (44.4) | 0.284 |
| NSTEMI | 110 (38.6) | 97 (37.6) | 13 (48.1) | 0.148 |
| UA | 11 (3.9) | 9 (3.5) | 2 (7.4) | 0.288 |
| Clinical presentation | ||||
| Heart rate on admission (bpm) | 75 (18) | 75 (18) | 77(22) | 0.711 |
| Systolic blood pressure (mmHg) | 126 (24) | 125 (24) | 134 (27) | 0.06 |
| Diastolic blood pressure (mmHg) | 77 (14) | 77 (14) | 74 (13) | 0.444 |
| Killip class≥2 | 62 (21.8) | 53 (20.5) | 9 (33.3) | 0.125 |
| Preserved left ventricular function | 139 (49.5) | 125 (49.0) | 14 (53.8) | 0.639 |
| Blood tests | ||||
| Estimated GFR (ml/min/1.73 m2) | 91.43 (38.68) | 93.74 (39.69) | 68.10 (31.8) | 0.002 |
| Creatinine (mg/dl) (median/IQR) | 0.9/5.2 | 0.9/5.2 | 1.1/3.5 | 0.013 |
| Hemoglobin (g/dl) | 14 (1.8) | 14 (1.7) | 13 (2.2) | 0.009 |
| CK-MB (U/l) | 167 (160) | 171 (163) | 130 (126) | 0.202 |
| NT-pro-BNP (pg/ml) (median/IQR) | 1089/69969 | 1033/69969 | 1575/40972 | 0.049 |
| CRP (mg/l) (median/IQR) | 4.20/314.0 | 4.1/314.0 | 8.0/173.4 | 0.022 |
| Peak cardiac troponin I (ng/l) (median/IQR) | 2.66/68 | 2.63/68.0 | 2.99/22.73 | 0.875 |
| Pre-hospital delay (hours) (median/IQR) | 2.2/88.4 | 2.0/88.4 | 4.6/32.1 | 0.015 |
| Length of hospital stay (days) | 6.9 (3.4) | 6.9 (3.8) | 7.3 (3.4) | 0.57 |
| GRACE risk score for six-month mortality or reinfarction | 173 (50) | 171 (49) | 184 (52) | 0.218 |
Continuous variables are shown as mean and standard deviation, if not stated otherwise. Qualitative variables are presented as number and valid percentage. BMI: body mass index; BNP: B-type natriuretic peptide; CK-MB: creatinine kinase type MB; CRP: C-reactive protein; GFR: glomerular filtration rate; IDF: International Diabetes Federation criteria; IQR: interquartile range; MI: myocardial infarction; NCEP ATP III: National Cholesterol Education Program Adult Treatment Panel III criteria; NSTEMI: non-ST-elevation myocardial infarction; STEMI: ST-elevation myocardial infarction; UA: unstable angina.
Patients with the defined endpoint were older (68.3 years vs. 62.3 years, p=0.023), presented with lower glomerular filtration rate (GFR) (68.10 ml/min vs. 93.74 ml/min, p=0.002), higher plasma creatinine (1.1 mg/dl vs. 0.9 mg/dl, p=0.013), significantly higher serum C-reactive protein (CRP) (8.0 mg/dl vs. 4.1 mg/dl, p=0.022) and NT-pro-BNP (1575 pg/ml vs. 1033 pg/ml, p=0.049), and lower admission hemoglobin (13 g/dl vs. 14 g/dl, p=0.009).
Hospital stay was relatively uneventful, with 3 (1.1%) reported deaths and 12 (4.2%) in-hospital reinfarctions. Mean hospital stay was approximately seven days.
Further demographic, clinical and laboratory data are shown in Table 1.
In-hospital management and treatment at dischargeIn general, hospital management and therapy at discharge did not differ between patients with or without events, although higher use of GP IIb/IIIa inhibitors was related to event occurrence. As shown in Table 2, 69.1% of patients underwent coronary revascularization; percutaneous coronary intervention (PCI) was the main reperfusion strategy. The overall rate of discharge therapy in accordance with international guidelines was very high.
In-hospital management and treatment at discharge.
| Variable | Total population | No events | Events | p |
| PCI | 191 (67.3) | 175 (68.1) | 16 (59.3) | 0.352 |
| Rescue PCI | 5 (1.8) | 4 (1.6) | 1 (3.7) | 0.395 |
| Fibrinolysis | 5 (1.8) | 5 (1.9) | 0 (0) | – |
| No revascularization | 83 (29.2) | 73 (28.4) | 10 (37.0) | 0.348 |
| Use of anticoagulants | 269 (94.7) | 245 (94.7) | 24 (92.3) | 0.636 |
| Use of GP IIb/IIIa inhibitors | 48 (16.9) | 40 (15.5) | 8 (30.8) | 0.048 |
| Discharge medications | ||||
| Beta blocker | 264 (93) | 240 (93) | 26 (100) | 0.703 |
| ACEi | 284 (100) | 230 (89.1) | 26 (100) | 1.00 |
| Aspirin | 284 (100) | 258 (100) | 26 (100) | – |
| Clopidogrel | 280 (98.6) | 255 (98.8) | 26 (100) | 0.32 |
| Statin | 284 (100) | 255 (98.8) | 26 (100) | 1.00 |
| Nitrates | 104 (36.7) | 89 (34.6) | 26 (100) | 0.02 |
Qualitative variables are presented as number and valid percent. ACEi: angiotensin-converting enzyme inhibitor; PCI: percutaneous coronary intervention.
At six months from hospital admission, cumulative mortality was 3.5% (10 patients), and there had been 20 reinfarctions (7.1%). The composite endpoint of mortality or MI was thus reached in 27 patients (9.5%).
General and abdominal obesityMore than 70% of the study population were obese or overweight, and almost one third were obese according to World Health Organization (WHO) cutoffs. High-risk WC (NCEP ATP III criteria) was present in 44.6%, and the proportion increased to 72.6% when the International Diabetes Federation (IDF) criteria were used.5,24
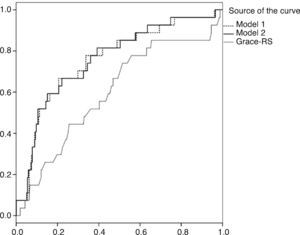
GRACE risk score performance and additional prognostic value of abdominal obesityIn the multivariate model for individual variables from the GRACE RS (model 1), only ST-segment deviation was an independent predictor of the endpoint (odds ratio [OR]=3.56, p=0.038). Elevated cardiac enzymes showed a significant protective effect for event occurrence (OR=0.20, p=0.013). The remaining covariates did not reach statistical significance (Table 3). Model 2 revealed similar results; WC was found not to be an independent predictor of outcome in multivariate analysis (p=0.692). The ROC curves for each multivariate model and for the GRACE RS are illustrated in Figure 1, and the AUCs and other predictive measures are presented in Table 4. The inclusion of WC in the GRACE RS-based model did not improve its discriminatory performance. There were no differences between the AUCs of the two models according to Hanley and McNeil's method. The calculated GRACE RS had a poor discriminatory ability (AUC=0.60): the point for best accuracy on the ROC curve for the GRACE RS was 165. After stratification by the best cutoff value, we found a significant association between high GRACE RS and the endpoint (p=0.026).
Binary logistic regression for predicting six-month mortality or MI using GRACE predictors alone and combined with waist circumference.
| Model 1 | Model 2 | |||
| OR | p | OR | p | |
| Age (10 year increments) | 1.40 | 0.060 | 1.40 | 0.062 |
| Creatinine (0.40 mg/ml increments) | 1.00 | 0.139 | 1.00 | 0.131 |
| Systolic blood pressure (20 mmHg decrements) | 1.02 | 0.124 | 1.06 | 0.114 |
| Heart rate (20 bpm decrements) | 1.24 | 0.652 | 1.25 | 0.707 |
| Killip class | 1.48 | 0.290 | 1.50 | 0.279 |
| Cardiac arrest at admission | 0.26 | 0.265 | 0.26 | 0.261 |
| ST-segment deviation | 3.56 | 0.038 | 3.56 | 0.037 |
| Elevated cardiac enzymes | 0.20 | 0.013 | 0.20 | 0.014 |
| Waist circumference | – | – | 0.99 | 0.692 |
The present study set out to assess whether the inclusion of WC measurement in the multivariate model derived from the GRACE RS improved risk prediction in ACS patients. To the best of our knowledge, this is the first study to quantify the additional predictive value of WC in relation to the GRACE RS.
Our data demonstrated that WC assessment did not improve the predictive accuracy of the GRACE RS. Furthermore, this analysis did not confirm WC measurement as an independent outcome predictor in multivariate analysis. An additional unanticipated result was that the predictive performance of the calculated GRACE RS was shown to be poor.
The study population was mostly composed of males (78.9%); similar proportions were reported in previous studies of ACS populations. Mean age and previous medical conditions were similar to those of the GRACE cohort.16 A higher proportion of STEMI patients was observed (57.5%), compared to ACS registries.18,21 However, our cardiac center receives patients from peripheral hospitals unable to perform PCI, which might explain the number of STEMI patients observed for whom immediate revascularization procedures were required.25
The results revealed that higher CRP and NT-pro-BNP and lower hemoglobin level at admission and lower GFR were related to outcome. All of these biomarkers are considered established prognostic markers, although none are currently used in risk scores.26
Aggressive treatment of ACS has become widespread, as shown by the PCI rate in our study (67.3%). Six-month mortality was 3.5%, lower that observed in GRACE or in the contemporary MASCARA registry.21 Nevertheless, unlike the present analysis, both registries had a PCI rate lower than 15%, which may explain our lower mortality. Besides, overall evidence-based cardiovascular therapy rates were very high, which has been associated with improvements in outcome.25
The prevalence of general and abdominal obesity was very high in the present analysis (26.9% and 44.6%, respectively), highlighting the obesity epidemic. These results confirm those of studies addressing the impact of obesity on ACS prognosis.3,4,12 It is recognized that abdominal obesity correlates with excessive visceral adiposity, which is associated with several proatherogenic features, including insulin resistance, hypertriglyceridemia, diabetes and hypertension.3 Despite the unquestionable utility of BMI at the population level, it appears to be a poor marker of adiposity-related risk in ACS, and there is currently a debate as to whether an “obesity paradox” exists in ACS.27 The association of adipose tissue with mortality in ACS is complex, and may rely more on the location than on the total amount of adipose tissue.3
In a recent meta-analysis, Coutinho et al. demonstrated that in CAD patients, increasing abdominal obesity (represented by WC or waist-to-hip ratio [WHR]) was associated with high mortality, independently of BMI,3 while Lee et al. found that WHR was an independent predictor of six-month mortality in STEMI patients.11 However, our results did not support the prognostic value of abdominal obesity in ACS. Zeller et al. also concluded that neither BMI nor WC independently predicted mortality after acute MI. However, they observed that patients with high WC but normal BMI (supposedly reflecting the presence of visceral adiposity) had a poorer prognosis.12 Similar results were reported by Kadakia et al.4
We decided to use a combined approach, using the GRACE RS as a prognostic reference. However, our data demonstrated that the GRACE RS had unexpectedly poor predictive accuracy, meaning that it represents a random classification of the risk of event occurrence. Despite its broad acceptance, it should be recognized that the use of the GRACE RS in different populations from its original cohort may compromise its accuracy. Besides, Beygui et al. stated that the discriminatory value of the GRACE RS might be limited in a low-event population.28 Although the GRACE RS has been validated in a Portuguese cohort of NSTEMI patients by De Araújo Gonçalves et al., these authors studied different time points and used a more selected population.22
Most of the GRACE RS variables did not reach statistical significance in multivariate analysis. However, ST-segment deviation was shown to be an independent predictor of outcome. This feature is actually a powerful risk predictor and has been incorporated in several risk scores. Yan et al. found that continuous ST-segment monitoring in NSTEMI patients confers additional prognostic value beyond the GRACE RS.29 However, Fox et al. stated that although the ECG is helpful for guiding treatment, it is unable to predict late complications, and a multivariate approach is therefore needed.2 Nevertheless, almost all the predictive information associated with the GRACE RS in the study population was due to ST changes, which raises doubts concerning the usefulness of the GRACE RS in clinical practice. Moreover, elevated cardiac enzymes had a significant protective prognostic effect. The mechanism behind this relation to outcome cannot be ascertained, since any measurable cardiac troponin is related to an unfavorable prognosis and even minor CK-MB enzyme elevations appear to have prognostic implications.17 Nevertheless, it should be pointed that 90.2% of our study population had elevated cardiac enzymes, and therefore the statistical analysis could have been skewed.
AUC is a commonly used statistic. However, it simply and directly addresses discriminatory ability, a major but not unique component of accuracy. Recent and more refined statistical methods, such as net reclassification improvement and integrated discrimination improvement, have been proposed as better tools for assessment of the additional value of a risk marker.30
Limitations and future perspectivesThe study has several limitations, and consequently its results should be interpreted with caution. Abdominal obesity data were not available for 34% of the cohort. The prognosis of these individuals was poorer (with higher mortality), although their general baseline characteristics did not differ from those of the study population. Severe clinical status might have limited anthropometric measurement in several individuals and therefore a selection bias cannot be excluded.
Second, this was a relatively small retrospective analysis in a single institution, based on nonrandomized data. Accordingly, the negative results obtained could be due to insufficient statistical power, and therefore this issue should be revisited in larger population-based multicenter studies, perhaps with extended follow-up, to assess the delayed prognostic impact of abdominal obesity.
Our results should be considered exploratory and need to be confirmed by future studies.
ConclusionRoutine early risk stratification remains an essential part of ACS care, and is supported by risk scores, such as the GRACE RS. However, risk scores need to be continually re-evaluated, since accurate risk stratification is still a challenge. In this study, abdominal obesity did not improve the discriminatory ability of the GRACE RS, and we can therefore conclude that abdominal obesity assessment does not increase the prognostic information provided by the GRACE RS. However, given the high prevalence of general and abdominal obesity observed in the study population, clarification of obesity-related risk is of major importance and should be reassessed in further research.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.