The aim of the present study was to determine the long-term prognostic value provided by the exercise electrocardiographic (ECG) response to nuclear myocardial perfusion imaging (MPI) in the evaluation of patients with chest pain, focusing on patients with a discrepancy between the two tests.
MethodsA total of 1460 consecutive patients (777 female; 62.6±11.4 years) undergoing exercise myocardial single-photon emission computed tomography (SPECT) were included. The endpoint was the occurrence of acute coronary syndrome, heart failure or cardiac death during follow-up.
ResultsIschemic ECG changes were observed during stress testing in 271 patients (18.5%) and 362 patients (24.7%) had positive (abnormal) exercise MPI results. There was a discrepancy between ECG and SPECT findings in 471 patients (32.2%). During the follow-up period (14.0-39.6 months), 224 patients (15.3%) presented cardiac events. The hazard ratios (HR) of ECG and MPI results to predict events were 1.506 (95% CI: 1.113-2.039) and 10.481 (95% CI: 7.799-14.080), respectively. In patients with negative MPI, the ECG response did not predict events (HR 1.214 [95% CI: 0.646-2.282]), the same as in patients with positive MPI (HR 1.203 [95% CI: 0.848-1.705]). Only in hypertensive patients with positive SPECT did the ECG show significant prognostic value (HR 1.937 [95% CI: 1.030-3.642]). In multivariate analysis, positive MPI proved an independent long-term prognostic factor (HR 10.536 [95% CI: 7.759-14.308]), but not ECG (HR 1.356 [95% CI: 0.994-1.850]).
ConclusionMPI results (normal vs. abnormal) had strong predictive value and discrepant ECG results had no significant additive prognostic value.
O objetivo do presente estudo, foi determinar o valor prognóstico a longo prazo, fornecido pelo eletrocardiograma (ECG) em resposta ao esforço na cintigrafia de perfusão miocárdica (CPM) na avaliação de doentes com dor torácica, com ênfase para os grupos de doentes com discrepância entre os dois testes.
MétodoForam incluídos 1460 doentes consecutivos (777 do sexo feminino; 62,6 ± 11,4 anos), submetidos a exercício na cintigrafia de perfusão miocárdica com SPECT. O endpoint foi a presença de síndrome coronária aguda, insuficiência cardíaca ou morte cardíaca durante o seguimento.
ResultadosDuzentos e setenta e um doentes (18,5%) apresentaram alterações eletrocardiográficas de isquemia durante o teste de esforço e 362 doentes (24,7%) tinham resultados positivos (anormais) na CPM. A discrepância entre os resultados do ECG e CPM apareceu em 471 doentes (32,2%). Durante o período de seguimento (14,0-39,6 meses), 224 (15,3%) apresentaram eventos cardíacos. O hazard ratio (HR) para predizer eventos dos resultados do ECG e CPM foi de 1,506 (1,113-2,039) e 10,481 (7,799-14,080), respetivamente. No grupo de doentes com CPM negativo, o ECG não prediz eventos [HR 1,214 (0,646-2,282)],e o mesmo acontece no grupo de doentes com CPM positivo [HR 1,203 (0,848-1,705)]. Apenas em doentes hipertensos com CPM positivo, o ECG mostrou valor prognóstico significativo [HR 1,937 (1,030-3,642)]. Na análise multivariada, a CPM positiva foi um fator independente de prognóstico a longo prazo [HR 10,536 (7,759-14,308)], mas não o ECG [HR 1,356 (0,994-1,850)].
ConclusãoO resultado da CPM (normal versus anormal) teve um forte valor preditivo e o resultado discrepante no ECG não teve um valor prognóstico adicional significativo.
The application of prognostic testing in patients with known or suspected coronary artery disease (CAD) is based on the premise of risk stratification.1 Ideally, the prognostic utility of a test is to distinguish patients with a high likelihood of future major cardiac events – who may benefit from an invasive strategy – from low-risk patients in whom invasive examination is not recommended.2
The standard test for the initial evaluation of low-risk patients who have a normal baseline electrocardiogram (ECG) is exercise treadmill testing (ETT).3 This remains an inexpensive, safe, and effective exam.4 From the standpoint of clinical management, when clinical cardiologists treat patients with chest pain, they are interested in knowing with high sensitivity and high specificity which patients are at high coronary risk, since cardiac catheterization is not without risks for the patient, as well as economic costs. Myocardial perfusion imaging (MPI) has shown its prognostic value for the prediction of future cardiac events beyond established risk factors and clinical presentation.5 Clinicians sometimes find discrepancies between the ECG (ECG) response in ETT and MPI.6,7 In such cases there may be doubts concerning the strategy to adopt in the management of patients.
The aim of the present study was to determine the prognostic value provided by the exercise ECG response to single-photon emission computed tomography (SPECT) MPI in the evaluation of patients with chest pain, focusing on patients with a discrepancy between the two tests (especially patients with positive ECG response and negative MPI).
2Methods2.1Study populationWe identified 4230 consecutive patients with an intermediate or high likelihood of CAD who underwent SPECT between January 1, 2003 and March 1, 2011. The indication for the test was the presence of ischemic equivalent, consisting of symptoms or ECG findings consistent with CAD. Patients with previous myocardial infarction or revascularization were considered to have known CAD and were excluded from this study, as were patients with valvular heart disease or primary cardiomyopathy. Patients with a non-diagnostic ECG but with underlying ECG abnormalities, including left bundle branch block, and those with pacemakers were also excluded, as were patients unable to exercise. Of the remaining patients (1520), 60 (3.9%) were lost to follow-up. The study conformed to the ethical standards of the Declaration of Helsinki.
2.2Perfusion myocardial images and ECG responseSubjects underwent technetium (Tc)-99m sestamibi rest-stress gated SPECT MPI with either a 1- or 2-day protocol. All patients performed a symptom-limited treadmill exercise test using standard protocols. During exercise, 12-lead ECG recording was performed at each minute of stress with continuous monitoring. At near maximal exercise, a weight-adjusted dose of Tc-99m sestamibi was injected and exercise continued for 1 min after injection. Tc-99m sestamibi SPECT imaging was begun 30 min after isotope injection. SPECT MPI was performed using an elliptical 180° acquisition for 64 projections at 20 s per projection. No attenuation or scatter correction was used. After filtered back-projection, short-axis, vertical, and horizontal long-axis tomograms were generated. SPECT data were analyzed by two imaging cardiologists with regard to the presence of reversible and/or fixed perfusion defects in short-axis and horizontal and vertical long-axis slices, as well as on polar maps, with a commercially available quantitative gated and perfusion SPECT software package, which also enabled assessment of left ventricular ejection fraction (LVEF). In addition, MPI scans were assessed semiquantitatively by segmental visual interpretation, using short-axis and vertical long-axis tomograms divided into 20 segments. Each segment was scored by consensus of two experienced observers using a five-point scoring system (0 = normal, 1 = equivocal, 2 = moderate, 3 = severe reduction of tracer uptake, and 4 = absence of detectable uptake). A summed stress score (SSS) was obtained by adding the scores of the 20 segments of the stress sestamibi images; SSS <3 was considered normal.
2.3DefinitionsCigarette smoking was defined as active smoking in the last six months. Diabetes was defined as increased fasting plasma glucose of ≥126 mg/dl, HbA1c of ≥6.5%, or undergoing treatment with insulin or hypoglycemic agents. Hypertension was defined as systolic/diastolic blood pressure >140/90 mmHg or current use of any antihypertensive medication. Dyslipidemia was defined as total cholesterol ≥220 mg/dl, triglycerides ≥150 mg/dl, high-density lipoprotein (HDL) cholesterol <40 mg/dl, or current use of lipid-lowering drugs. These four variables (cigarette smoking, diabetes, hypertension and dyslipidemia) were considered as cardiovascular risk factors, together with the presence of previous myocardial infarction or of peripheral arterial disease. Age >45 years (males) or >55 years (females) was also considered a cardiovascular risk factor. An ECG stress test was considered positive if there was a horizontal or downsloping ST-segment depression of ≥0.1 mV at 0.08 s after the J-point.
2.4Follow-upEvents were defined as cardiac death (confirmed by review of death certificate, hospital chart, or physician's records), non-fatal myocardial infarction (documented by appropriate cardiac enzyme and electrocardiographic changes), revascularization or admission due to new-onset heart failure. Events at one year and during follow-up were analyzed. The median follow-up was 16.8 months (interquartile range: 14.0-39.6 months).
2.5Statistical analysisThe statistical analyses were performed with SPSS (Statistical Package for the Social Sciences), version 17.0. Categorical or dichotomous variables are expressed as absolute values and percentages, and were compared with Pearson's chi-square test. Continuous variables with normal distribution are expressed as mean ± standard deviation, and the Student's t test was used for comparisons between groups. Continuous data from more than two groups were compared with ANOVA. A binomial logistic regression model was used to evaluate the independent contribution of ECG response and MPI to the risk of events at one year. Age in years, number of cardiovascular risk factors, LVEF as a continuous variable, ECG response and MPI results were included in the model in backward stepwise analysis. C statistics, as a measure of discriminative power, were calculated for predicting cardiac events in the first year after the test. A Cox proportional hazard analysis was carried out to assess the independent role of both tests (ECG and SPECT) for predicting mortality during follow-up using the same variables as in the binomial logistic regression. Adjusted odds and hazard ratios and 95% confidence intervals (CI) were presented. Kaplan-Meier curves were constructed to evaluate prognosis during follow-up of different groups based on ECG response and MPI results, and the results were analyzed using the log-rank test. Receiver operating characteristic (ROC) curve analysis was performed to establish the diagnostic value of both tests (ECG and SPECT) to predict events. A p value <0.05 was considered statistically significant.
3Results3.1Baseline characteristicsA total of 1460 patients (777 female; mean age 62.6±11.4 years) were included in the study. Table 1 shows their baseline clinical characteristics. Ischemic ECG changes were observed during stress testing in 271 patients (18.5%) and 362 patients (24.7%) had positive MPI results (Table 2).
Baseline characteristics of the overall population and of different groups according to SPECT and ECG results.
| Variables | Total | SPECT −, ECG − | SPECT −, ECG + | SPECT +, ECG − | SPECT +, ECG + | p |
| Age (years) | 62.6±11.4 | 62.8±11.3 | 63.0±12.0 | 61.9±11.3 | 62.2±12.3 | 0.638 |
| Female (%) | 53.2 | 53.5 | 54.2 | 51.2 | 54.3 | 0.899 |
| Current smoking (%) | 13.0 | 13.0 | 15.3 | 12.5 | 9.9 | 0.652 |
| Hypertension (%) | 66.1 | 65.0 | 64.7 | 68.0 | 75.3 | 0.243 |
| Dyslipidemia (%) | 58.9 | 59.7 | 57.4 | 58.4 | 55.6 | 0.843 |
| Diabetes (%) | 24.2 | 26.0 | 20.0 | 21.7 | 23.5 | 0.223 |
| Peripheral arterial disease (%) | 3.2 | 3.1 | 4.7 | 2.8 | 1.2 | 0.451 |
| Atrial fibrillation (%) | 6.2 | 5.1 | 6.8 | 8.2 | 11.1 | 0.061 |
| LVEF (%) | 61.0±11.9 | 60.9±11.5 | 60.9±13.4 | 61.1±12.1 | 62.3±12.3 | 0.797 |
| Energy cost (METs) | 8.7±3.1 | 8.7±3.1 | 8.4±3.0 | 8.6±3.2 | 9.2±3.0 | 0.361 |
| Events at six months (%) | 8.7 | 2.3 | 4.2 | 25.3 | 33.3 | 0.001 |
| Events during follow-up (%) | 15.3 | 5.4 | 6.3 | 43.3 | 54.3 | 0.001 |
−: negative; +: positive; ECG: electrocardiographic result; LVEF: left ventricular ejection fraction; METs: metabolic equivalents; SPECT: single-photon emission computed tomography result.
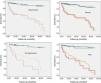
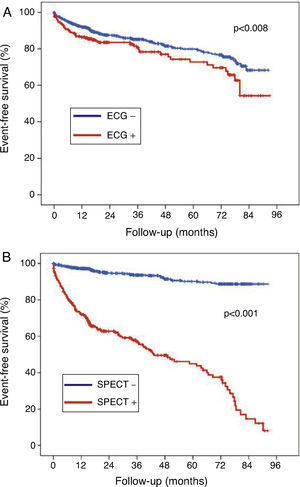
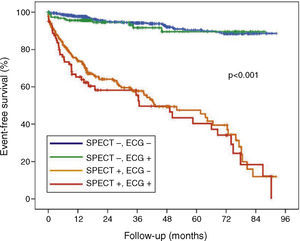
During the follow-up period (1-92 months), 224 (15.3%) of the total population presented cardiac events. Compared to patients who were still alive at the end of follow-up, those who died had a higher incidence of positive ECG response and positive MPI results (Table 3). There were no statistically significant differences between groups (with and without events) in terms of other variables (age and gender, cardiovascular risk factors and LVEF). The hazard ratios (HR) of ECG changes and MPI results to predict events were 1.506 (95% CI: 1.113-2.039, p=0.008) and 10.481 (95% CI: 7.799-14.080, p=0.001), respectively (Figure 1). For comparison of different groups (based on ECG and MPI results), survival curves were constructed for the four groups (Figure 2). As can be seen, the prognosis of patients with positive MPI was clearly worse than that of patients with negative MPI, independently of ECG changes during stress. In multivariate analysis (Table 4), adjusted for age, gender, number of cardiovascular risk factors and LVEF, MPI proved an independent long-term prognostic factor (HR 10.536, 95% CI: 7.759-14.308; p=0.001), but not ECG changes (HR 1.356, 95% CI: 0.994-1.850; p=0.055).
Baseline characteristics of the study population, stratified by presence of cardiac death and cardiac events.
| Variables | Events | No events | p |
| Age (years) | 62.7±11.3 | 62.6±11.4 | 0.937 |
| Female (%) | 53.2 | 53.6 | 0.909 |
| Current smoking (%) | 13.1 | 12.5 | 0.804 |
| Hypertension (%) | 70.5 | 65.3 | 0.127 |
| Dyslipidemia (%) | 62.5 | 58.3 | 0.235 |
| Diabetes (%) | 25.4 | 24.0 | 0.649 |
| Peripheral arterial disease (%) | 3.6 | 3.1 | 0.695 |
| Atrial fibrillation (%) | 5.8 | 6.3 | 0.357 |
| LVEF (%) | 61.0±12.7 | 61.0±11.9 | 0.987 |
| Energy cost (METs) | 8.6±3.3 | 8.7±3.1 | 0.504 |
| SPECT + (%) | 72.8 | 16.1 | 0.001 |
| ECG + (%) | 25.0 | 17.4 | 0.007 |
+: positive; ECG: electrocardiographic result; LVEF: left ventricular ejection fraction; METs: metabolic equivalents; SPECT: single-photon emission computed tomography result.
Multivariate analysis to predict long-term outcomes.
| VARIABLES | HAZARD RATIO | CI 95% | P value |
| Age | 1.004 | 0.991–1.017 | 0.573 |
| Number of cardiovascular risk factors | 1.167 | 1.027–1.326 | 0.018 |
| Left ventricular ejection fraction | 0.996 | 0.984–1.007 | 0.455 |
| SPECT + | 1.356 | 0.994–1.850 | 0.055 |
| EKG + | 10.536 | 7.759–14.308 | 0.001 |
At one year after testing, 127 (8.7%) of the total population presented events. Patients with ECG changes during exercise testing were at greater risk of events at one year than those without (OR: 1.768, 95% CI: 1.169-2.675; p=0.007), as were patients with positive SPECT (OR 13.684, 95% CI: 8.851-21.155; p=0.001). The area under the curve (AUC) for MPI results to predict events at one year (0.787: 95% CI: 0.743-0.831) was significantly larger than for ECG changes (0.549: 95% CI: 0.495-0.604) (p=0.002). The combined model of ECG changes and MPI results increased the AUC for the prediction of events to 0.802 (95% CI: 0.760-0.844), without reaching statistical significance compared to the AUC for MPI results (p=0.691). In multivariate analysis (Table 5), adjusted for age, gender, number of cardiovascular risk factors and LVEF, both ECG changes and MPI results proved independent predictors of 1-year outcomes (OR 1.737, 95% CI: 1.091-2.767; p=0.020 for ECG changes, and OR 13.670, 95% CI: 8.691-21.503; p=0.001 for MPI result). The C statistic of the model was 0.811.
Multivariate analysis to predict events in the first year.
| VARIABLES | ODDS RATIO | CI 95% | P value |
| Age (years) | 0.997 | 0.977–1.017 | 0.794 |
| Number of cardiovascular risk factors | 1.192 | 0.987–1.440 | 0.069 |
| Left ventricular ejection fraction | 0.997 | 0.980–1.013 | 0.699 |
| SPECT + | 1.737 | 1.091–2.767 | 0.020 |
| EKG + | 13.670 | 8.691–21.503 | 0.001 |
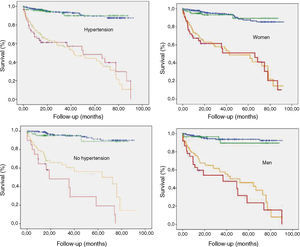
Normal MPI with a positive ECG in the exercise test was observed in 190 patients (13.0%) and the opposite (positive MPI and negative ECG) in 281 patients (19.2%). No statistically significant differences were found between the clinical characteristics of either of these groups compared to the rest of the study population. Figure 3 shows the survival curves in the discrepant groups adjusted by gender and hypertension. Of the 1098 patients (75.2%) with negative SPECT, the presence of ECG changes during stress testing was not associated with more events at one year (OR 1.857, 95% CI: 0.810-4.257; p=0.244) or more events throughout the follow-up period (HR 1.214, 95% CI: 0.646-2.282; p=0.547). The same was true for the 362 patients (24.8%) with positive SPECT (OR for events at one year 1.479, 95% CI: 0.866-2.524, p=0.151, and HR for follow-up events 1.203, 95% CI: 0.848-1.705; p=0.307). However, in the latter group (positive MPI) we found that non-hypertensive patients (n=110) with ischemic ECG changes during stress testing (n=20) had a worse prognosis (percentage of events 70% vs. 37.8% in hypertensive patients with positive MPI and ischemic ECG changes) (HR for positive ECG response 1.937, 95% CI: 1.030-3.642, p=0.009).
In addition we focused on patients with negative MPI and positive ECG. In this subgroup, 11 (6.3%, 0.75% of the total study population) had cardiac events during follow-up. Of these, seven were undergoing cardiac catheterization, and multivessel disease was detected in all except one (who had proximal left anterior descending disease). In these patients, the ECG response was markedly positive (widespread ST depression ≥2 mm).
4DiscussionThe most striking result of our study is the low prognostic value added by the ECG response to that of MPI in patients with chest pain undergoing exercise stress testing. MPI results (normal vs. abnormal) had strong predictive value, but discrepant ECG results had no significant additive prognostic value (HR 10.4 vs. 1.5). Besides the general implications of this result, particular consideration should be given to two particular groups: firstly patients with multivessel CAD, in whom MPI results may be misleadingly balanced, and in whom the ECG response is often overly positive (widespread ST-segment depression >2 mm); and secondly non-hypertensive patients, in whom, even if they had a positive response on MPI, a positive ECG response suggests a worse prognosis.
Significant perfusion abnormalities result in myocardial ischemia that affects the ST segment on the ECG tracing, evaluated during stress testing (exercise or pharmacological stress with dipyridamole, adenosine, or dobutamine).6,7 Abnormal ECG findings may result from ischemia, but they may also reflect other factors (leading to false positive results), particularly in women and patients with hypertension8–12. In our study we found no differences in the percentage of positive ECG responses according to gender and hypertension, unlike other studies, despite the high percentage of female (>50%) and hypertensive (>65%) patients.
The prognostic value of the ECG response to exercise and MPI has been evaluated in multiple independent studies.13,14 By the 1990s SPECT imaging was considered to have superior value compared to ECG, associated with a minimal mortality risk of <1% per year.15–17 However, in 2003 Abbott et al.7 and Klodas et al.18 questioned this belief, showing a significant risk of a cardiac event (with a yearly risk of death or myocardial infarction of 5-10%) in patients with no perfusion abnormalities on SPECT but with “ischemic ST depression” during dipyridamole or adenosine stress testing. They explained these results on the basis of multivessel CAD that resulted in true positive ECG findings and false negative perfusion imaging with SPECT. One year later, Candell et al.19 retrospectively analyzed 33 patients (of 7350 myocardial perfusion SPECT studies) who had normal scintigraphic findings with a positive ECG in the exercise test and coronary angiography. Twenty-one of the 26 women (81%) and one of the seven men (14%) had normal coronary angiographic findings (p=0.004). Seven out of 11 patients with CAD had left main coronary artery or multivessel disease. The authors concluded that the “normal SPECT with positive ECG” pattern is infrequent, and is observed predominantly in women with normal coronary angiographic findings. Later, Hage et al.20 confirmed the superior prognostic value of SPECT over ECG: with normal (true negative) SPECT findings, the presence of concomitant ischemic (false positive) ST changes on the ECG does not have an adverse effect on prognosis. They presented the results of 73 patients with ischemic ST depression but without perfusion abnormalities detected by SPECT during adenosine stress, followed for five years. The cardiac mortality in this group of patients was less than 1.3%.
We focused on patients with chest pain and discrepancies between the two tests: positive SPECT MPI with a negative ECG response and vice versa, negative MPI with a positive ECG response. We found no differences in baseline characteristics of patients in the different groups. In patients with negative SPECT the event rate was very low, regardless of the ECG response. There was a small proportion of patients (<1%) with negative MPI and multivessel CAD in whom the ECG response was very positive. Although the literature reports an overall sensitivity of SPECT MPI for detecting multivessel disease ranging from 80% to 95%,21 in cases with evenly distributed ischemia without inducible flow heterogeneity among the different vessel territories, balanced ischemia has been hypothesised to explain lack of perfusion defects.5 By its nature, SPECT only allows detection of relative perfusion defects. Therefore, the true extent of myocardial ischemia may be underestimated, particularly in vascular territories adjacent to areas with more severe coronary stenosis. It may be necessary to specify different degrees of positivity or the time of normalization of ECG response in order to determine that a negative result of ischemia by nuclear MPI is not a false positive.
In addition, Ghadri et al.22 recently showed that in patients with normal SPECT MPI, a coronary artery calcium score (AAC) >1000 confers high added diagnostic value for detecting CAD, predominantly in patients with one- and two-vessel disease, and state that this is not based solely on unmasking balanced ischemia due to three-vessel disease. According to the authors, balanced ischemia may not be solely due to balanced epicardial coronary lesion severity, but could also be caused by microcirculatory dysfunction in which global hyperemic myocardial flow response and myocardial flow reserve are blunted. A massive increase in CAC would – although measured in the epicardial vessel – then reflect involvement of the coronary microcirculatory tree, potentially associated with a decrease in myocardial flow reserve, favoring a balanced hyperemic response due to blunted flow heterogeneity.
On the other hand patients with positive MPI have a poorer prognosis, independently of ECG response. Special mention should be made of non-hypertensive patients, in whom the ECG result cannot be distorted by signs of left ventricular hypertrophy with systolic overload. In these patients (positive MPI) the ECG response identifies a subgroup of patients with very high risk of cardiac events (more than two-thirds).
5ConclusionsThis study addresses a frequent clinical dilemma: what to do with discrepant ECG and MPI findings? After analyzing the prognostic value of MPI and ECG response to exercise testing in 1460 consecutive patients with intermediate or high likelihood of CAD, we concluded that when the results of MPI and ECG are discordant, it is correct to consider only the MPI results.
6Ethical disclosures6.1Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
6.2Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
6.3Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
7Conflicts of interestThe authors have no conflicts of interest to declare.