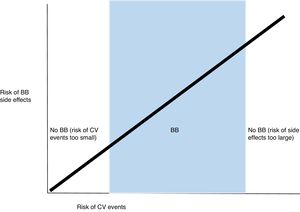
We would like to thank Fernando Montenegro Sá and João Morais for their interest in our paper.1 Beta-blockers are indicated after ST-segment elevation myocardial infarction (STEMI) in patients with left ventricular ejection fraction (LVEF) ≤40% (class I recommendation, level of evidence A) but in those with LVEF >40% the benefit is not clear (class IIa, level B).2 We agree that in patients in the 40-50% range beta-blockers appear more likely to help than to harm, due to their moderate probability of future events. The gradient of benefit means that beta-blockers should probably not be used in very low risk STEMI,3,4 in which the risk of cardiovascular events is extremely small in the near future. In addition, beta-blockers should be avoided in high-risk patients in whom side effects will probably occur, as in those with hypotension, acute heart failure,5 or shock6 (Figure 1).
Further studies are needed to better identify STEMI patients who might benefit from beta-blockers, taking into consideration not only LVEF, but also other factors associated with prognosis that might improve with this treatment. For instance, endothelial dysfunction is common in STEMI7 and beta-blockers improve microvascular function.8 This is also the case with atrial fibrillation.9,10 Most studies of beta-blockers in STEMI were performed in an era when the rate of primary angioplasty was low and heart failure and mechanical complications were frequently seen.11 The current scenario is different and extrapolation of previous data could lead to overuse of these drugs. In the Description of Acute Myocardial Infarction: Management, New Therapies and Evolution (DIAMANTE) registry, 86% of our patients received beta-blockers.1 Finally, regarding dosage, Mars et al.12 have recently shown that target dose is not associated with cardiovascular outcomes, and Goldberger et al.13 even suggest that patients treated with 12.5-25% of the target dose may have enhanced survival compared with other doses.
Conflicts of interestThe authors have no conflicts of interest to declare.