Non-dipper and extreme dipper blood pressure (BP) profiles are associated with a worse cardiovascular prognosis. The relationship between nocturnal BP profile and hypertensive retinopathy (HR) is not fully established.
AimTo assess the association between the prevalence and severity of HR and nocturnal BP.
MethodsWe prospectively studied hypertensive patients who underwent 24-hour ambulatory BP monitoring. The population was divided into two groups according to the presence or absence of lesions and compared according to baseline characteristics, nocturnal BP profile (dippers, non-dippers, inverted dippers/risers and extreme dippers) and mean nocturnal systolic (SBP) and diastolic (DBP) BP values. The presence and severity of HR were assessed using the Scheie classification. The relationship between nocturnal SBP and DBP values (and nocturnal BP profile) and the prevalence and severity of HR was determined.
ResultsForty-six patients (46% male, aged 63±12 years) were analyzed, of whom 91% (n=42) were under antihypertensive treatment. Seventy percent (n=33) had uncontrolled BP. HR was diagnosed in 83% (n=38). Patients with HR had higher mean systolic nocturnal BP (151±23 vs. 130±13 mmHg, p=0.008). Patients with greater HR severity (Scheie stage ≥2) had higher nocturnal BP (153±25 vs. 140±16 mmHg, p=0.04). There was no statistically significant association between DBP and nocturnal BP patterns and HR.
ConclusionsThe prevalence and severity of HR were associated with higher nocturnal SBP. No relationship was observed between nocturnal BP profile and the presence of HR.
Os perfis tensionais noturnos non-dipper e extreme-dipper têm sido associados a lesões de órgão-alvo. A relação entre a pressão arterial (PA) e retinopatia hipertensiva (RH) está pouco esclarecida.
ObjetivoAvaliar em doentes (dts) hipertensos a relação entre os valores noturnos de pressurometria em ambulatório de 24 h (MAPA) e prevalência e a gravidade da RH.
MétodosForam avaliados prospectivamente dts hipertensos submetidos à realização de MAPA de 24 h. Foram determinadas características basais, PA sistólica (PAS) e diastólica (PAD) médias noturnas, e os dts classificados pelo perfil tensional noturno em dipper; non-dipper; inverted-dipper e extreme-dipper. O diagnóstico de RH foi estabelecido por fundoscopia e a gravidade definida pela classificação de Scheie. Foi estabelecida a relação entre valores de PAS e PAD noturnos e o perfil tensional noturno com a prevalência e gravidade da RH.
ResultadosForam avaliados 46 dts (46% sexo masculino [n=21]; idade média 63±12 anos). Noventa e um por cento dos dts estavam sob terapêutica anti-hipertensora (n=42); destes, 30% apresentavam PA controlada (n=13). A presença de RH foi observada em 83% dos dts (n=38). Os dts com RH apresentaram níveis de PAS noturna mais elevados (151±23 versus 130±13, p=0,008). A PAS noturna esteve ainda associada a uma maior gravidade de RH (153±25 versus 140±16, p=0,04). Não existiu relação entre a PAD noturna ou o perfil tensional noturno e presença de RH.
ConclusãoNíveis mais elevados de PAS noturna estiveram associados a RH. Não se verificou relação entre o perfil tensional noturno e a presença de RH.
Hypertension is a common disease, with a prevalence in the general population of 30-45% and a significant burden of morbidity and mortality.1
Various studies have demonstrated a better correlation between 24-hour ambulatory blood pressure monitoring (ABPM) values and the degree of target organ damage and overall cardiovascular prognosis compared to casual blood pressure (BP) values.2
According to various studies, the non-dipper profile is associated with more target organ damage, particularly left ventricular (LV) hypertrophy, microalbuminuria and kidney injury, and sleep disorders, as well as a worse cardiovascular prognosis and higher risk for cardiac and cerebrovascular events.2–6 The extreme dipper profile has also been shown to have an important impact on cardiovascular prognosis.2
Hypertensive retinopathy (HR) is the main ocular manifestation of hypertension, 50-80% of hypertensive individuals developing abnormalities in retinal microvasculature.8 The signs of HR are important indicators of risk for cardiovascular morbidity and mortality7 and according to some authors, retinal assessment is crucial for stratifying vascular risk in hypertension.7
The relationship between circadian BP variation and the prevalence and severity of HR is not fully established. According to some studies, HR is more frequent and more severe in non-dipper patients.3
In this study we aimed to analyze the relationship between nocturnal values from 24-hour ABPM and the prevalence and severity of HR in hypertensive patients.
MethodsPopulation and sampleThe population consisted of hypertensive patients who underwent ABPM between January and December 2013. Patients were invited by telephone to undergo fundoscopy at the hospital with the aim of identifying target organ damage. Of a total of 355 patients, only 46 agreed to undergo the test, and these constitute the study sample; the remainder refused or could not be contacted by telephone.
Study variablesThe sample was characterized according to demographic (age and gender), clinical (personal history, comorbidities and cardiovascular risk factors, and duration and control of hypertension), laboratory (serum creatinine), and echocardiographic (concentric LV hypertrophy) variables, and treatment (antihypertensive drug class). These variables were assessed through a questionnaire given to the patients (Appendix A) and by reviewing electronic medical records.
To assess patients’ BP profile, their nocturnal and daytime systolic (SBP) and diastolic (DBP) BP were measured, and on the basis of nocturnal BP profile, patients were classified as dippers (mean BP fall >10% and <20%), non-dippers (mean BP fall <10%), inverted dippers (mean BP fall <0%) and extreme dippers (mean BP fall >20%).
Diagnosis of hypertensive retinopathyThe diagnosis of HR was established by fundoscopy and its severity graded using the Scheie classification, which grades hypertensive lesions (stages 1-4) and arteriolosclerotic changes (grade 0-4) (Table 1).
Scheie classification of hypertensive retinopathy.
| Stage | Alterations on fundoscopy |
|---|---|
| 0 | Diagnosis of hypertension but no visible retinal abnormalities |
| 1 | Diffuse arteriolar narrowing; no focal constriction |
| 2 | More pronounced arteriolar narrowing with focal constriction |
| 3 | Focal and diffuse narrowing, with retinal hemorrhage |
| 4 | Retinal edema, hard exudates, optic disc edema |
IBM SPSS Statistics version 20 for Windows 8 was used for the statistical analysis. Continuous variables were expressed as mean ± standard deviation and compared with the Student's t test. Categorical variables were expressed as absolute value and/or percentage and were compared with the chi-square test. Associations were considered to be statistically significant with a p-value <0.05.
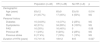
ResultsThe study population consisted of 46 patients, 46% of them male (n=21), with a mean age of 63±12 years. The demographic, clinical and laboratory characteristics of the sample according to presence of HR are presented in Table 2.
Baseline characteristics of the study population.
| Population (n=46) | HR (n=38) | No HR (n=8) | p | |
|---|---|---|---|---|
| Demographic | ||||
| Age (years) | 63±12 | 65±9 | 53±18 | 0.014 |
| Male | 21 (45.7%) | 17 (45%) | 4 (50%) | NS |
| Personal history | ||||
| Diabetes | 16 (34.8%) | 14 (37%) | 2 (25%) | NS |
| Dyslipidemia | 42 (91%) | 34 (89%) | 8 (100%) | NS |
| PAD | 16 (35%) | 16 (40%) | 0 | 0.06 |
| Previous MI | 11 (24%) | 9 (24%) | 2 (25%) | NS |
| Previous stroke | 8 (17.4%) | 7 (18%) | 1 (13%) | NS |
| Duration of HTN (years) | 15.7±11.6 | 18±12 | 6±5 | 0.027 |
HR: hypertensive retinopathy; HTN: hypertension; MI: myocardial infarction; PAD: peripheral arterial disease.
Among comorbidities and risk factors, dyslipidemia and diabetes were the most frequent, found in 91% and 35% of the patients, respectively. Mean creatinine levels were 1.07±07 mg/dl in the total population and 1.12±07 mg/dl in patients with HR. A total of 53% of the patients met echocardiographic criteria for LVH (Table 2).
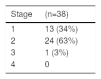
HR was found in 83% of the patients, of whom 64% were in stage 2 or higher of the Scheie classification (Table 3).
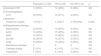
A total of 42 patients (91%) were receiving antihypertensive therapy, of which the most common pharmacological classes were beta-blockers, used in 50% of the patients, and diuretics in 44%, followed by angiotensin-converting enzyme inhibitors, angiotensin receptor blockers and calcium channel blockers (39% each). In 30% of the patients this treatment resulted in controlled BP (Table 4).
Baseline characteristics and antihypertensive therapy according to the presence of hypertensive retinopathy.
| Population (n=46) | HR (n=38) | No HR (n=8) | p | |
|---|---|---|---|---|
| Controlled HTN | 13 (30%) | 10 (26%) | 3 (38%) | NS |
| Echocardiographic | ||||
| LVH | 20 (53%) | 18 (47%) | 2 (25%) | NS |
| Laboratory | ||||
| Creatinine (mg/dl) | 1.07±0.7 | 1.12±0.7 | 0.75±0.053 | 0.005 |
| Antihypertensive therapy | ||||
| Beta-blocker | 23 (50%) | 19 (50%) | 4 (50%) | NS |
| ACEI | 18 (39%) | 15 (39%) | 3 (38%) | NS |
| ARB | 18 (39%) | 16 (42%) | 2 (25%) | NS |
| Diuretic | 20 (44%) | 18 (47%) | 2 (25%) | NS |
| CCB | 18 (39%) | 16 (42%) | 2 (25%) | NS |
| Aldosterone blocker | 0 | 0 | 0 | NS |
| Centrally acting | 5 (11%) | 4 (11%) | 1 (13%) | NS |
| Vasodilator | 7 (15%) | 5 (13%) | 2 (25%) | NS |
ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; CCB: calcium channel blocker; HR: hypertensive retinopathy; HTN: hypertension; LVH: left ventricular hypertrophy.
A non-dipper profile was found in 37% of the patients, dipper in 48%, extreme dipper in 7% and inverted dipper in 9%. Mean nocturnal SBP and DBP were 148±23 mmHg and 66±9 mmHg, respectively (Table 5).
Presence of hypertensive retinopathy according to nocturnal blood pressure profile and daytime/nocturnal blood pressure variations.
| Population (n=46) | HR (n=38) | No HR (n=8) | p | Non-severe HR (n=13) | Severe HR (n=25) | p | |
|---|---|---|---|---|---|---|---|
| Dipper | 22 (48%) | 18 (47%) | 4 (50%) | NS | 6 (46%) | 12 (48%) | NS |
| Extreme dipper | 3 (7%) | 3 (8%) | 0 | NS | 1 (8%) | 2 (8%) | NS |
| Inverted dipper | 4 (9%) | 2 (5%) | 2 (25%) | NS | 2 (15%) | 0 | NS |
| Non-dipper | 17 (37%) | 15 (39%) | 2 (25%) | NS | 4 (31%) | 11 (44%) | NS |
| Nocturnal SBP (mmHg) | 148±23 | 151±23 | 130±13 | 0.008 | 140±16 | 153±25 | 0.04 |
| Nocturnal DBP (mmHg) | 66±9 | 66±9 | 64±7 | NS | 65.6±10 | 66±7.2 | NS |
| Daytime SBP (mmHg) | 138±13.4 | 139±14 | 129±8 | 0.021 | 135±11 | 140±15 | NS |
| Daytime DBP (mmHg) | 76±9 | 76±10 | 72±4 | NS | 76±7 | 75.4±11 | NS |
DBP: diastolic blood pressure; HR: hypertensive retinopathy; SBP: systolic blood pressure; Severe HR: stage ≥2 on the Scheie classification.
The prevalence of HR in our population was high (83%), which is in agreement with the literature, given that 50-80% of hypertensive patients develop abnormalities in retinal microvasculature.8
Older age (65±9 years) and longer duration of hypertension (18±12 years) were associated with a statistically significant higher risk of HR, but gender and personal history were not.
In theory, patients with treated and controlled hypertension are at less risk of target organ damage, or at least their clinical course should be slower and more progressive, but this was not the case in our population. Only 38% of patients with controlled hypertension did not present any microvascular damage (uncontrolled hypertension: 85% [n=28] with HR vs. 15% [n=5] without HR, p=NS; controlled hypertension: 77% [n=10] with HR vs. 23% [n=3] without HR, p=NS).
High mean creatinine levels were associated with the presence of HR, but LVH was not. According to the literature, organ damage associated with hypertension is more common and occurs earlier in the heart (LVH, diastolic dysfunction) than in the retina and kidneys. It is possible that the small sample size was the reason an association between LVH and HR could not be established.9
There was no statistical association between presence of HR and class of antihypertensive drug.
According to various studies, the non-dipper and extreme dipper profiles are associated with more target organ damage and have a significant cardiovascular impact. There are few studies on retinal damage and BP profile, but these lesions are more frequent and more severe in non-dipper patients.2–6
No nocturnal blood pressure profile was associated with higher risk of HR; although the prevalence of dipper and non-dipper profiles among patients with HR was high (47% and 39% respectively), this did not reach statistical significance.
On the other hand, high nocturnal and daytime SBP values (nocturnal SBP: 151±23 mmHg with HR vs. 130±13 mmHg without HR, p=0.008; daytime SBP: 139±14 mmHg with HR vs. 129±8 mmHg without HR, p=0.021) were associated with the presence of HR. More severe HR was observed at high nocturnal SBP levels (nocturnal SBP 153±25 mmHg: HR stage ≥2, vs. 140±16 mmHg: non-severe HR, p=0.04). In patients with hypertension, SBP was more closely associated than DBP with a negative impact on the retinal microvasculature. Observational studies have demonstrated that SBP is an important and independent predictor of risk for cardiovascular and kidney disease.10
LimitationsThe small sample size is one of the study's main limitations.
ConclusionHR was highly prevalent in the study sample and was associated with older age and longer duration of hypertension.
No relationship was found between nocturnal BP profile and presence or severity of HR. Higher nocturnal SBP was associated with greater prevalence and severity of HR. Although the sample was small, SBP was associated with a greater risk of microvascular damage in the retina compared with DBP.
In view of the high prevalence of retinopathy in the hypertensive population, and given the negative cardiovascular impact of HR demonstrated in various studies, retinal assessment should be part of the physical examination of a hypertensive patient, and treatment should be specifically targeted to correct SBP.
Nonetheless, further studies with larger populations are needed to elucidate the relationship between BP profile and HR, as well as to enable more precise treatment options.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Duarte T, Gonçalves S, Brito R, et al. Relação entre o perfil tensional noturno e a prevalência e gravidade da retinopatia hipertensiva. Rev Port Cardiol. 2018;37:169–173.