We aimed to study the psychosocial adjustment (PSA), psychiatric morbidity and quality of life of adolescents and young adults with congenital heart disease (CHD) to determine which demographic and clinical variables negatively affect adjustment and which increase resilience.
MethodsThe study included 74 patients with CHD, 41 male and 33 female, aged between 12 and 26 years (mean 18.76±3.86). Demographic information and a complete clinical history were obtained. The participants were interviewed regarding social support, family environment, self-image and physical limitations. A standardized psychiatric interview was conducted, and self-report questionnaires were administered for assessment of PSA (Youth Self Report and Adult Self Report) and quality of life (World Health Organization Quality of Life – Short Version). A caregiver completed an observational version of the PSA questionnaire (Child Behavior Checklist or Adult Behavior Checklist).
ResultsFemale participants showed more feelings of anxiety and depression (U=952.500; p=0.003), thought problems (U=929.500; p=0.005) and aggressive behavior (U=999.000; p=0.000). They also showed a higher rate of psychopathology. Patients with complex forms of CHD reported more thought problems (U=442.000; p=0.027) and internalization (U=429.000; p=0.021). Compared to the Portuguese population as a whole, participants showed better quality of life in the domains of social relationships (t=2.333; p=0.022) and environment (t=3.754; p=0.000). Patients who had undergone surgery had worse quality of life in physical terms (t=−1.989; p=0.050), social relationships (t=−2.012; p=0.048) and general quality of life (U=563.000; p=0.037), compared to those who were not operated. Better social support was associated with better quality of life in physical terms (t=3.287; p=0.002) and social relationships (t=3.669; p=0.000). Better school performance was also associated with better overall quality of life (U=457.000; p=0.046), less withdrawn behavior (U=812.500; p=0.031), fewer feelings of anxiety and depression (U=854.000; p=0.009), fewer attention problems (U=903.500; p=0.001), and lower scores for internalization (U=817.000; p=0.029) and externalization (U=803.500; p=0.042). Physical limitations had a detrimental effect on quality of life (U=947.500; p=0.001).
DiscussionFemale participants were more prone to worse psychological adjustment and to psychopathology. Patients with complex forms of CHD showed worse PSA, as they need regular care, which restricts social contact with peers and family and integration in school and leisure activities. Patients who had undergone surgery showed worse quality of life as they often have long hospital stays, during which social activities are restricted, making it more difficult for them to develop a good social support network. They require close medical care, and the restrictions on their activities may be life-limiting. Their sense of survival may also be threatened.
ConclusionsPatients with CHD appear to be more prone to psychopathology and female patients are more likely to show worse PSA. Social support was shown to play a crucial role in buffering stress and promoting patients’ adjustment.
Caracterizar a população de adolescentes e jovens adultos com cardiopatias congénitas (CC) ao nível do seu ajustamento psicossocial e morbilidade psiquiátrica, bem como avaliar a qualidade de vida (QV), para perceber quais são as variáveis com impacto na vida e na adaptação à doença.
População e métodosParticiparam 74 pacientes com CC, sendo 41 do sexo masculino e 33 do sexo feminino, com idades entre 12-26 (média = 18,76 ± 3,86). Foram recolhidos os dados demográficos e clínicos mais relevantes dos pacientes e foi aplicado um conjunto de instrumentos, incluindo uma entrevista semiestruturada sobre tópicos de suporte social, estilo de educação na família, autoimagem e limitações físicas, uma entrevista psiquiátrica estandardizada e questionários para avaliar o ajustamento psicossocial na forma de autorrelato (YSR e ASR) e relato dos cuidadores (CBCL e ABCL), bem como um questionário de avaliação da qualidade de vida (WHOQOL-BREF).
ResultadosO sexo feminino relatou mais ansiedade/depressão (u = 952,500; p = 0,003), alterações do pensamento (u = 929,500; p = 0,005) e comportamento agressivo (u = 999,000; p = 0,000). Pacientes com CC complexas relataram mais alterações de pensamento (u = 442,000; p = 0,027) e internalização (u = 429,000; p = 0,021). Comparativamente com a população portuguesa, os nossos participantes apresentaram melhor QV nos domínios relações sociais (t = 2,333; p = 0,022) e ambiente (t = 3,754; p = 0,000). Os pacientes que não foram submetidos a intervenções cirúrgicas revelaram melhor QV nos domínios físico (t = −1,989; p = 0,050), de relações sociais (t = −2,012; p = 0,048) e QV geral (u = 563,000; p = 0,037). A presença de um melhor suporte social está relacionada com uma melhor QV nos pacientes em todos os domínios avaliados, com destaque para o físico (t = 3,287; p = 0,002) e relações sociais (t = 3,669; p = 0,000). Um melhor desempenho académico encontrava-se também associado com uma melhor perceção de QV global (u = 457 000; p = 0,046), com menos tendência ao isolamento (u = 812.500; p = 0,031), menos sentimentos de ansiedade e de depressão (u = 854 000; p = 0,009), menos problemas de atenção (u = 903 500; p = 0,001), e valores mais baixos de internalização (u = 817 000; p = 0,029) e de externalização (u = 803 500; p = 0,042). As limitações físicas tinham um efeito nocivo no QV (u = 947 500; p = 0,001).
DiscussãoAs participantes do sexo feminino evidenciaram pior ajustamento psicossocial e maior propensão à psicopatologia. As CC complexas exigem mais cuidados regulares, limitando o contacto social com pares, a integração escolar e de lazer, e dificultando a adaptação. A realização de cirurgias influencia a QV dos pacientes, pela exigência de mais cuidados médicos, induzindo maiores limitações na sua vida diária, o que dificulta a aquisição de uma rede de suporte social satisfatória.
ConclusõesOs pacientes com CC evidenciaram uma maior tendência a apresentar psicopatologia, sendo o sexo feminino mais predisposto a sofrer com os efeitos do desajustamento psicossocial. O suporte social revelou um papel preponderante no ajustamento dos doentes.
Congenital heart disease (CHD) is the result of abnormalities that occur during gestation leading to malformations of the heart or blood vessels.1
Developments in medical and surgical treatment have improved survival, and 85–90% of children with CHD now live to adulthood with a reasonable quality of life.1–3
As advances in treatment at various levels have enabled CHD patients to live increasingly longer and with fewer limitations, the question of their adjustment to their condition has attracted increasing attention.4 It is thus essential to understand the effects of CHD at all levels, as the literature shows conflicting results.5–8
While some studies have reported a tendency for behavioral and emotional problems in these patients,5,9,10 others have revealed adaptive psychological functioning in adults with CHD.11 Similarly, in some studies more severe CHD appears to be associated with worse psychosocial adjustment and psychiatric morbidity,6,9 but others do not support this finding.9
There have also been conflicting results in terms of quality of life, with some studies reporting worse psychological well-being and quality of life compared to the healthy population,4,12 and others finding no correlation between the presence of CHD and lower quality of life, with similar results to those found in healthy subjects.13,14
This study aimed to assess psychosocial adjustment, psychiatric morbidity and quality of life in a population of adolescents and young adults with CHD, with or without surgical repair, in order to clarify the impact of certain demographic and clinical variables on increasing resilience and adaptation or worsening adjustment and well-being.
MethodsThe study included 74 patients with CHD, who were approached to participate in the study on a single occasion during attendance at the pediatric cardiology or cardiology outpatient clinics. Adult patients or caregivers in the case of minors gave their informed consent after all aspects of the study had been explained.
Of the 74 patients, 41 were male and 33 were female. The mean age of the participants was 18.76±3.86 years (range 12–26).
CHD was complex in 27, moderate in 13 and mild in 34. With regard to residual lesions, four had severe, 18 moderate and 52 mild lesions. Seventeen participants (23%) had been diagnosed with at least one form of psychopathology during their lives.
Of the total study population, 40 had been diagnosed during the neonatal period, 28 in the first year of life, three between the ages of one and three, and three between the ages of three and six.
Of the participants who had undergone surgery, the first intervention had been performed during the neonatal period in two, in the first year of life in 24, between the ages of one and three in 15, between the ages of three and six in 16, and between the ages of six and 12 in three.
With regard to level of education, nine had completed the second cycle, 27 the third cycle, 33 secondary education, and five had a university degree. Most participants (69) were single, two were married, two were in a civil union and one was divorced.
Sixty-four caregivers accompanying patients also participated in the study by completing a questionnaire; 10 refused to participate or were not present at the time of application of the protocol and subsequently expressed no desire to participate.
The instruments used in the study included a personal record, a semi-structured interview, a standardized psychiatric interview (Schedule for Affective Disorders and Schizophrenia – Lifetime version [SADS-L]), the Youth Self Report (YSR) and Child Behavior Checklist (CBCL) for patients aged under 18, and the Adult Self Report (ASR) and Adult Behavior Checklist (ABCL) for those aged 18 or over. The short version of the World Health Organization Quality of Life questionnaire (WHOQOL-Bref) was also applied.
Each participant's personal record covered demographic variables, including civil status, educational level and profession, and clinical history, including diagnosis, severity and type of CHD, description of surgery, residual lesions and drug therapy.
The semi-structured interview, consisting of 38 multiple-choice or short-answer questions, covered areas such as social support, family environment, functional limitations, school performance and self-image.
The standardized psychiatric interview SADS-L was used to assess the presence of psychopathology.
YSR and ASR are self-report questionnaires designed to characterize a child's or adult's functioning, respectively. For the purposes of this study, responses were analyzed on the scales related to withdrawal, somatic complaints, anxiety and depression, thought problems, attention problems, rule-breaking behavior, aggressive behavior, internalization and externalization. Responses on the YSR scale related to social problems were not considered since the ASR does not have an equivalent scale.15
The CBCL and ABCL are designed to be completed by someone who knows the patient well (parent or caregiver), describing their perception of a patient's functioning and behavior.
Since the YSR/ASR and CBCL/ABCL are similar instruments, the scores were combined in order to obtain a larger number of responses and thus greater representativeness, the total scores for each scale being used in the statistical analysis.
WHOQOL-Bref is a quality of life self-report questionnaire that can be applied in healthy subjects or individuals with any type of disease.16 It consists of 26 questions, with responses rated on a five-point Likert scale, in which 5 corresponds to the highest rating, except in the case of the negatively formulated questions 3, 4 and 26, for which 5 is the lowest rating.
The statistical analysis was performed using the IBM Social Package for the Social Sciences (SPSS), version 19.0. The Student's t test was used for parametric variables and the Mann-Whitney test for nonparametric variables.
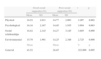
ResultsTable 1 shows differences in self-reported psychosocial adjustment between the sexes.
Mann-Whitney test for gender differences in self-reported psychosocial adjustment.
| ASR/YSR | M (n=41) | F (n=33) | U | p |
| Mean | Mean | |||
| Withdrawal | 36.30 | 38.98 | 725.500 | 0.591 |
| Somatic complaints | 32.39 | 43.85 | 886.000 | 0.021 |
| Anxiety/depression | 30.77 | 45.86 | 952.500 | 0.003 |
| Thought problems | 31.33 | 45.17 | 929.500 | 0.005 |
| Attention problems | 33.41 | 42.58 | 844.000 | 0.067 |
| Rule-breaking behavior | 36.78 | 38.39 | 706.000 | 0.744 |
| Aggressive behavior | 29.63 | 47.27 | 999.000 | 0.000 |
| Internalization | 31.18 | 45.35 | 935.500 | 0.005 |
| Externalization | 34.18 | 41.62 | 812.500 | 0.139 |
ASR: adult self report; F: female; M: male; U: Mann-Whitney test; YSR: youth self report.
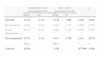
Table 2 shows differences in psychosocial adjustment between participants with complex CHD and those with moderate or mild forms.
Mann-Whitney test for differences in self-reported psychosocial adjustment according to severity of CHD.
| ASR/YSR | Complex(n=27)Mean | Moderate/mild(n=47)Mean | U | p |
| Withdrawal | 43.54 | 34.03 | 471.500 | 0.065 |
| Somatic complaints | 43.93 | 33.81 | 461.000 | 0.049 |
| Anxiety/depression | 38.59 | 36.87 | 605.000 | 0.740 |
| Thought problems | 44.63 | 33.40 | 442.000 | 0.027 |
| Attention problems | 35.00 | 38.94 | 702.000 | 0.446 |
| Rule-breaking behavior | 42.56 | 34.60 | 498.000 | 0.119 |
| Aggressive behavior | 43.22 | 34.21 | 480.000 | 0.081 |
| Internalization | 45.11 | 33.13 | 429.000 | 0.021 |
| Externalization | 34.85 | 39.02 | 706.000 | 0.422 |
ASR: adult self report; U: Mann-Whitney test; YSR: youth self report.
Table 3 shows differences in psychosocial adjustment between participants who had undergone surgery and those who did not require surgical intervention, as assessed by caregivers.
Mann-Whitney test for differences in psychosocial adjustment between patients with and without surgical intervention, as reported by caregivers.
| ABCL/CBCL (CR) | Surgery (n=54) | No surgery (n=11) | U | p |
| Mean | Mean | |||
| Withdrawal | 32.67 | 34.64 | 315.000 | 0.751 |
| Somatic complaints | 30.87 | 43.45 | 412.000 | 0.041 |
| Anxiety/depression | 31.35 | 41.09 | 386.000 | 0.117 |
| Thought problems | 30.94 | 43.14 | 408.500 | 0.040 |
| Attention problems | 33.21 | 31.95 | 285.500 | 0.840 |
| Rule-breaking behavior | 32.88 | 33.59 | 303.500 | 0.907 |
| Aggressive behavior | 34.06 | 27.82 | 240.000 | 0.317 |
| Internalization | 32.70 | 34.45 | 313.000 | 0.779 |
| Externalization | 32.96 | 33.18 | 299.000 | 0.972 |
ABCL: adult behavior checklist; CBCL: child behavior checklist; CR: caregiver report; U: Mann-Whitney test.
Table 4 shows differences in psychosocial adjustment between participants with satisfactory school performance compared to those with poor performance.
Mann-Whitney test for differences in self-reported psychosocial adjustment between participants with satisfactory vs. poor school performance.
| ASR/YSR | Poor school performance (n=26)Mean | Satisfactory school performance (n=48)Mean | U | p |
| Withdrawal | 44.75 | 33.57 | 812.500 | 0.031 |
| Somatic complaints | 38.94 | 36.72 | 661.500 | 0.667 |
| Anxiety/depression | 46.35 | 32.71 | 854.000 | 0.009 |
| Thought problems | 43.52 | 34.24 | 780.500 | 0.070 |
| Attention problems | 48.25 | 31.68 | 903.500 | 0.001 |
| Rule-breaking behavior | 40.25 | 36.01 | 695.500 | 0.410 |
| Aggressive behavior | 41.29 | 35.45 | 722.500 | 0.263 |
| Internalization | 44.92 | 33.48 | 817.000 | 0.029 |
| Externalization | 44.40 | 33.76 | 803.500 | 0.042 |
ASR: adult self report; U: Mann-Whitney test; YSR: youth self report.
Table 5 shows the prevalence of diagnosed psychopathology compared to the references values of other studies.
Prevalence of diagnosed psychopathology compared to references values of various other populations.
Percentage of adult population worldwide with mental and behavioral disorders, as assessed by the World Health Organization.17
It should be noted that the prevalence of psychopathology among female participants was more than twice as high as in males (33.3% and 14.6%, respectively, a statistically significant difference).
Table 6 compares results in the study population with reference values for the Portuguese population as a whole for all quality of life domains.
Means and standard deviation for the four quality of life domains and general quality of life in the study participants and the Portuguese population as a whole.
| Reference valuesa | Study population | t | p | |||
| Mean | SD | Mean | SD | |||
| Physical | 77.49 | 12.27 | 75.29 | 13.516 | −1.400 | 0.166 |
| Psychological | 72.38 | 13.50 | 73.34 | 13.924 | 0.590 | 0.557 |
| Social relationships | 70.42 | 14.54 | 74.91 | 16.573 | 2.333 | 0.022 |
| Environmental | 64.89 | 12.24 | 70.65 | 13.209 | 3.754 | 0.000 |
| General | 71.51 | 13.30 | 72.47 | 15.89 | 0.518 | 0.606 |
Table 7 shows differences in quality of life between participants who had undergone surgery and those who did not require surgical intervention.
Student's t test for the four quality of life domains and Mann-Whitney test for general quality of life, comparing patients who had undergone surgery with those who did not.
| Surgery(n=60) | No surgery(n=14) | t | p | |||
| Mean | SD | Mean | SD | |||
| Physical | 15.81 | 2.224 | 17.06 | 1.567 | −1.989 | 0.050 |
| Psychological | 15.46 | 2.304 | 16.71 | 1.557 | −1.928 | 0.058 |
| Social relationships | 15.69 | 2.634 | 17.24 | 2.409 | −2.012 | 0.048 |
| Environmental | 15.14 | 2.207 | 16.04 | 1.525 | −1.443 | 0.153 |
| Mean | Mean | U | p | |||
| General | 35.12 | 47.71 | 563.000 | 0.037 | ||
SD: standard deviation; t: Student's t test; U: Mann-Whitney test.
Table 8 shows differences in quality of life between those with good or poor social support.
Student's t test for the four quality of life domains and Mann-Whitney test for general quality of life, comparing participants with good or poor social support.
| Good social support(n=54) | Poor social support(n=20) | t | p | |||
| Mean | SD | Mean | SD | |||
| Physical | 16.52 | 2.011 | 14.77 | 2.083 | 3.287 | 0.002 |
| Psychological | 16.16 | 2.167 | 14.45 | 1.935 | 3.094 | 0.003 |
| Social relationships | 16.62 | 2.143 | 14.27 | 3.145 | 3.669 | 0.000 |
| Environmental | 15.70 | 1.901 | 14.25 | 2.348 | 2.725 | 0.008 |
| Mean | Mean | U | p | |||
| General | 41.52 | 26.65 | 323.000 | 0.005 | ||
SD: standard deviation; t: Student's t test; U: Mann-Whitney test.
Table 9 shows differences in quality of life between participants with satisfactory or poor school performance.
Student's t test for the four quality of life domains and Mann-Whitney test for general quality of life, comparing participants with satisfactory or poor school performance.
| Satisfactory school performance(n=48) | Poor school performance(n=26) | t | p | |||
| Mean | SD | Mean | SD | |||
| Physical | 16.42 | 2.192 | 15.36 | 1.968 | 2.045 | 0.045 |
| Psychological | 16.06 | 2.218 | 15.03 | 2.127 | 1.950 | 0.055 |
| Social relationships | 16.15 | 2.327 | 15.67 | 3.185 | 0.752 | 0.455 |
| Environmental | 15.73 | 2.210 | 14.52 | 1.708 | 2.413 | 0.018 |
| Mean | Mean | U | p | |||
| General | 40.98 | 31.08 | 457.000 | 0.046 | ||
SD: standard deviation; t: Student's t test; U: Mann-Whitney test.
It should be noted that 51.4% of participants had failed exams at school (mean 1.74±0.86 years).
DiscussionIn this study, female participants presented significantly more somatic complaints, higher indices of anxiety and depression, thought problems and aggressive behaviors, and a higher degree of internalization, and hence worse psychosocial adjustment.
The gender differences observed in CHD patients may be linked to the presence of a surgical scar on the chest, affecting body image and self-esteem and contributing to feelings of insecurity and uncertainty in personal and sexual relations. Another factor leading to insecurity in these patients may be fears that the disease could affect their reproductive capacity and childbirth.5,6,20
Female patients also tend to be more concerned about their bodies than males,5 and be more likely to experience anxiety and depression when faced with situations that hinder interpersonal relationships, reflected in a greater tendency for internalization.5,6 They thus have a higher risk of presenting emotional and behavioral problems than their male counterparts.21
Patients with complex CHD more often report somatic complaints and thought problems and have higher indices of internalization than those with moderate or mild CHD. This suggests that adolescents and young adults with complex CHD present worse psychosocial adjustment, which may be related to their need for more medical care throughout their lives, while those with mild or moderate CHD are more able to lead a similar life to healthy individuals of the same age.6,22
Since complex CHD presents a higher risk than mild or moderate CHD, it is understandable that adolescents and young adults with a complex form should report more somatic complaints, as they are more alert to the signs produced by their bodies. This will tend to interfere with their thought processes, making them more anxious about possible complications (anxiety is one component of the internalization scale).
When assessed by caregivers, individuals who had not undergone surgery more often presented somatic complaints and thought problems, which suggests that surgical repair plays an important role in improving quality of life in CHD patients.9,23
Patients with CHD require regular medical care, which means that many have to miss school, which in turn leads to poor performance, anxiety and depression, attention problems, and higher indices of internalization and externalization; this is reflected in our study's results, which show that patients with poor school performance presented worse psychosocial adjustment.1,23–26
With regard to psychiatric morbidity, 23% of our subjects had been diagnosed with a mental disorder. Based on the World Health Organization estimate of 10% for the adult population worldwide, this suggests that adolescents and young adults with CHD are more prone to psychopathology.17
However, the prevalence of 23% in our study population was comparable to that reported for the general population in six European countries (25%).18 Similar results were also observed for lifetime prevalence of mental disorders in Spain (19.4%), Italy (18.1%) and Germany (25.2%), although the figures were much higher in France (37.9%) and the USA (47.4%).19
It would be useful to compare the prevalence of psychopathology among our patients with estimates for the general Portuguese population, but such figures are not yet available, and this is one of the major limitations of our study.
With regard to the gender distribution of psychopathology, its prevalence was more than twice as high in female participants, a finding that is consistent with their worse psychosocial adjustment and with reported prevalences of mental disorders, particularly anxiety and depression, in population studies in various countries.
Our population of CHD patients reported a better quality of life compared to the reference values for the healthy Portuguese population in the social relationships and environment domains, while other authors have found a worse quality of life than for the normal population, particularly in the WHOQOL-Bref physical and general quality of life domains, as well as in the psychological and social domains, albeit less marked.12
Individuals who had not undergone any form of surgery reported a better quality of life in physical, social relationships and general terms on self-assessment than those who had. While most CHD patients who undergo surgical repair succeed in functioning normally in most areas of their lives, there are certain developmental issues in cases of complex or moderate disease, which make long-term planning more difficult for these patients.27
Social support was shown to have an important impact on quality of life, individuals with greater support presenting better quality of life in all the domains assessed, particularly in physical, psychological, social relationships, environmental and general terms.
Social support, at the individual, family or community level, has a major impact as a mediator between stress and psychological well-being; patients’ perception of its availability is extremely important in counteracting the effects of the stress caused by both physical and mental health problems.28
Individuals with a satisfactory school performance present a better quality of life in physical, environmental and general terms, as well as in psychological adjustment. School performance can be severely affected by CHD, as patients often require hospitalization and may have restrictions on activities with their peers, both of which mean they are regularly excluded from school activities.1,29
ConclusionsThe study's results appear to show that adolescents and young adults with CHD are prone to emotional and behavioral problems. Female patients were more likely to have worse psychosocial adjustment, as were those with complex CHD, those who had not undergone surgical intervention (according to caregivers), and those with poor school performance.
With regard to psychiatric morbidity, the data for this population appear to indicate a slightly higher likelihood of suffering some form of mental disorder.
By contrast, the study participants reported a better quality of life than the general Portuguese population, highlighting the importance of social support.
Nevertheless, despite the role of various types of social support, the fact that CHD is diagnosed at an early stage of life means that patients have to draw on all their skills to deal with the challenges of developmental milestones and to live a normal life, albeit with certain limitations, many of which can be overcome by coping strategies.
FundingThis research was funded by CESPU.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Coelho R, Teixeira F, Silva AM, et al. Ajustamento psicossocial, morbilidade psiquiátrica e qualidade de vida em adolescentes e jovens adultos com cardiopatias congénitas. Rev Port Cardiol. 2013;32:657–664.