Prof. John Barlow (Figure 1) gained his place amongst the giants of Cardiology because of his discovery of the mechanism of the mitral valve failure that became known as the Barlow Syndrome. There is great confusion amongst the cardiological fraternity about syndrome, disease and prolapse. Although Prof. Barlow was one of the first to characterize mitral valve prolapse, his real contribution was in deciphering “The significance of late systolic murmurs and mid-late systolic clicks”. He attributed these sounds to the mitral valve mechanism. Prior to that, they were thought to be of extra-cardiac origin, including pericardial adhesions. The paper under this name had been initially rejected by the principal scientific journals of the time on the grounds that it was “too extreme to claim that the cause was due to the mitral valve mechanism” and was only published in February 1963 in the Maryland State Medical Journal, which was directed by a friend of his.1 This was immediately followed by a publication (October 1963) in the American Heart Journal under the name of “The significance of late systolic murmurs”, with the description of auscultatory findings in seven patients2.
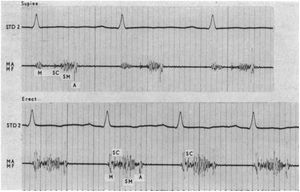
The concept was later expanded in another paper published in the American Heart Journal, in 1966, as “Aneurysmal protrusion of the posterior leaflet of the mitral valve. An auscultatory-electrocardiographic syndrome“,3 and in the British Heart Journal, in 1968, under the title of “Late systolic murmurs and non-ejection (“mid-late”) systolic clicks. An analysis of 90 patients”.4 These purely auscultatory findings (there was no echocardiography in those days, but they could be registered by phonocardiography - Figure 2) define the true Barlow Syndrome.
These findings were confirmed in autopsies and were associated to myxoid degeneration of the mitral valve; hence, the confusion with what was later termed Barlow's disease. What Prof. Barlow described was a specific “auscultatory-electrocardiographic” syndrome characterized by a billowing leaflet, a term he preferred to prolapse, which consisted of the protrusion of the leaflet body to the atrial side, above the annulus, without the significant regurgitation that characterizes prolapse, from which it can now be clearly differentiated by the echocardiogram.
Symptoms of the syndrome include anxiety, chest pain and palpitations. The resting electrocardiogram may show ST-segment and T-wave abnormalities. A billowing mitral posterior leaflet was often demonstrated by cine-angiocardiography in patients with late systolic murmurs. It is common in young women and the majority of patients had a benign course and required reassurance only, although sudden death could occur.5,6
Of interest, part of the findings were confirmed in a survey of 12 050 urban black schoolchildren conducted by Prof. Barlow and collaborators in 1972, which detected 168 (prevalence rate of 14 per 1000) with a non-ejection systolic click, a late systolic murmur, or both.7 The etiology of the mitral valve abnormality was then unknown but they considered that a significant proportion might have early rheumatic heart disease. The evolution in these children did not confirm the rheumatic etiology, but this study demonstrated the high prevalence of acute rheumatic fever in the region. Because Prof Barlow linked it with the poor socio-economic conditions of this population, he was then heavily criticized by the country's government of the time.8
The paper published in the American Heart Journal in 19663 became one of the most cited works in the area of cardiology and was designated a citation classic by the Institute for Scientific Information, in 1983.
The Man, the Scientist1John Brereton Barlow was born in South Africa on 24 October 1924 and qualified as a medical doctor in 1951, at the University of the Witwatersrand, Johannesburg. He had entered medical school in 1940 but interrupted his studies soon afterwards when South Africa became involved in World War II and he enlisted in the military. He spent time with British forces in North Africa and with the Fifth US Army in Italy. After graduation, he became a registrar (resident) at the Baragwanath Hospital in Johannesburg, but moved to the Hammersmith Hospital in London two years later and further to the Royal Postgraduate Medical School, where he worked under another famous cardiologist, Sheila Sherlock, whom he always mentioned with great respect and admiration.
Right from the beginning, the young John Barlow developed an interest in auscultation and phonocardiography, which led him to investigate the non-ejection clicks and late systolic murmurs that characterize the Syndrome. Curiously, he had previously (1958) published a paper on “The use of amyl nitrite in differentiating mitral and aortic systolic murmurs”, in the British Heart Journal,9 while still in England, and another one in 1962, already from South Africa, under the title of “The significance of aortic ejection systolic murmurs”, in the American Heart Journal.10
In the late 1950s, he returned to the Johannesburg Hospital where he became head of the Cardiology Unit, in 1971, and Professor of Cardiology, in 1980. His ongoing research included significant studies on several cardiac disorders, especially in the valve area, with seminal works on the mitral and tricuspid valves. The name and fame of Prof. Barlow attracted a large number of international fellows who spent different lengths of time to absorb the master's knowledge. Internally, he was widely acknowledged as an excellent clinician and his opinion was sought by patients from all walks of life, from poor children from Soweto to high levels of society. One of his most famous patients was Nelson Mandela. He was awarded some of the highest national and international distinctions.
Prof. Barlow demonstrated an eccentric character, virtually emotionless, both in his personal and professional life. He had an innovative mind, limitless energy and enthusiasm, great sense of humour (sometimes not easy to perceive) and immense dedication to principles. Clinically, he was noticeable by the time and patience he placed in taking the patients’ medical history and in the physical examination. He could easily spend 10 or 15 min observing the neck of a patient to evaluate the degree of tricuspid regurgitation. In the end, he could tell what the a, c and v-waves of the jugular venous pressure were. One of his typical phrases was “when all else fails, examine the patient”!
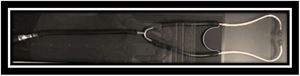
He took great pride on his stethoscope, with several bells and diaphragms, which he religiously interchanged while auscultating the same patient (Figure 3). He often passed the ear-pieces to the people around him, especially the residents, to teach them the characteristics of the sounds or murmurs. In fact, he was the “echo machine” that did not exist yet, and was most of the times proven right when the surgeons opened the patient's chest. His ears must have been true hi-fi systems. To complement these pedagogic activities, he edited a series of “long-play” 12-inch vinyl records with sounds and murmurs!
He tended not to trust medical tests. His theory that “severe aortic valve stenosis and significant coronary disease could not co-exist, as they were incompatible” became famous. This was one of only a few things that proved him wrong! He was usually adamant in his convictions and always had a “superiority” speech, but he listened to the senior collaborators who, on the other hand, had the greatest respect for his opinions. But he could be hard on those who flouted the rules. As Prof. Tom Bothwell, another giant of South African medicine, said, “Barlow was intolerant of mediocrity, intolerant of his own (and others’) failings, when not attaining absolute recall, and meticulous attention to medical detail and offering a ‘sloppy’ diagnosis”! But he could be kind and considerate, especially to the patients.
Every Saturday morning, he chaired a clinical meeting, attended by almost everybody in the Cardiology and Cardiac Surgery medical staff, where every single patient proposed for surgery was discussed. The concept of Heart Team was already practiced there, more than 5 decades ago! In these meetings his doctrine that “current dogma should always be questioned and challenged” was always present in everybody's mind. In a plaque outside the cathlab of his Clinic he wrote in 1984: “It is my hope that members of this staff will always question that which appears to be obvious, and clarify whatever is not understood”.
Prof John Barlow was, indeed, a remarkable Man, a superb Physician and a supreme Cardiologist.
My professional relationship with Prof. BarlowWith over four decades in cardiac surgery, which constitutes two thirds of the history of our discipline, I had the opportunity to meet many legends in cardiology and cardiac surgery and work with some. But John Barlow was, perhaps, the one that marked me the most.
I first met “The Professor” in August 1976, only a couple of weeks after I initiated my training in cardiothoracic surgery. I was attending the Thursday afternoon ward round in the cardiac surgical unit, which he ran every week, religiously, having to travel some 20 Km from his own unit. I was in the second or third row, watching his painfully long examination of a patient, noting that his eyes had turned on me several times. Suddenly, he lifted the stethoscope and asked in his loud and hard voice: “who is that chap?” I felt like running away as fast as possible! In the end, he greeted me with a warm welcome.
This happened at the Baragwanath Hospital, for black patients (we were still in the era of the apartheid), the largest hospital in the southern hemisphere with its more than 3500 beds and 1.5 million patients attended per year. It was there that I had the most fundamental part of my learning of cardiac surgery and where I initiated my interest in mitral valve repair in rheumatics, then just an annuloplasty, with undefined results, even before I became a specialist surgeon.11 He incentivized me to go to Paris and learn the Carpentier techniques of mitral valvuloplasty, and accompanied me in my initial experience.
Again, he was my first “echo-machine”, before I had access to a real one. He used to write his assessment of the valve both before and after I operated on the patient, using a red BIC-pen – one of his eccentricities, always accompanied by a verbal encouraging word. I remember vividly a case in whose notes he wrote (in red): “no one in this world will be able to repair this valve”, only to add, a week later, after I successfully accomplished the repair: “no one, perhaps with the exception of Manuel Antunes”! He knew very well that my reaction to his preliminary note would be to do all the possible (and the impossible) to repair that valve!
When I wrote my book on Mitral Valve Repair in 1989,12 a sequence of my PhD thesis, he, together with Prof. Carpentier, wrote a preface. There he stated: “When a surgeon, such as Professor Antunes, has indeed mastered the ‘French Correction’, then even a somewhat conservative cardiologist, such as I, has felt justified in supporting his endeavours with difficult rheumatic cases. I am now even more confident in referring patients to him for a constructive repair in patients who have non-rheumatic prolapsed leaflets, irrespective of whether the mitral regurgitation is hemodynamically, moderate, moderate or even fairly mild. When resort to valve replacement is improbable, a policy of earlier surgical management can be substantiated”. How advanced were we in 1988! One day, he convinced me to operate on a young woman with Barlow syndrome, with no mitral regurgitation, whose only problem were repeated and prolonged episodes of tachycardia. It resulted well!
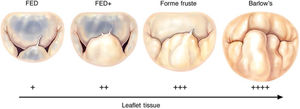
Further to that, Prof. Barlow also took great pride in teaching me how to properly auscultate a heart and the secrets of sounds and murmurs. And I still remember the long discussions we had about billowing versus prolapse and Barlow Syndrome versus Barlow Disease, the extreme form of the degenerative mitral valve spectrum described by another giant in cardiology, Alain Carpentier (Figure 4).
To show how advanced was he on his time, he frequently discussed with me and the other surgeons the importance of performing tricuspid annuloplasty together with surgery on the mitral valve; he believed that tricuspid annular dilatation was “often partly or mainly organic”, hence the natural progression of the regurgitation. He described “the restriction-dilatation syndrome”, which portraits the role of tricuspid regurgitation in perpetuating late-onset heart failure after mitral valve surgery. This was clearly stated in his book Perspectives on the Mitral Valve, in which I participated in three chapters.13 The book was published in 1986, long before the extensively cited publication by Dreyfus, in 2005, which revolutionized the attitude of cardiac surgeons towards secondary tricuspid regurgitation. Why did I not listen to him then?
Prof Barlow kept his support throughout my ascension in the hospital and university career over one decade, until I applied for the position of Chief Surgeon and Professor of the University of the Witwatersrand. The previous professor, Robin Kinsley, to whom I owe much of what I know, had decided to leave for private practice and the position became vacant. Prof. Barlow was very fond of Prof. Kinsley and was acutely saddened by the loss. I was appointed to the position, I am sure with his strong support, but he wanted me to be a second Kinsley, which, for the better or for the worse, I was not. One day, after he criticized something I had done differently, I reminded him that, although I greatly respected him for what he was and had done for me, I was now at his same level, as head of a department and university professor. May be I was unkind and too hard, but I was still struggling to get hold of my department and could not tolerate outside interferences, even by Prof. Barlow.
I could see the anger in his eyes - nobody had ever spoken to him like that. He stopped talking to me for a while, but then Providence played in my favor. I already wrote about Barlow's stethoscope and its special characteristics, which made it ‘unique’ in the world. Upon going home after a day's work, Prof. Barlow had the habit of taking his stethoscope from around the neck, place it on the roof of the car while taking out his white coat. One day, he forgot to place the stethoscope back into the car and it got lost! It was as if heaven had fallen over his head; because of its uniqueness, the stethoscope was irreplaceable! I and the others around decided to buy him a new stethoscope, with all the sound properties available at that time; but it obviously was not Barlow's stethoscope!
Some time later, a patient of mine phoned and asked to meet me as he had something in which I could be interested. Imagine my surprise when I saw Barlow's stethoscope in his hands, which he wanted to offer me as a gift. I was fast to phone Prof. Barlow and ask him to receive me. I went to his office and put the stethoscope on top of his desk, right in front of his eyes. For the first time, I saw Prof. Barlow drop a few tears – after all, the man also had emotions! From that moment on, our relationship normalized and I could again take advantage of his immense knowledge. I left Johannesburg only a year later, in 1988, and I am sure that Prof. Barlow missed me, although he obviously never showed the feeling. Back in Portugal, in 1988, I continued to correspond with him and even wrote a final paper with him on the tricuspid valve, published in Heart in 2007.14 It was the last paper with his name.
Prof. Barlow died on 10 December 2008. I will always remember him. Also for the words in the dedication in his abovementioned book, which reads: “To all the students who listen, look, touch and reflect: may they hear, see, feel and comprehend”. I was blessed to have been his student and to have heard, seen, felt and comprehended him!
Some biographical notes from Wikipedia (https://en.wikipedia.org/wiki/John_Brereton_Barlow - accessed 17/08/2019).
Previously published in Cirugía Cardiaca en México, Antunes, MJ. Professor John Barlow - The Legend. Cir Card Mex 2020; 5(1): 1-5. Reproduced with permission.