An exaggerated accumulation of type I and type III fibrillar collagens occurs throughout the free wall and interventricular septum of patients with primary hypertension and left ventricular hypertrophy (LVH). In the present study the serum concentration of procollagen type III amino terminal peptide (PIIIP) was measured to determine the value of this peptide as a potential marker of ventricular fibrosis in hypertensive patients, particularly those with LVH.
MethodsThe study population consisted of patients with never-treated mild to moderate essential hypertension and 30 normotensive control subjects. Clinical, echocardiographic, electrocardiographic and biochemical parameters were assessed in all patients.
ResultsHeart rate, body mass index and levels of blood pressure were increased in hypertensives, particularly those with LVH, compared to normotensive controls. Posterior wall thickness, left ventricular (LV) mass and LV mass index, and serum PIIIP concentration were also increased in hypertensives, with significant differences between the two hypertensive groups. The ratio between maximal early and late transmitral flow velocity measured during diastole was lower in hypertensives, particularly those with LVH, than in normotensive controls.
ConclusionsThe increase in PIIIP indicates that type III collagen synthesis increases in hypertensives, particularly those with LVH, implying that alterations in the heart in hypertension are the result not solely of hypertrophied LV muscle, but also of increased collagen deposition within the ventricular wall and around the coronary vessels.
Thus, measurement of serum PIIIP could be a practical and useful tool in the non-invasive assessment of myocardial remodeling in hypertension.
Nos doentes com hipertensão arterial (HT) ocorre uma acumulação exagerada de fibras de colagénio tipo I e III quer a nível da parede livre, quer ao longo do septo interventricular do ventrículo esquerdo. Esta acumulação é mais marcada nos HT que apresentam hipertrofia ventricular esquerda. O objetivo do presente estudo, foi a determinação da importância da concentração sérica de procolágeno tipo III, como marcador de fibrose miocárdica, nos hipertensos, principalmente com hipertrofia ventricular esquerda.
MétodosA população estudada era composta por pacientes com ligeira a moderada hipertensão essencial nunca tratados (HT) e por 30 pacientes normotensos. Os parâmetros clínicos, ecocardiográficos, eletrocardiográficos e bioquímicos foram avaliados em todos os pacientes.
ResultadosOs hipertensos apresentavam valores de pressão arterial, frequência cardíaca e índice de massa corporal aumentados quando comparados com os normotensos. Os hipertensos apresentavam valores mais elevados de índice de massa do ventrículo esquerdo e de concentração sérica de PIIIP, e menor relação entre as velocidades de fluxo mitral máxima precoce e a máxima final avaliadas durante a diástole. Os HT com hipertrofia ventricular esquerda apresentavam diferenças significativas destes parâmetros em relação aos HT e normotensos sem hipertrofia ventricular esquerda.
ConclusãoA concentração sérica PIIIP no soro poderá ser um marcador útil e prático para avaliar de forma não invasiva a remodelação miocárdica, bem como um índice do colagénio depositado nestes pacientes hipertensos, podendo apoiar na escolha criteriosa do tratamento mais eficaz da hipertensão arterial.
The myocardium contains types I and III collagen as major fibrillar collagens. These collagens are constantly synthesized and secreted as procollagens in the interstitial space. Increased collagen turnover has been associated with myocardial fibrosis and plays an important role in determining the functional properties of the arterial vasculature and ventricular myocardium. An exaggerated accumulation of type I and type III fibrillar collagens occurs throughout the free wall and interventricular septum of patients with primary hypertension1,2 and left ventricular (LV) hypertrophy (LVH).3
Types I and III collagen are synthesized as procollagens with a small amino terminal and a larger carboxy terminal propeptide. Once secreted into the extracellular space, the propeptides are removed by specific endopeptidases, thus allowing integration of the rigid collagen triple helix into the growing fibril.4 The three-amino acid procollagen type III amino terminal peptide (PIIIP) formed during this process is released into the blood. The serum concentration of PIIIP has been proposed as a useful marker of type III collagen synthesis.5 This is supported by a variety of clinical observations demonstrating that high serum levels of the peptide reflect on-going tissue fibrosis.6 Other authors have shown that serum PIIIP concentration is abnormally increased in a small group of patients with essential hypertension,7 thus suggesting that type III collagen turnover is also increased in this condition.
It has been proposed that the excess of myocardial collagen seen in hypertension is the result of both increased collagen synthesis and unchanged or decreased collagen degradation. The development of LVH depends not only on the renin-angiotensin system generating angiotensin II,8 but also on mechanical stress, which activates the protein kinase cascade of phosphorylation in cardiac myocytes.9
In the present study serum PIIIP concentration was measured to assess more accurately the intensity of the fibrogenic process in patients with essential hypertension. In addition, the relation between serum PIIIP concentrations and various parameters of LV anatomy and function were analyzed to determine the value of this peptide as a potential marker of ventricular fibrosis in hypertensive patients.
MethodsThe study population consisted of patients with never-treated mild to moderate essential hypertension and 30 normotensive control subjects. All subjects gave their informed consent and the local human research ethics committee approved the study protocol.
Blood pressure was measured in the morning, after 10 min in the supine position, using a mercury column sphygmomanometer. Phases I and V of the Korotkoff sounds were used; three measurements were obtained on each occasion, at 5-min intervals, and averaged. Hypertension was defined as present if systolic and diastolic blood pressure were ≥140 and 90 mmHg, respectively. All patients underwent appropriate clinical and laboratory assessment to exclude hypertension secondary to the following: renal disorders, renal artery abnormalities, adrenocortical disorders, pheochromocytoma, and iatrogenic causes. Conditions associated with elevated serum PIIIP concentrations (chronic liver disease, pulmonary fibrosis, rheumatoid arthritis, extensive wounds and acute myocardial infarction) were excluded after complete medical examination. We also excluded patients with overt coronary artery disease or other organic heart disease as shown by clinical, ECG, and echocardiographic criteria. None of the women were pregnant or taking oral contraceptives. The control group consisted of 30 subjects with blood pressure <140/90 mmHg in repeated measurements, referred to our center for suspected hypertension. None of the control subjects had echocardiographic evidence of cardiac disturbances.
Echocardiographic studyTwo-dimensional, targeted M-mode and Doppler ultrasound recordings were obtained in each patient. M-mode measurements were taken according to the guidelines laid down by the American Society of Echocardiography.10 LV mass was calculated using the formula validated by Devereux and Reichek.11 LV mass index (LVMI) was obtained by dividing LV mass by body surface area. Relative wall thickness (RWT) was measured at end-diastole as 2×(posterior wall thickness/internal dimensions). The presence of LVH was established either when LVMI was >111 g/m2 for men and >106 g/m2 for women or when RWT was >0.44.12 LV fractional shortening and ejection fraction were calculated according to Quinones et al.13 The following pulsed Doppler measurements were obtained: maximal early transmitral velocity in diastole (VE) and maximal late transmitral velocity in diastole (VA). A diagnosis of diastolic dysfunction was established when the VE/VA ratio was <1.14
Biochemical measurementsThe general biochemical assessment included plasma glucose concentration and serum lipid profile and measurement of serum potassium and serum and urine creatinine. Blood samples were drawn in a fasting state. Biochemical parameters were measured by routine laboratory methods. Renal creatinine clearance was calculated as the product of urine flow rate and urine creatinine concentration divided by serum creatinine concentration.
Serum samples to determine PIIIP and procollagen type I amino terminal peptide (PIP) were taken at the time of the clinical studies and stored at −40°C for up to six months. The six-month follow-up samples were analyzed together with samples from the initial setup. No changes were observed in samples analyzed twice.
Serum PIIIP was determined by a coated-tube radioimmunoassay as previously described by Risteli et al.,15 using commercial antisera specifically directed against the terminal amino terminal peptide (RIA-gnost Procollagen-III-Peptide, Behringwerke, Marburg, Germany). The inter- and intra-assay variations for determining PIIIP were both <10%. The sensitivity (lower detection limit) was 1.5 ng PIIIP/ml.
Statistical analysisValues are expressed as mean ± SEM. The one-way ANOVA test was used to assess the statistical significance of differences between control subjects and patients with and without LVH. The correlation between continuously distributed variables was tested by univariate regression analysis. A two-tailed p value of <0.05 was considered significant.
ResultsBaseline demographic, biochemical, ambulatory blood pressure monitoring, and echocardiographic parameters are presented in Table 1. As expected, blood pressure levels were higher in hypertensive patients, especially those with LVH, than in normotensive patients.
Baseline demographic, biochemical, ambulatory blood pressure monitoring, and echocardiographic parameters.
| Parameter | Normotensive patients | Hypertensive patients without LVH | Hypertensive patients with LVH |
|---|---|---|---|
| Age, years (range) | 57 (45–76) | 59 (34–68) | 58 (29–78) |
| Gender, male:female | 15:15 | 19:21 | 18:22 |
| SBP, mmHg | 125.1±6.2 | 154.2±23.0 | 161.4±26.1 |
| DBP, mmHg | 80.2±4.5 | 98±11 | 102±13 |
| HR, bpm | 72.2±6.7 | 82.1±15 | 87.1±13 |
| BMI, kg/m2 | 27.1±1.2 | 28.4±1.4 | 29.2±1.6 |
| Blood glucose, mg/dl | 93.2±3.6 | 89.2±5.9 | 95.2±8.9 |
| Cholesterol, mg/dl | 218.6±15.2 | 214.5±14.4 | 225.2±13.5 |
| Triglycerides, mg/dl | 110.5±16.7 | 135.2±14.6 | 136.2±12.2 |
| CCR, ml/min×1.73 m2 | 101.5±10.7 | 105.3±11.6 | 105.7±12.7 |
| ST, mm | 9.4±0.4 | 10.9±0.3 | 12.1±0.5 |
| PWT, mm | 8.5±0.12 | 9.45±0.22 | 10.43±0.24 |
| LVMI, g/m2 | 89.6±2.3 | 96.2±4.1 | 115.8±7.8 |
| VE/VA ratio | 1.48±0.02 | 1.03±0.03 | 0.89±0.05 |
| EF, % | 67±5.3 | 69.7±6.2 | 72±4.6 |
| PIIIP, ng/ml | 9.94±0.84 | 11.25±0.76 | 13.94±0.85 |
BMI: body mass index; bpm: beats per minute; CCR: creatinine clearance; DBP: diastolic blood pressure; EF: ejection fraction; HR: heart rate; K+: potassium; LVH: left ventricular hypertrophy; LVMI: left ventricular mass index; PIIIP: procollagen type III amino terminal peptide; PWT: posterior wall thickness; SBP: systolic blood pressure; ST: septal thickness; VE: maximal early transmitral velocity in diastole; VA: maximal late transmitral velocity in diastole.
Values are expressed as mean (range), mean ± SEM, or number of subjects.
Values are expressed as mean (range), mean ± SEM, or number of subjects.
Heart rate and body mass index were higher in hypertensive patients compared with normotensive patients. No other differences in clinical and biochemical parameters were found between the three groups.
Posterior wall thickness was increased in hypertensive patients compared with normotensive controls, and calculated LV mass and LVMI were also increased in the hypertensive groups, particularly in those with LVH. The VE/VA ratio was lower in the hypertensive patients, particularly in those with LVH, than in normotensive controls. Parameters of systolic function were within normal limits in all patients studied.
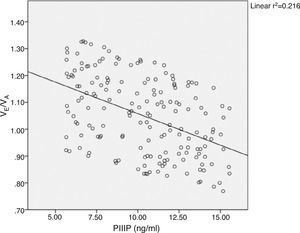
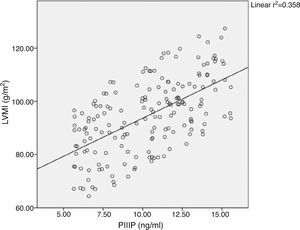
Considering all patients in the model, it can be seen that there is an inverse correlation between PIIIP and the VE/VA ratio (Figure 1) and a direct correlation between serum PIIIP concentrations and LVMI (Figure 2).
Like other authors,16 we found increased serum PIIIP concentrations in patients with essential hypertension.
PIIIP, like PIP,17 is eliminated from the blood by the liver. Considering that none of the patients studied showed impaired liver function, it could be assumed that the elevated serum PIIIP concentrations in hypertensive patients represent increased production of the peptide in the hypertensive heart, related to LVH. The half-life of collagen in hypertrophic myocardium is 17 days, compared to 80–120 days in normal myocardium. Furthermore, fibroblast proliferation may also contribute to increased collagen synthesis. This remodeling of collagen structure has been reported in hypertension,17,18 heart failure,19 stunned myocardium20 and myocardial infarction. In the present study, hypertensive patients with liver disease, lung disease, and diabetes were excluded because these conditions are also causes of elevated PIIIP.
Although serum PIIIP has been proposed as a useful marker of fibrogenesis,5,21 it should be noted that this peptide is not completely removed from its procollagen precursor during the extracellular processing of type III collagen.24
Serum PIIIP concentrations in hypertensive patients with LVH in this study were increased relative to the normal serum range of 0.25–0.7 U/ml and to patients without LVH. This finding was expected, since in vivo studies have shown that chronic elevation of circulating angiotensin II or aldosterone cause myocardial accumulation of fibrillar collagen. In vitro, effector hormones of the renin-angiotensin-aldosterone system have been shown to directly enhance collagen synthesis in rat fibroblasts. This may be of particular interest to explain the increased synthesis of type III collagen, since a direct correlation has been reported22 between serum PIIIP and plasma renin activity in hypertensive patients.
A variety of experimental and clinical findings indicate that cardiac collagen accumulation adversely influences diastolic relaxation and LV stiffness. We found that serum PIIIP concentrations are inversely correlated with the VE/VA ratio, suggesting that myocardial accumulation of type III collagen plays a role in diastolic dysfunction in patients with essential hypertension.
The findings presented here show an increase in serum PIIIP concentrations in patients with essential hypertension, which may be a marker of increased type III collagen in these patients. On the other hand, the relation observed between serum PIIIP and parameters of LV mass and diastolic function lead us to propose that circulating procollagen-derived peptides may reflect ongoing myocardial fibrosis in essential hypertension.
The correlations found demonstrate that in LVH there is collagen deposition and that this deposition is related to LV diastolic function and LVMI.
To summarize, an increase in serum PIIIP concentration indicates that type III collagen synthesis increases in hypertensive patients, particularly in those with LVE. Therefore, alterations in the heart in hypertension are the result not solely of hypertrophied LV muscle, but also of increased collagen deposition within the ventricular wall and around the coronary vessels. The results of these hemodynamic and structural LV alterations are usually recognized as electrocardiographic and echocardiographic LVH, which may be manifested clinically by angina pectoris and cardiac failure as well as silent ischemia, myocardial infarction and, of course, sudden death.
Measurement of serum PIIIP could therefore be a practical and useful tool in the non-invasive assessment of myocardial remodeling in hypertension. In particular, it may have clinical importance in documenting the extent of collagen accumulation and in evaluating pharmacological measures to prevent or even reverse this accumulation.
Nevertheless, because of the limitations of this investigation, we are aware that further large studies are necessary to validate this approach.
Study limitationsDue to its cross-sectional nature, this study should be considered hypothesis-generating at best, and no causal inferences can be drawn regarding pathophysiological mechanisms. Cardiac hypertrophy is a complex process that involves not only collagen turnover (both synthesis and degradation) but also degradation and formation of elastin and formation of collagen cross-links, as well as other spatial and mechanical alterations involving integrins, collagen and smooth muscle cells, regulated by a variety of cytokines and growth factors. This study was not designed to provide a comprehensive analysis of this plethora of regulatory factors. A study reporting serial changes in LVMI and PIIIP might provide better delineation of the temporal relationship between these two entities, providing crucial insights into the precise ways in which they modulate each other. Nevertheless, these findings provide a framework around which future investigations could be planned.
ConclusionsThis study demonstrates that an increase in serum PIIIP concentration indicates that type III collagen synthesis increases in hypertensive patients, particularly in those with LVE. Alterations in the heart in hypertension are thus the result not solely of hypertrophy of LV muscle, but also of increased collagen deposition within the ventricular wall and around the coronary vessels. The study also shows that there a relationship between PIIIP levels and LVMI.
Our results support a possible role for altered circulating collagen markers such as PIIIP that are associated with LVH, which in turn is an important correlate of ventricular mass in hypertensive patients.
Myocardial fibrosis may lead to relaxation abnormalities of the myocardium secondary to impairment of the relengthening of cardiomyocytes during the relaxation phase of the cardiac cycle. A reduced VE/VA ratio reveals impaired relaxation. Accumulation of collagen fibers within the myocardium is mainly responsible for an increase in intrinsic myocardial stiffness and a decrease in ventricular distensibility. We observed an inverse correlation between myocardial fibrosis and values for this parameter in all hypertensive patients.
The results of these hemodynamic and structural alterations affecting the LV are usually recognized as electrocardiographic and echocardiographic LVH, which may be manifested clinically by angina pectoris, cardiac failure, silent ischemia, myocardial infarction and, of course, sudden death.
Measurement of serum PIIIP could therefore be a practical and useful tool in the non-invasive assessment of myocardial remodeling in hypertension. In particular, it may have clinical importance in documenting the extent of collagen accumulation and in evaluating pharmacological measures to prevent or even reverse this accumulation. Future mechanistic studies could examine whether pharmacologic agents that reduce circulating collagen biomarkers in hypertensive patients also reduce the degree of LVH in this population.
Changes in PIIIP concentrations may be a valuable tool to assess the ability of antihypertensive treatment to regress myocardial fibrosis in hypertensive patients.
Nevertheless, because of the limitations of this investigation, we are aware that further large studies are necessary to definitively validate this approach.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.