Although mortality after primary percutaneous coronary intervention (PPCI) is higher in women than in men, there is disagreement as to whether gender is an independent risk factor for mortality in ST-elevation myocardial infarction (STEMI). Our aim was to assess how gender influenced short-term prognosis in patients undergoing PPCI in the Portuguese Registry of Interventional Cardiology.
MethodsOf 60158 patients prospectively included in a large registry of contemporary PCI, from 2002 to 2012, we included 7544 patients with STEMI treated by PPCI, of whom 1856 (25%) were female. The effect of gender on in-hospital mortality was assessed by multivariate logistic regression analysis with propensity score matching.
ResultsWomen were older (68±14 vs. 61±13 years, p<0.001), with a higher prevalence of diabetes (30% vs. 21%, p<0.001) and hypertension (69% vs. 55%, p<0.001). Men were more frequently revascularized within six hours of symptom onset (71% vs. 63%, p<0.001). Cardiogenic shock was more frequent in women (7.1% vs. 5.7%, p=0.032). Female gender was associated with a worse short-term prognosis, with 1.7 times higher risk of in-hospital death (4.3% in women and 2.5% in men, 95% confidence interval (CI) 1.30–2.27, p<0.001). After computed propensity score matching based on baseline clinical characteristics, in-hospital mortality was similar between women and men (odds ratio 1.00, 95% CI 0.68–1.48, p=1.00).
ConclusionsIn the Registry, women with STEMI treated by PPCI had a greater risk-factor burden, less timely access to treatment and a worse prognosis. However, after risk adjustment, female gender ceases to be an independent predictor of in-hospital mortality.
A mortalidade na mulher após angioplastia primária (ICP-P) é superior à do homem. Contudo, permanece contraditório o papel do sexo poder ser fator de risco independente para mortalidade no contexto de enfarte agudo do miocárdio com supradesnivelamento de ST (EAMST). Com base no Registo Nacional de Cardiologia de Intervenção (RNCI), pretendemos avaliar como é que o género feminino influencia o prognóstico a curto prazo nos doentes com EAMST submetidos a ICP-P a nível nacional.
MétodosDe 60158 doentes incluídos prospetivamente no RNCI de 2002-2012, incluímos na análise 7544 doentes com EAMST tratados por ICP-P, dos quais 25% foram mulheres. Utilizámos modelos de regressão logística e ajustamento por propensity score para avaliar o impacto do sexo na mortalidade hospitalar.
ResultadosAs mulheres foram mais idosas (68±14 versus 61±13, p<0,001), mais diabéticas (30 versus 21%, p<0,001) e hipertensas (69 versus 55%, p<0,001). Os homens foram revascularizados mais cedo (71 versus 63% nas primeiras 6 horas, p<0,001). Choque cardiogénico foi mais frequente nas mulheres (7,1 versus 5,7%, p=0,032). Estas apresentaram um pior prognóstico a curto prazo, com 1,7 x maior risco de morte intra-hospitalar (4,3 versus 2,5%; IC 95% 1,30-2,27; p<0,001). Utilizando um modelo de regressão ajustado através de um propensity score, o sexo deixa de ser preditor de mortalidade hospitalar (OR 1,00; IC 95% 0,68-1,48; p=1,00).
ConclusõesNo RNCI as mulheres com EAMST tratadas com ICP-P apresentaram maior risco cardiovascular, um acesso menos atempado a ICP-P e um pior prognóstico. Contudo, após ajustamento do risco, o género feminino deixa de ser preditor independente de mortalidade hospitalar.
Cardiovascular disease remains the leading cause of mortality in women, and 23% of deaths among women in Europe are due to coronary artery disease (CAD).1 The proportion of women diagnosed with CAD has increased in recent years, but it is still underdiagnosed and undertreated compared to men, with less use of revascularization strategies and optimized medical therapy.2 Furthermore, the belief persists that women have worse prognosis than men following primary percutaneous coronary intervention (PPCI).3,4 Women's greater mortality may be explained by the fact that they have a higher cardiovascular risk and that CAD is underdiagnosed and undertreated in women, or be due to gender-related differences in anatomy and biological response to infarction.3 Previous registries have presented conflicting evidence as to whether female gender is an independent risk factor for mortality in ST-elevation myocardial infarction (STEMI).3–7
Our aim was to analyze the situation in Portugal regarding treatment of STEMI in women by PPCI based on the Portuguese Registry of Interventional Cardiology, and to assess how gender influenced in-hospital prognosis of these patients.
MethodsPopulationThe Portuguese interventional cardiology database is a prospective, observational registry of PCI in interventional cardiology units in Portugal. Between January 4, 2002 and July 24, 2012, 60158 patients were included from 22 centers. We retrospectively analyzed 7544 consecutive patients undergoing PPCI in the context of STEMI of less than 12 hours evolution. STEMI was defined as the presence of symptoms consistent with myocardial ischemia lasting more than 30 minutes and persistent ST elevation (>1 mm in two contiguous leads) or new-onset or previously undocumented complete left bundle branch block. Patients who underwent thrombolysis during the index hospitalization were excluded.
No exclusion criteria were applied in terms of the complexity of STEMI presentation or type of lesion.
All patients gave their informed consent for inclusion in the Registry.
Men and women were compared in terms of demographic characteristics, risk factors, previous cardiovascular history, disease severity, location of myocardial infarction (MI) and procedural characteristics.
Data on in-hospital clinical course were obtained from the Registry.
Statistical analysisThe male and female patient groups were analyzed according to continuous and categorical variables. Categorical variables were characterized in terms of absolute and relative frequencies. The central tendency and distribution of continuous variables were estimated by sample mean and standard deviation, or median and interquartile range, depending on whether values presented a normal distribution.
Categorical variables were compared using the chi-square test or Fisher's exact test as appropriate, while continuous variables were compared using the Student's t test, or the Mann–Whitney test when criteria for use of the former were not met. The Kolmogorov–Smirnov method was used to test the normality of distribution of continuous variables and Levene's test was used for equal variances.
The influence of each variable (including gender) on mortality was assessed in univariate analysis by means of odds ratios (OR) and 95% confidence intervals (CI). In the first regression model, only gender was considered an independent variable. The impact of gender on in-hospital mortality was subsequently adjusted for other variables, producing various logistic regression models. In the second model, the impact of gender was adjusted for age >65 years; in the third, it was adjusted for age, risk factors (diabetes, hypertension, dyslipidemia and smoking) and cardiovascular history (previous MI, percutaneous or surgical revascularization, congestive heart failure, stroke, peripheral arterial disease or chronic renal failure); in the fourth, clinical variables of severity at admission (cardiogenic shock and anterior MI) were added to all the variables included in the third model. Finally, the fifth model was adjusted for all the above variables, as well as procedural characteristics (type of access, type of stent and thrombectomy).
In order to minimize selection bias in this non-randomized study, a further logistic regression analysis was performed with gender as a dependent variable to determine a propensity score, which was then used to match men and women in a ratio of 1:1. The variables used to calculate the propensity score were age, risk factors and cardiovascular history. After matching the two sexes, the estimated risk of in-hospital death in women compared to men was again adjusted by means of a logistic regression model that included the same variables as in the fourth model described above.
When constructing all the above models to determine predictors of in-hospital death, gender was forced to enter the model by being included in the first block of variables, while the other predictors were selected from the second block of variables using the forward stepwise method. The Hosmer–Lemeshow test was used to assess the goodness of fit of the logistic regression models, while their discriminatory power was assessed by the area under the receiver operating characteristic (ROC) curve.
The statistical analysis was performed using SPSS, version 19.0.0.2. The level of significance was set at 5%.
ResultsBaseline characteristicsA total of 7544 consecutive patients from the Registry who underwent PPCI in the context of STEMI were included. The study population was divided into two groups according to gender: 1856 (25%) women and 5688 (75%) men. Demographic characteristics and clinical presentation at admission are shown in Table 1.
Demographic characteristics and clinical presentation.
| Women (n=1856) | Men (n=5688) | p | |
| Demographic | |||
| Age, years | 68±14 | 61±13 | <0.001 |
| Age > 65 years | 62.9 | 37.4 | <0.001 |
| CV risk factors | |||
| Diabetes | 29.6 | 20.6 | <0.001 |
| Dyslipidemia | 43.5 | 45.4 | 0.164 |
| Smoking | 21.6 | 57.3 | <0.001 |
| Hypertension | 68.8 | 54.8 | <0.001 |
| Previous CV history | |||
| MI | 10.7 | 15.3 | <0.001 |
| PCI | 10.9 | 15.9 | <0.001 |
| CABG | 0.9 | 1.9 | 0.008 |
| Stroke | 6.3 | 4.4 | 0.003 |
| PAD | 2.8 | 3.0 | 0.676 |
| CHF | 3.6 | 2.4 | 0.013 |
| CRF | 4.0 | 2.5 | 0.002 |
| Clinical presentation at admission | |||
| Cardiogenic shock | 7.1 | 5.7 | 0.032 |
| LV ejection fraction ≤40% | 19.1 | 17.1 | 0.225 |
Values presented as mean±standard deviation or relative frequency. CABG: coronary artery bypass grafting; CHF: congestive heart failure; CRF: chronic renal failure; CV: cardiovascular; LV: left ventricular; MI: myocardial infarction; PAD: peripheral arterial disease; PCI: percutaneous coronary intervention.
Women were older (68±14 vs. 61±13 years, p<0.001) and had a higher prevalence of diabetes (30% vs. 21%, p<0.001), hypertension (69% vs. 55%, p<0.001) and chronic renal failure (4% vs. 2%, p=0.002). On the other hand, they were less likely to smoke (22% vs. 57%, p<0.001) and less often had a history of coronary disease, including MI (11% vs. 15%, p<0.001), PCI (11% vs. 16%, p<0.001) or coronary artery bypass grafting (CABG) (1% vs. 2%, p=0.008).
The proportion of patients undergoing PPCI who went directly to a center with interventional cardiology facilities was greater among women (91% vs. 89%, p=0.014), but this did not influence door-to-balloon times, which were similar in both sexes (Table 2). Nevertheless, women were revascularized later than men (4.6 hours vs. 3.9 hours, p<0.001) as they arrived at hospital later (4.3 hours vs. 3.7 hours, p<0.001), and the percentage of men revascularized within six hours of symptom onset was higher than in women (71% vs. 63%, respectively, p<0.001).
Procedural characteristics.
| Women (n=1856) | Men (n=5688) | p | |
| Times (min) | |||
| Pain-to-balloon | 274 (175–482) | 237 (152–391) | <0.001 |
| Pain-to-door | 260 (160–452) | 223 (140–380) | <0.001 |
| Door-to-balloon | 24 (14–50) | 22 (14–47) | 0.472 |
| Form of admission | |||
| Direct to center with primary PCI | 90.6 | 88.5 | 0.014 |
| Transfer from another hospital | 9.4 | 11.5 | 0.014 |
| Infarct-related vessel | |||
| Left main | 0.9 | 1.0 | 0.657 |
| Anterior descending | 36.3 | 36.3 | 0.997 |
| Circumflex | 13.4 | 15.1 | 0.078 |
| Right coronary | 49.4 | 47.1 | 0.090 |
| Graft | 0.1 | 0.5 | 0.007 |
| Diseased vessels | |||
| Left main | 2.9 | 3.9 | 0.056 |
| Anterior descending | 71.6 | 68.1 | 0.006 |
| Circumflex | 39.6 | 43.6 | 0.004 |
| Right coronary | 55.1 | 56.9 | 0.192 |
| Multivessel disease (≥2 vessels) | 47.4 | 49.0 | 0.223 |
| Type of lesion | |||
| A | 9.3 | 9.2 | 0.906 |
| B | 34.5 | 33.9 | 0.694 |
| C | 56.3 | 56.9 | 0.657 |
| In-stent restenosis | 2.0 | 2.9 | 0.049 |
| Type of access | |||
| Femoral | 86.0 | 82.7 | <0.001 |
| Radial | 13.8 | 17.0 | 0.001 |
| Brachial | 0.2 | 0.2 | 1.000 |
| Stenting | 78.1 | 79.9 | 0.110 |
| Type of stent | |||
| DES | 44.4 | 46.8 | 0.105 |
| BMS | 55.1 | 52.9 | 0.141 |
| Thrombectomy | 22.7 | 26.2 | 0.003 |
| Glycoprotein IIb/IIIa inhibitor (abciximab) | 26.7 | 35.0 | <0.001 |
| Intra-aortic balloon pump | 3.8 | 3.0 | 0.122 |
| TIMI 3 flow at admission | 25.0 | 21.7 | 0.016 |
| Final TIMI 3 flow | 92.2 | 93.6 | 0.075 |
| Complete revascularization | 59.1 | 56.1 | 0.028 |
Values presented as median (P25-P75) or relative frequency. BMS: bare metal stent; DES: drug-eluting stent; P-PCI: primary percutaneous coronary intervention.
Cardiogenic shock was more common in women (7.1% vs. 5.7%, p=0.032). There were no significant differences in the infarct-related vessel or in the extent of coronary disease, the percentage of multivessel disease being similar in both sexes.
Procedural characteristicsProcedural characteristics are shown in Table 2. Femoral access was used most frequently in both groups, and radial access was used less often in women (14% vs. 17%, p=0.001). There was no difference in the type of stent employed, but thrombectomy (23% vs. 26%, p=0.003) and glycoprotein IIb/IIIa inhibitors (27% vs. 35%, p<0.001) were more often used in men. There was a tendency for final TIMI 3 flow to be more frequently achieved in men, reflecting a better angiographic result.
Predictors of in-hospital mortalityIn-hospital mortality was higher in women (4.3% vs. 2.5%, p<0.001), the risk of death being 1.7 times higher in women than men (95% CI 1.30–2.27; p<0.001) (Table 3).
Univariate predictors of in-hospital mortality.
| OR (95% CI) | p | |
| Demographic | ||
| Female gender | 1.72 (1.30–2.27) | <0.001 |
| Age > 65 years | 3.52 (2.62–4.73) | <0.001 |
| CV risk factors | ||
| Diabetes | 1.79 (1.33–2.41) | <0.001 |
| Dyslipidemia | 0.64 (0.48–0.87) | 0.004 |
| Smoking | 0.35 (0.26–0.49) | <0.001 |
| Previous CV history | ||
| Stroke | 1.86 (1.11–3.09) | 0.016 |
| PAD | 3.72 (2.27–6.12) | <0.001 |
| CHF | 5.22 (3.25–8.37) | <0.001 |
| CRF | 2.53 (1.41–4.53) | 0.001 |
| Clinical presentation at admission | ||
| Cardiogenic shock | 17.42 (13.13–23.12) | <0.001 |
| LV ejection fraction ≤40% | 14.81 (8.31–26.40) | <0.001 |
| Anterior MI | 2.01 (1.50–2.69) | <0.001 |
| Left main and/or multivessel disease | 1.48 (1.12–1.95) | 0.005 |
| Procedural characteristics | ||
| TIMI 3 flow at admission | 0.57 (0.35–0.93) | 0.024 |
| Final TIMI 3 flow | 0.14 (0.10–0.21) | <0.001 |
| Radial access | 0.24 (0.13–0.45) | <0.001 |
| BMS | 2.88 (1.98–4.18) | <0.001 |
| Thrombectomy | 0.70 (0.50–0.98) | 0.038 |
| Complete revascularization | 0.72 (0.55–0.96) | 0.023 |
BMS: bare metal stent; CHF: congestive heart failure; CI: confidence interval; CRF: chronic renal failure; CV: cardiovascular; LV: left ventricular; MI: myocardial infarction; OR: odds ratio; PAD: peripheral arterial disease.
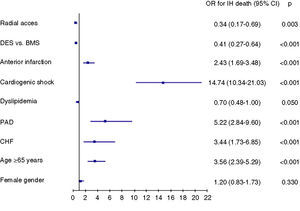
Adjustment for age >65 years revealed that this factor largely explained the increased risk in women compared to men (Table 4). On multivariate analysis (Figure 1), the independent predictors of in-hospital death were age >65 years, peripheral arterial disease, history of congestive heart failure, cardiogenic shock, and anterior MI. Dyslipidemia, use of drug-eluting stents and radial access were protective variables. The area under the ROC curve in the final model was 0.88, which reflects the excellent discriminatory power of the model.
In-hospital mortality in primary percutaneous coronary intervention according to gender.
| OR (95% CI) | p | Area under ROC curve | ||
| Model 1 | Unadjusted OR | 1.72 (1.30–2.27) | <0.001 | |
| Model 2 | OR adjusted for age >65 years | 1.31 (0.98–1.74) | 0.064 | 0.66 |
| Model 3 | OR adjusted for age and previous CV history | 1.07 (0.76–1.50) | 0.695 | 0.74 |
| Model 4 | OR adjusted for age, previous CV history and severity of clinical presentation | 1.09 (0.75–1.57) | 0.655 | 0.86 |
| Model 5 | OR adjusted for age, previous CV history, severity of clinical presentation and procedural characteristics | 1.20 (0.83–1.73) | 0.330 | 0.88 |
CI: confidence interval; CV: cardiovascular; OR: odds ratio; ROC: receiver operating characteristic. Previous CV history includes CV risk factors (diabetes, hypertension, dyslipidemia and smoking) and clinical history (previous myocardial infarction, percutaneous or surgical revascularization, congestive heart failure, stroke, peripheral arterial disease and chronic renal failure); severity of clinical presentation includes cardiogenic shock at admission and anterior myocardial infarction; procedural characteristics include radial access, type of stent and thrombectomy.
Based on a logistic regression model with gender as a dependent variable, a propensity score was calculated, which was then used to match 1338 women and 1338 men (a ratio of 1:1). Following this adjustment, in-hospital mortality was similar for both sexes, around 3.9% (OR 1.00, 95% CI 0.68–1.48, p=1.00).
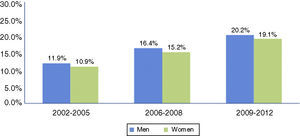
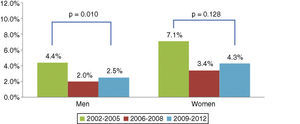
Changes in in-hospital mortality over the study periodThe percentage of women in the Registry undergoing PPCI has increased linearly over the years (11% in the period 2002–2005, 15% in 2006–2008, and 19% in 2009–2012; p<0.001 for trend), similar to the trend observed in men (Figure 2). Throughout the study period, in-hospital mortality among women was higher than in men, with a more marked difference in recent years (Table 5).
Although in-hospital mortality rates decreased in absolute terms in both sexes between 2002 and 2012, the reduction was only significant in men (Figure 3).
DiscussionClinical and angiographic characteristicsAs seen in many other studies on coronary revascularization, both surgical and percutaneous, clinical presentation of coronary disease differs between the sexes.3–6,8,9 Women tend to present acute coronary syndrome at older ages, on average a decade later, and more often have atypical symptoms rather than classic angina. They also have a worse cardiovascular profile, with a higher prevalence of diabetes and hypertension, and the presence of multiple cardiovascular risk factors is common among post-menopausal women.
Despite the higher risk profile of women undergoing PPCI, disease severity is similar to that of men, with a similar prevalence of multivessel disease.9
The incidence of congestive heart failure and cardiogenic shock at admission is significantly higher in women, despite the fact that they less often have previous MI and present similar left ventricular function to men, as observed in numerous other studies.3,4,9 The most frequently suggested explanation is the greater prevalence of diastolic dysfunction due to older age and hypertensive heart disease.10 Hypertrophied myocardium may be more vulnerable in situations of transient ischemia, the decreased diastolic compliance that occurs following sudden occlusion of a vessel being less well tolerated in patients with a preexisting “stiff” ventricle.10 On the other hand, the higher incidence of hemodynamic instability at admission may be explained by the fact that women arrive in the catheterization laboratory after a longer delay from symptom onset.3 The time to mechanical reperfusion is thus longer in women due to longer pain-to-door times.3,4,11 In the 1950s and 1960s, coronary disease was seen as a disease of men, but from the 1970s onward there was an increase in coronary disease among women, which was attributed to changes in their lifestyle, with increased prevalence of smoking, use of oral contraceptives and increasing numbers of women in employment.12 This, together with the fact that cardiovascular disease is still the leading cause of death in women,1 highlights the importance of implementing measures to raise awareness among women of the symptoms of MI and of the need to seek immediate medical attention. The longer delay between symptom onset and mechanical reperfusion is one of the modifiable predictors of a worse prognosis.
Procedural characteristicsThere are also gender-based differences in procedural characteristics. Coronary arteries in women are of smaller diameter and this may influence the type of material used, notably reducing the use of stents.1 However, this was not the case in our study, in which stenting and types of stent were similar in both sexes. The reduction in restenosis observed with widespread use of drug-eluting stents appears to be similar in men and women.13 Smaller caliber arteries, together with a greater tendency for arterial vasospasm, may explain the less frequent use of radial access in women. PCI success rates are similar in both sexes,14 as is the use of new antithrombotic drugs.15 Nevertheless, glycoprotein IIb/IIIa inhibitors are far less often administered in women as adjuvant therapy to antithrombins in primary angioplasty. This may be because women undergoing PCI present more bleeding and vascular complications than men.16,17 A subanalysis of the ACUITY trial showed that women have more bleeding complications at 30 days compared to men, but with no differences in short- or long-term mortality. Women treated with bivalirudin have fewer bleeding complications compared to those receiving heparin together with glycoprotein IIb/IIIa inhibitors, but with no difference in ischemic events.18
Evidence shows that there are still gender-based differences in treatment of coronary disease, with women presenting STEMI and age >65 years less often receiving reperfusion therapy.1 In Portugal, there has been a progressive increase in recent years in women undergoing PPCI, with reduced in-hospital mortality for STEMI between 2002 and 2012 (in both sexes). However, despite these advances in STEMI treatment, unadjusted in-hospital mortality remains higher in women, which highlights the need for strategies to improve risk stratification, diagnosis and treatment of cardiovascular disease in women.
In-hospital mortalityThis analysis of the PCI Registry revealed that in Portugal female gender is not an independent predictor of in-hospital mortality in MI treated by PPCI. In our non-adjusted model, women had worse prognosis than men, but as in previous studies,5–7,19,20 after adjustment for comorbidities and other adverse factors, female gender ceased to be an independent predictor of unfavorable outcome after PCI. This finding was repeated in multivariate logistic regression analysis, as well as when adjusted to the propensity score.
In the thrombolytic era, in-hospital survival among women was consistently lower than that of men,21,22 with more associated fatal bleeding complications.19 In a multicenter study of 395 patients (27% female) with STEMI that compared PPCI with thrombolysis, primary angioplasty was an independent predictor of survival in women.19 In a substudy of the randomized GUSTO II-B trial, both sexes showed benefits from direct angioplasty compared to thrombolysis, with fewer major adverse events at 30 days, but the absolute benefit was greater in women (direct angioplasty prevented 56 events/1000 women vs. 42 events/1000 men).20 The introduction of primary angioplasty as the treatment of choice for STEMI, progressive improvements in PCI techniques and success rates, and advances in adjuvant antiplatelet and anticoagulant therapy, may all explain the differences observed between earlier and later studies. Nevertheless, the results of recent studies assessing gender differences in primary angioplasty are in disagreement with the present study, reporting female gender as an independent predictor of worse short-term prognosis, irrespective of age and baseline cardiovascular risk factors.3,4 Earlier studies suggested that pathophysiological differences between the sexes may contribute to higher mortality in women with STEMI. Estrogens, which protect women against coronary atherosclerosis,23 could make vulnerable plaques less stenotic.24 Women would therefore have less collateral circulation and less ability to develop preconditioning in STEMI, worsening their prognosis.25,26 However, this would only explain the differences observed in younger, premenopausal women. On the other hand, the present analysis of the Registry was of a larger sample (>7000 treated by PPCI) than in previous studies3,4 and included data from multiple centers, and thus reflects the situation in the country as a whole rather than of a single center; the statistical methodology used was also superior, including a propensity score; and the data presented are more up-to-date, with lower in-hospital mortality in both men and women. In a recently published risk-adjusted analysis of 13752 patients (34.6% women), Kovacic et al. confirmed that female gender was not an independent predictor of mortality after PCI in the drug-eluting stent era,27 which supports the findings of our study.
LimitationsThe present study was observational, unblinded and non-randomized, and may therefore be subject to confounding factors that were not recognized or taken into account in the risk-adjusted analysis. The fact that no data were included on bleeding events, a known independent risk factor for mortality, is another limitation. No information was available on use of in-hospital medication, notably antiplatelets (except glycoprotein IIb/IIIa inhibitors) and adjuvant anticoagulation therapy, and thus the possibility of differences between the sexes in administration of these drugs cannot be excluded.
ConclusionIn this sample from the Portuguese Registry of Interventional Cardiology, women with STEMI treated by PPCI had a higher risk profile, less timely access to treatment and a worse prognosis. However, after risk adjustment, female gender ceased to be an independent predictor of in-hospital mortality.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors thank the Portuguese National Cardiology Data Collection Center (CNCDC), particularly Dr. Adriana Belo, for their help in the statistical treatment of the data.
Sociedade Portuguesa de Cardiologia.
Please cite this article as: Calé R, de Sousa L, Pereira H, Costa M, de Sousa Almeida M, em nome dos Investigadores do Registo Nacional de Cardiologia de Intervenção. Angioplastia primária na mulher: realidade nacional. Rev Port Cardiol. 2014;33:353–361.