The aim of this study was to assess the change in the theoretical probability of coronary artery disease (CAD) in patients with suspected CAD undergoing coronary computed tomographic angiography as the first-line test compared to CCTA after an exercise ECG.
MethodsPre- and post-test probabilities of CAD were assessed in 158 patients with suspected CAD undergoing dual-source CCTA as the first-line test (Group A) and in 134 in whom CCTA was performed after an exercise ECG (Group B). Pre-test probabilities were calculated based on age, gender and type of chest pain. Post-test probabilities were calculated according to Bayes’ theorem.
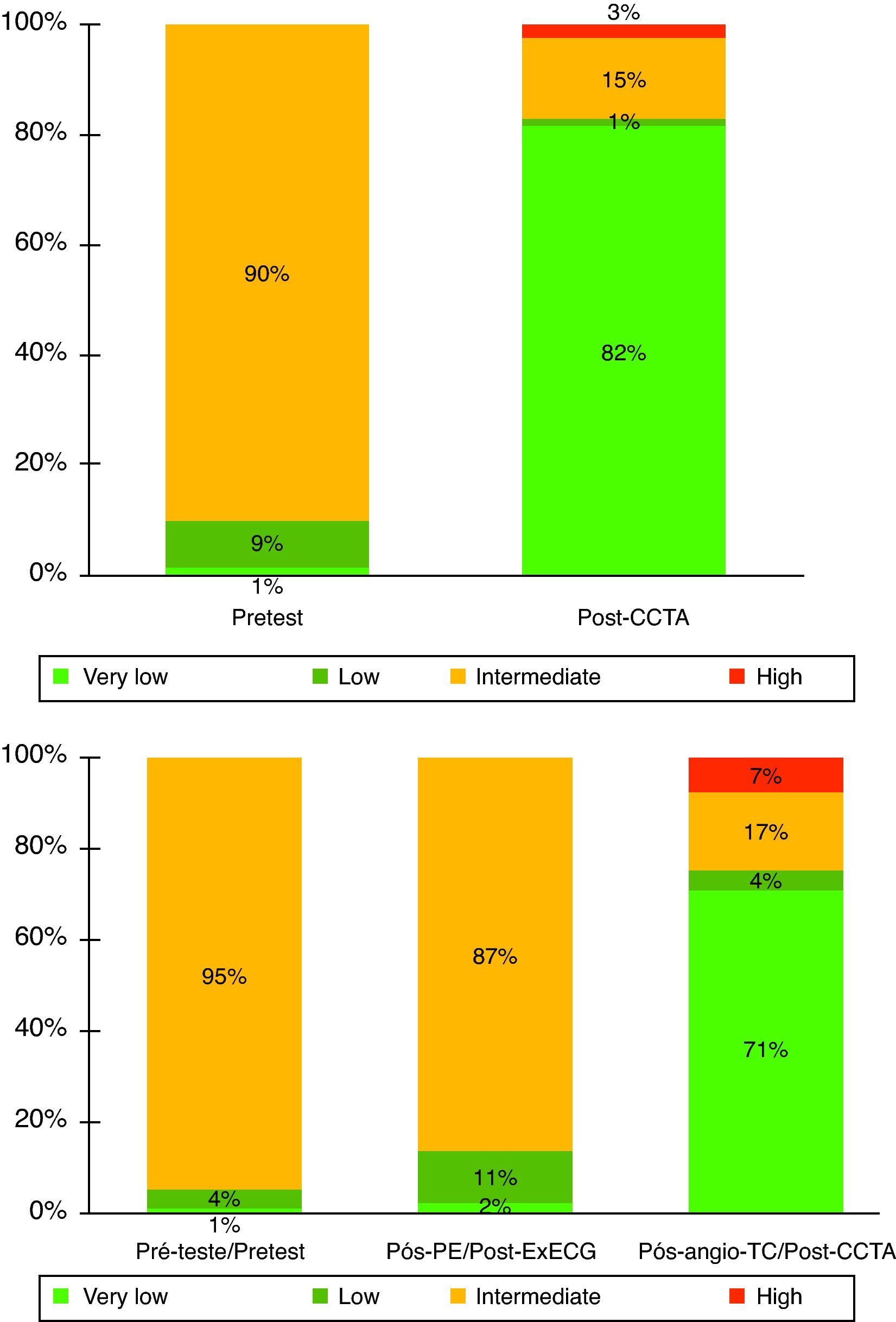
ResultsThere were no significant differences between the groups regarding pre-test probability (median 23.5% [13.3–37.8] in group A vs. 20.5% [13.4–34.5] in group B; p=0.479). In group A, the percentage of patients with intermediate likelihood of disease (10–90%) was 90% before testing and 15% after CCTA (p<0.001), while in group B, it was 95% before testing, 87% after exercise ECG (p=NS), and 17% after CCTA (p<0.001).
ConclusionUnlike exercise testing, CCTA is able to reclassify risk in the majority of patients with an intermediate likelihood of obstructive CAD. The use of CCTA as the first-line diagnostic test for CAD may be advantageous in this setting.
A prova de esforço (PE) continua a ser o exame de 1.ª linha no diagnóstico de doença coronária (DC), mas por vezes a angio-TC é já o primeiro estudo solicitado. O objetivo deste estudo foi avaliar a evolução da probabilidade teórica de DC obstrutiva em doentes que efetuaram angio-TC cardíaca como exame de 1.ª linha versus doentes submetidos a angio-TC após PE.
MétodosDe um registo prospetivo de angio-TC cardíaca, selecionámos 292 doentes avaliados por suspeita de DC, dos quais 158 efetuaram AngioTC como exame de 1.ª linha (Grupo A) e 134 após PE (Grupo B). Em cada doente, a probabilidade pré-teste de DC obstrutiva foi estimada com base no sexo, idade e sintomatologia. As probabilidades pós-teste foram calculadas de acordo com o teorema de Bayes.
ResultadosNão se registaram diferenças significativas entre os dois grupos quanto à probabilidade pré-teste inicial (mediana 23,5% [13,3-37,8] no grupo A versus 20,5% [13,4-34,5] no grupo B; p=0,479). No grupo A, a percentagem de doentes com probabilidade intermédia (10-90%) foi de 90% antes do exame, e de 15% após a Angio-TC (p<0,001). No grupo B, a percentagem de doentes com probabilidade intermédia foi de 95% antes dos exames, de 87% após a PE (p=NS), e de 17% após a Angio-TC (p<0,001).
ConclusãoAo contrário da PE, a angio-TC permite reclassificar o risco na maioria dos doentes que apresentam probabilidade intermédia de DC obstrutiva. O uso da angio-TC como exame diagnóstico de primeira linha poderá ser vantajoso neste contexto.
Clinical assessment of patients with suspected stable coronary artery disease (CAD) often includes non-invasive exams. An exercise ECG is usually the first-line exam in this context,1 complemented by other functional tests such as stress echocardiography (SE) and myocardial perfusion scintigraphy (MPS). In recent years, coronary computed tomographic angiography (CCTA) has been increasingly used as a valid alternative in patients with intermediate or low pre-test probability2 and in some cases it is now the first exam requested. The value of any diagnostic test depends on how the result changes the patient's pre-test probability, ideally either increasing it to a level that justifies invasive coronary angiography or reducing it to a level where the diagnosis can be excluded. The aim of this study was to assess the change in the theoretical probability of obstructive CAD in patients undergoing CCTA as the first-line exam compared to CCTA after an exercise ECG.
MethodsFrom a prospective registry of 575 patients who underwent CCTA at Hospital dos Lusíadas between January 2009 and April 2011, we selected those for whom the indication was clinical suspicion of CAD. Asymptomatic patients and those with documented CAD, particularly those with a history of acute coronary syndrome, myocardial revascularization or coronary stenosis ≥50% on previous invasive coronary angiography, were excluded. Patients who had been referred following imaging studies of myocardial ischemia (SE or MPS) were also excluded. The 292 patients included in the analysis were divided into two groups according to the diagnostic approach: CCTA as the first-line exam (group A) or an exercise ECG followed by CCTA (group B).
Pre-test probabilityThe pre-test probability of obstructive CAD was determined for each patient using the predictive model of Genders et al.,3 who updated and extended the previous model of Diamond and Forrester.4 The variables considered in the latest model are age, gender and symptoms (classified as typical chest pain, atypical chest pain or non-specific chest pain). The probability function, estimated by the logistic regression model used, is expressed as: f(z)=1/(1+e−z), in which z represents the contribution of each of the variables involved and is equal to −4.37+0.04×age (in years)+1.34 (in men)+1.9 in the case of typical angina or 0.64 in the case of atypical angina.
Exercise ECGPatients in group B underwent CCTA after an exercise ECG performed in the previous six months. The exercise ECGs were performed and interpreted by the respective attending physicians, and the results were classified as positive, negative, inconclusive or doubtful based on the information in the reports in the possession of the patients and/or the clinical data on the referral for CCTA.
Coronary computed tomographic angiographyAll patients underwent CCTA on a 64-slice dual-source scanner (Siemens SOMATOM® Definition, Forchheim, Germany) following administration of 5mg sublingual nitroglycerin. Beta-blockers were administered in 72% of cases and prospective ECG triggering was used in 44% of patients. The median total dose of radiation was 280mGycm (171–577). Acquisition without contrast was performed immediately prior to CCTA in all cases in order to calculate the Agatston calcium score. The decision to include patients with Agatston scores above 400 was made on a case-by-case basis, since in our institution this is considered a relative contraindication for CCTA. Three-dimensional reconstruction and analysis of the CCTA images were performed on a workstation (TeraRecon®, California, USA), using multiplanar reconstructions, maximum intensity projections and vessel cross-sections, as appropriate. Anatomically obstructive CAD was defined as at least one ≥50% stenosis in an epicardial vessel.
Post-test probabilityThe post-test probability was calculated for each patient using Bayes’ theorem, according to the equation: P(A|B)=[P(B|A)×P(A)]/P(B), in which P (A|B) is the post-test probability conditioned by the pre-test probability [P(A)] and P(B) is the probability determined by the test used.5,6
A sensitivity of 98% and specificity of 85% were assumed for CCTA based on the results of the latest published meta-analysis.7 For exercise ECGs, a sensitivity and specificity of 68% and 77%, respectively, were assumed.1
In patients with inconclusive exercise ECG, the post-test probability assigned was the same as the pre-test probability estimated as described above. Similarly, in patients in whom CCTA did not show the presence of obstructive plaques but in whom one or more segments were not assessed due to artefacts, the post-test probability assigned was the same as the pre-test probability.
The groups were compared using the Student's t test or Mann–Whitney test for continuous variables and Fisher's exact test for categorical variables. The results for continuous variables with symmetric and asymmetric distribution are presented as means±standard deviation and medians and interquartile range, respectively. The statistical analysis was performed using SPSS version 17.0.
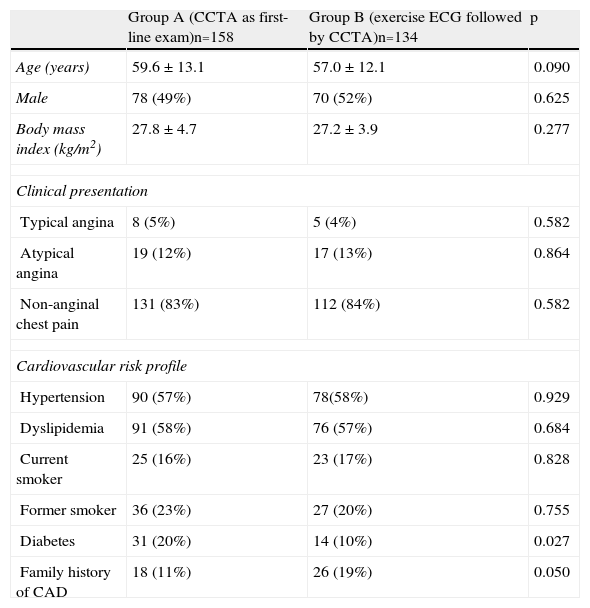
ResultsThere were no statistically significant differences between the two groups in demographic variables, clinical presentation or cardiovascular risk profile (Table 1), with the exception of diabetes, which was more common in group B (20% vs. 10%, p=0.027), and a family history of premature CAD, which was more common in group A (19% vs. 11%, p=0.050).
Baseline characteristics of the study groups.
| Group A (CCTA as first-line exam)n=158 | Group B (exercise ECG followed by CCTA)n=134 | p | |
| Age (years) | 59.6±13.1 | 57.0±12.1 | 0.090 |
| Male | 78 (49%) | 70 (52%) | 0.625 |
| Body mass index (kg/m2) | 27.8±4.7 | 27.2±3.9 | 0.277 |
| Clinical presentation | |||
| Typical angina | 8 (5%) | 5 (4%) | 0.582 |
| Atypical angina | 19 (12%) | 17 (13%) | 0.864 |
| Non-anginal chest pain | 131 (83%) | 112 (84%) | 0.582 |
| Cardiovascular risk profile | |||
| Hypertension | 90 (57%) | 78(58%) | 0.929 |
| Dyslipidemia | 91 (58%) | 76 (57%) | 0.684 |
| Current smoker | 25 (16%) | 23 (17%) | 0.828 |
| Former smoker | 36 (23%) | 27 (20%) | 0.755 |
| Diabetes | 31 (20%) | 14 (10%) | 0.027 |
| Family history of CAD | 18 (11%) | 26 (19%) | 0.050 |
CAD: coronary artery disease; CCTA: coronary computed tomographic angiography.
The median Agatston calcium score was 0.8 (0.0–93.5), with only 6% of patients presenting scores >400.
The median pre-test probability of obstructive CAD was 23% (13–36%), with no significant difference between the groups (p=0.479).
Of the 134 patients who underwent exercise ECG, 68 (51%) had a positive test, of whom 60 had ECG criteria only, six had angina during the test, and two had both angina and ECG alterations. The exercise ECG was classified as negative for myocardial ischemia in 36 patients (27%), doubtful in 10 (7%) and inconclusive in 20 (15%).
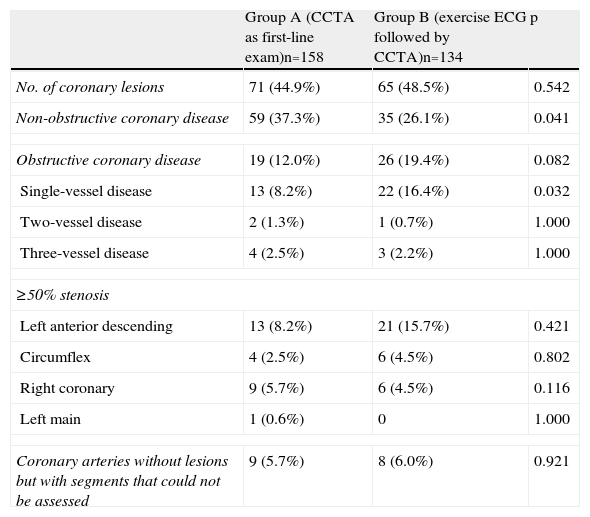
Nineteen patients (12%) in group A and 26 (19%) in group B presented obstructive CAD on CCTA (p=0.082). CCTA findings in the overall study population are shown in Table 2. The percentage of patients in group B who presented obstructive CAD on CCTA was 22% among those with positive exercise ECG, and 14% among those with negative exercise ECG.
Findings by coronary computed tomographic angiography in groups A and B.
| Group A (CCTA as first-line exam)n=158 | Group B (exercise ECG followed by CCTA)n=134 | p | |
| No. of coronary lesions | 71 (44.9%) | 65 (48.5%) | 0.542 |
| Non-obstructive coronary disease | 59 (37.3%) | 35 (26.1%) | 0.041 |
| Obstructive coronary disease | 19 (12.0%) | 26 (19.4%) | 0.082 |
| Single-vessel disease | 13 (8.2%) | 22 (16.4%) | 0.032 |
| Two-vessel disease | 2 (1.3%) | 1 (0.7%) | 1.000 |
| Three-vessel disease | 4 (2.5%) | 3 (2.2%) | 1.000 |
| ≥50% stenosis | |||
| Left anterior descending | 13 (8.2%) | 21 (15.7%) | 0.421 |
| Circumflex | 4 (2.5%) | 6 (4.5%) | 0.802 |
| Right coronary | 9 (5.7%) | 6 (4.5%) | 0.116 |
| Left main | 1 (0.6%) | 0 | 1.000 |
| Coronary arteries without lesions but with segments that could not be assessed | 9 (5.7%) | 8 (6.0%) | 0.921 |
CCTA: coronary computed tomographic angiography.
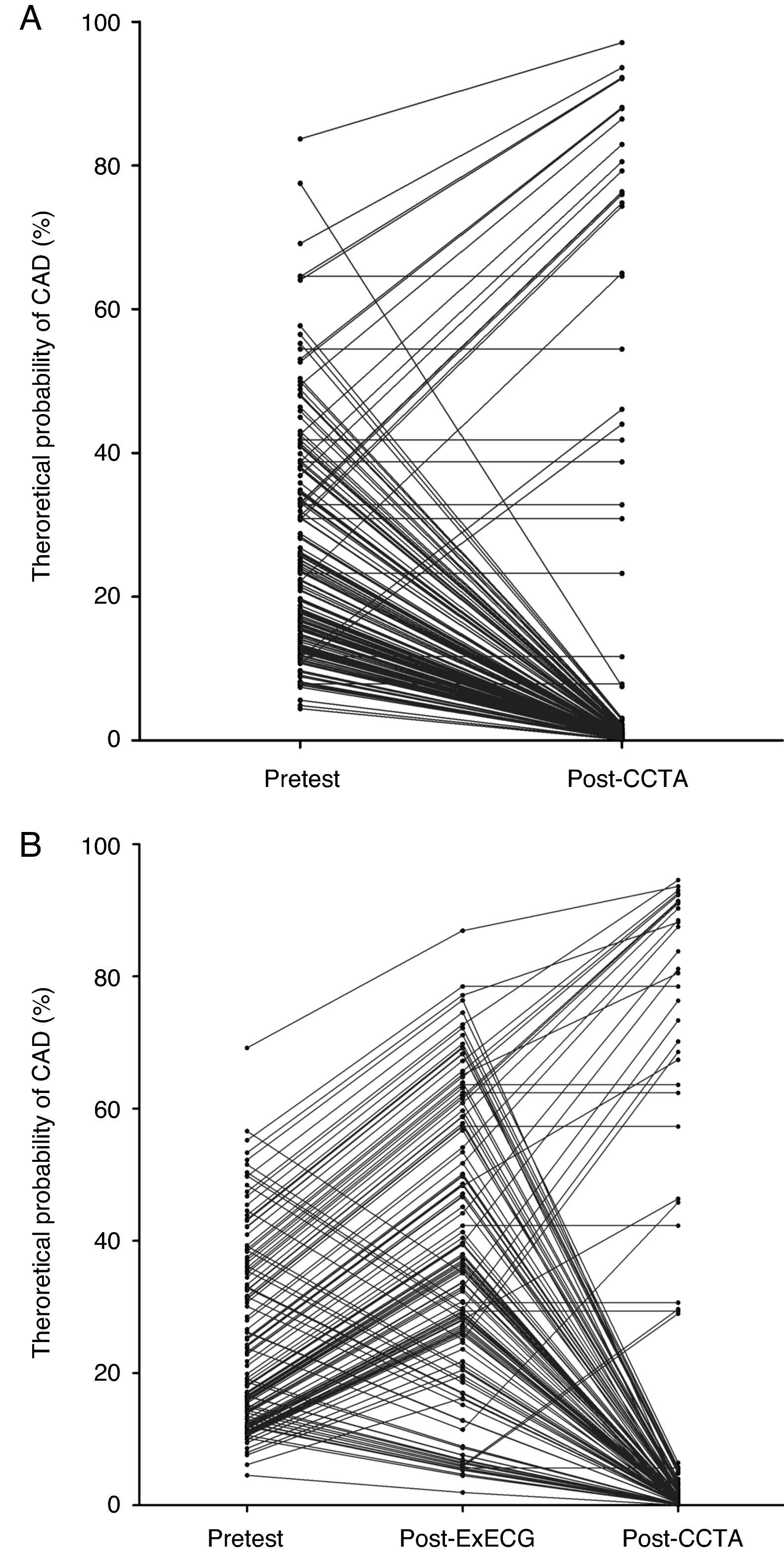
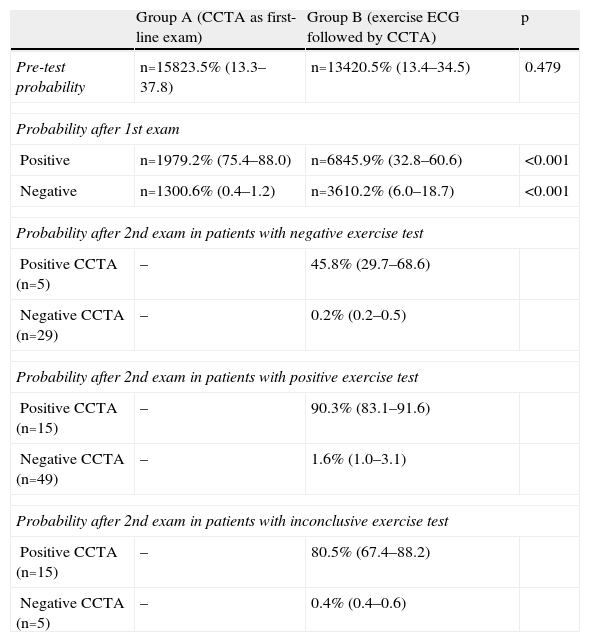
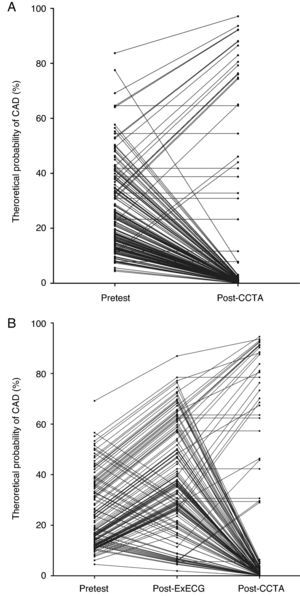
The theoretical probability of CAD in groups A and B at each diagnostic stage is shown in Table 3. The change in the probability of CAD for each individual in groups A and B during the diagnostic process is shown in Figure 1.
Change in theoretical probability of obstructive coronary artery disease in groups A and B.
| Group A (CCTA as first-line exam) | Group B (exercise ECG followed by CCTA) | p | |
| Pre-test probability | n=15823.5% (13.3–37.8) | n=13420.5% (13.4–34.5) | 0.479 |
| Probability after 1st exam | |||
| Positive | n=1979.2% (75.4–88.0) | n=6845.9% (32.8–60.6) | <0.001 |
| Negative | n=1300.6% (0.4–1.2) | n=3610.2% (6.0–18.7) | <0.001 |
| Probability after 2nd exam in patients with negative exercise test | |||
| Positive CCTA (n=5) | – | 45.8% (29.7–68.6) | |
| Negative CCTA (n=29) | – | 0.2% (0.2–0.5) | |
| Probability after 2nd exam in patients with positive exercise test | |||
| Positive CCTA (n=15) | – | 90.3% (83.1–91.6) | |
| Negative CCTA (n=49) | – | 1.6% (1.0–3.1) | |
| Probability after 2nd exam in patients with inconclusive exercise test | |||
| Positive CCTA (n=15) | – | 80.5% (67.4–88.2) | |
| Negative CCTA (n=5) | – | 0.4% (0.4–0.6) | |
CCTA: coronary computed tomography angiography.
With CAD probability classified as very low (<5%), low (5–9%), intermediate (10–90%) or high (>90%), it was found that:
- -
in group A, 84% (119/142) of patients with intermediate probability initially were reclassified in other categories;
- -
in group B, only 13% (17/127) of patients with intermediate probability were reclassified after exercise ECG, 15 being reclassified as low probability and two as very low probability. Following CCTA in this group, 82% (94/115) of patients with intermediate probability after exercise ECG were reclassified (Figures 2 and 3).
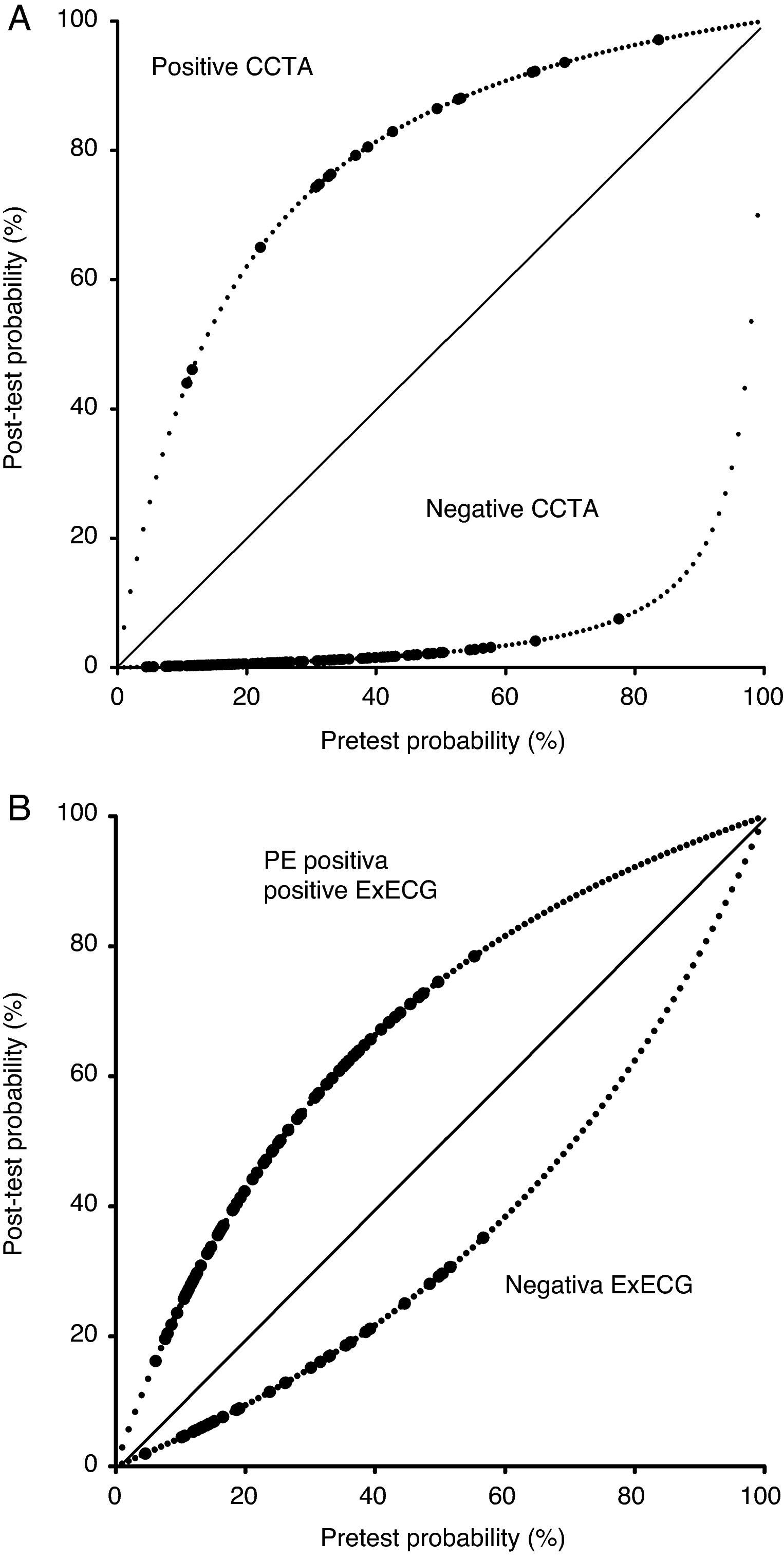
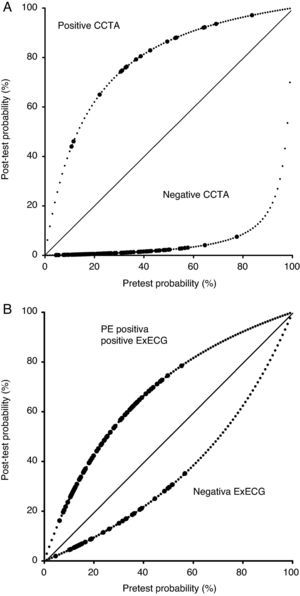
Figure 3.(A and B) Change in theoretical probability of obstructive coronary artery disease in the two study groups according to Bayes’ theorem. The dashed line represents the negative or positive likelihood ratio, based on the sensitivity and specificity considered for each test. The filled circles represent the post-test probability of each patient in groups A and B. CCTA: coronary computed tomographic angiography; ExECG: exercise ECG.
The approach to patients with suspected CAD invariably involves a qualitative or quantitative estimate of the likelihood of disease based on symptoms and cardiovascular risk factors. Current guidelines for the management of these patients recommend that those with high probability be referred directly for invasive coronary angiography, while non-invasive tests are indicated in those with intermediate probability.8,9 According to Bayes’ theorem, these exams will change the probability of CAD, ideally either increasing it to a level that justifies invasive coronary angiography or reducing it to a level where the diagnosis can be excluded. Based on the sensitivity and specificity of exercise ECG and CCTA reported in meta-analyses, our aim was to assess the change in the theoretical probability of obstructive CAD when these exams were performed in specific patients. It should be pointed out that this was not a study of diagnostic accuracy and that, given the absence of a gold standard exam, no exam can be assumed to be better than another if their results conflict. Nevertheless, the results of this analysis suggest that CCTA reclassifies the majority of patients with intermediate probability into lower or higher categories, while exercise ECG reclassifies a small proportion of patients only, most remaining at intermediate levels.
It is interesting that in our study population the number of CCTAs requested as the first-line exam was slightly higher than the number requested following an exercise ECG, and that in the latter case, they were requested as often for patients with positive exercise ECG as for those with a negative test. It should also be noted that the pre-test probability was relatively low in both groups, suggesting a generally appropriate use of CCTA on the part of referring physicians. In addition, the prevalence of obstructive CAD as assessed by CCTA was slightly lower than that estimated by the pre-test probability, which is in agreement with recent data indicating that clinical methods tend to overestimate prevalence.10
The choice of a first-line exam should be based on its advantages and disadvantages in terms of diagnostic accuracy, accessibility, cost and contraindications. Exercise ECG is accessible and inexpensive, which makes it the most commonly requested non-invasive test for patients with suspected CAD. However, its limited sensitivity and specificity lead to suboptimal performance in many cases,11 which can raise indirect costs: inconclusive tests generally necessitate additional exams, which increases the overall cost of the diagnostic strategy; false negative results can delay or prevent correct diagnosis, while false positive results frequently require more complex and costly non-invasive exams or result in unnecessary diagnostic catheterization, which entails risks and potentially avoidable costs. The extent of the latter problem is illustrated by the results of a large American registry, in which 62% of 398978 individuals referred for diagnostic invasive coronary angiography did not present obstructive CAD.9 In Portugal, recent data from a large-volume center showed that 43% of 1892 patients undergoing diagnostic coronary angiography for suspected CAD over a five-year period did not have obstructive CAD, and of these two-fifths had been referred following a positive exercise test.12 Wider use of CCTA, when used appropriately, could help to minimize this problem, since it appears to help reduce the number of invasive procedures.13
One advantage of exercise testing is that it provides information on a patient's functional capacity, an important factor in prognosis.14 However, CCTA also provides prognostic information and can detect non-obstructive CAD, which is not assessed by functional tests such as an exercise ECG.15,16 A recent head-to-head comparison suggests that CCTA has greater prognostic value than exercise testing.17
CCTA is not without disadvantages and limitations. The fact that it is less accessible and more costly, and employs ionizing radiation and iodinated contrast, limits its use in clinical practice. In particular, its cost-effectiveness has been the subject of investigation. When compared with the standard functional tests (exercise testing, SE and MPS), CCTA has been shown to be cost-effective,18 especially when pre-test probability is ≤50%.19 It should also be borne in mind that a significant percentage of patients undergoing CCTA (particularly those with an intermediate degree of stenosis) will subsequently require ischemia testing if unnecessary invasive coronary angiography and/or angioplasty are to be avoided. CCTA may soon be able to assess ischemia through perfusion imaging20,21 or computation of coronary fractional flow reserve,22 but this application is not yet established. With regard to the other limitations mentioned above, the availability of the technique has increased considerably in recent years, as have efforts to reduce the radiation to which patients are exposed; exams are now performed with lower effective radiation doses than for MPS and even for invasive coronary angiography.23–26
The results of our study thus support the latest clinical guidelines for the diagnosis of stable CAD of the UK National Institute for Health and Clinical Excellence (NICE), which advise against the use of exercise testing in this context after analyzing the diagnostic performance and cost-effectiveness of each modality.27 The same guidelines propose CCTA as the first-line exam in patients with a pre-test probability of 10–29%, ischemia imaging for those with a pre-test probability of 30–60%, and direct referral for invasive coronary angiography in those with a pre-test probability of >60%. Various ongoing studies, including PROMISE (PROspective Imaging Study for Evaluation of Chest Pain) and CRESCENT (Computed Tomography versus Exercise Testing in Suspected Coronary Artery Disease), may increase our understanding of the relative advantages and disadvantage of CCTA as the first-line exam in the diagnosis of CAD.
Our study has certain limitations. Firstly, it was essentially a theoretical exercise, the results of which are dependent on certain assumptions, particularly in terms of the sensitivity and specificity of the two techniques assessed, which may be different in the real world from those reported in studies performed in international reference centers.28 Since not all patients underwent invasive coronary angiography, it was not possible to assess the true sensitivity and specificity of each of the tests in this population. Secondly, the sample may not have been representative of all patients with suspected CAD, since those with typical symptoms or clearly positive exercise tests were probably referred directly for conventional coronary angiography. In addition, while the CCTA exams were interpreted in the same center by the same operators in all cases, the exercise ECGs were interpreted by the physicians who performed them and/or by the respective attending physicians, and there was thus no way to ensure the consistency of the criteria used. It should also be borne in mind that functional and anatomical findings do not necessarily correlate closely,29 which may partly explain the discrepancy observed in the study's results. Lastly, only ST-segment alterations and the occurrence of chest pain during exercise testing were considered diagnostic criteria, and conclusive tests were classified as positive or negative, which is a simplification but is virtually inevitable in this type of analysis. However, while scores such as the Duke score have recognized prognostic value, their diagnostic accuracy is still far inferior to CCTA, with sensitivity and specificity of 75% and 50%, respectively.30
ConclusionUnlike exercise testing, CCTA as the first-line diagnostic exam is able to reclassify risk in the majority of patients with an intermediate likelihood of obstructive CAD on clinical criteria. The use of CCTA as the initial exam may be advantageous in this setting.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Faria Alves M, et al. Probabilidade teórica de doença coronária pré- e pós-teste em duas estratégias diagnósticas – Contributo relativo da prova de esforço e da angio-Tc cardíaca. Rev Port Cardiol. 2013. http://dx.doi.org/10.1016/j.repc.2012.06.009.