Natriuretic peptides are ubiquitously used for diagnosis, follow-up and prognostic assessment in various heart conditions. N-terminal pro-brain natriuretic peptide (NT-proBNP) correlates with aortic stenosis severity, however its significance after transcatheter aortic valve implantation (TAVI) is not well established.
AimWe aimed to assess the prognostic value of NT-proBNP at one year in patients undergoing TAVI.
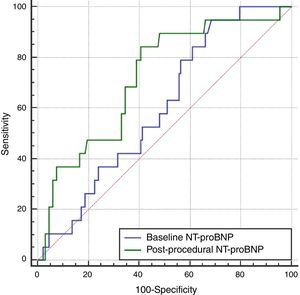
MethodsThis single-center retrospective analysis included 151 patients in whom both baseline and one-month post-procedure NT-proBNP were measured, from 206 consecutive patients undergoing TAVI between November 2008 and December 2014. The best cut-off values of both baseline and one-month post-TAVI NT-proBNP for one-year mortality were determined by receiver operating characteristic curve analysis. Independent predictors of one-year mortality were assessed by Cox regression.
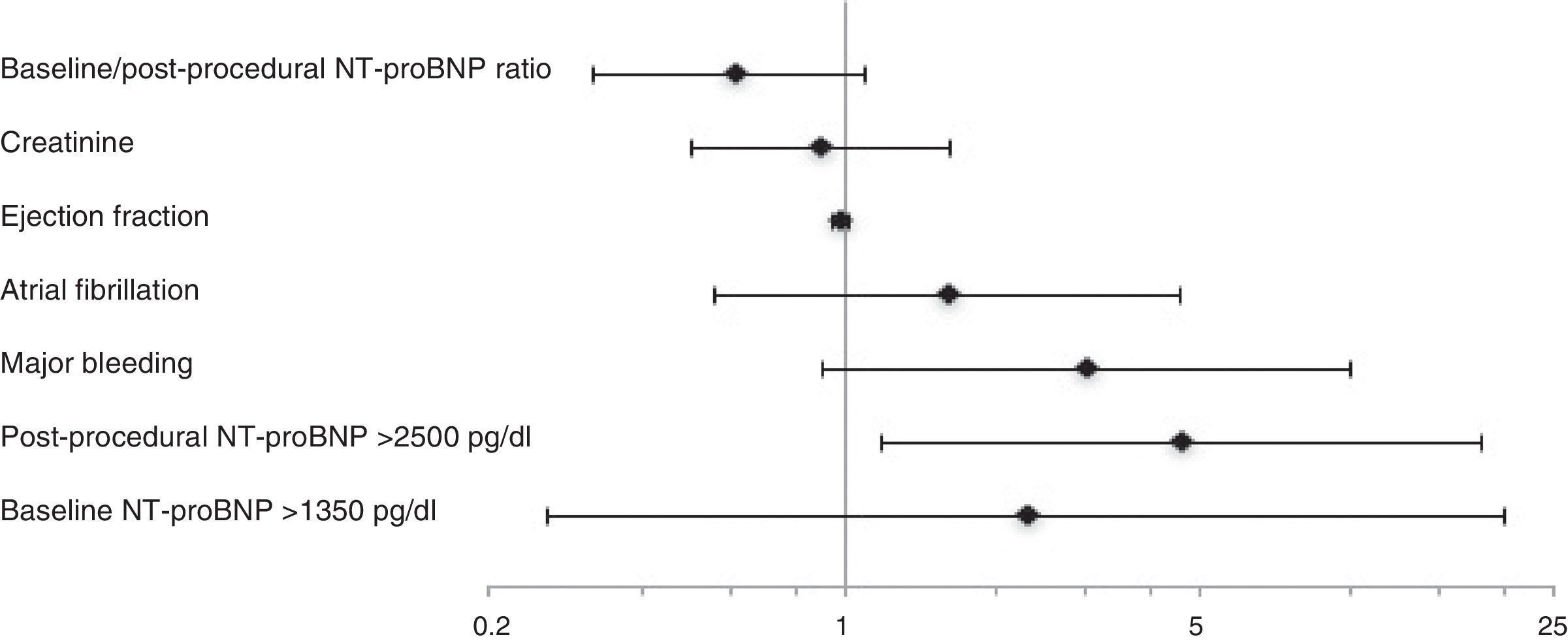
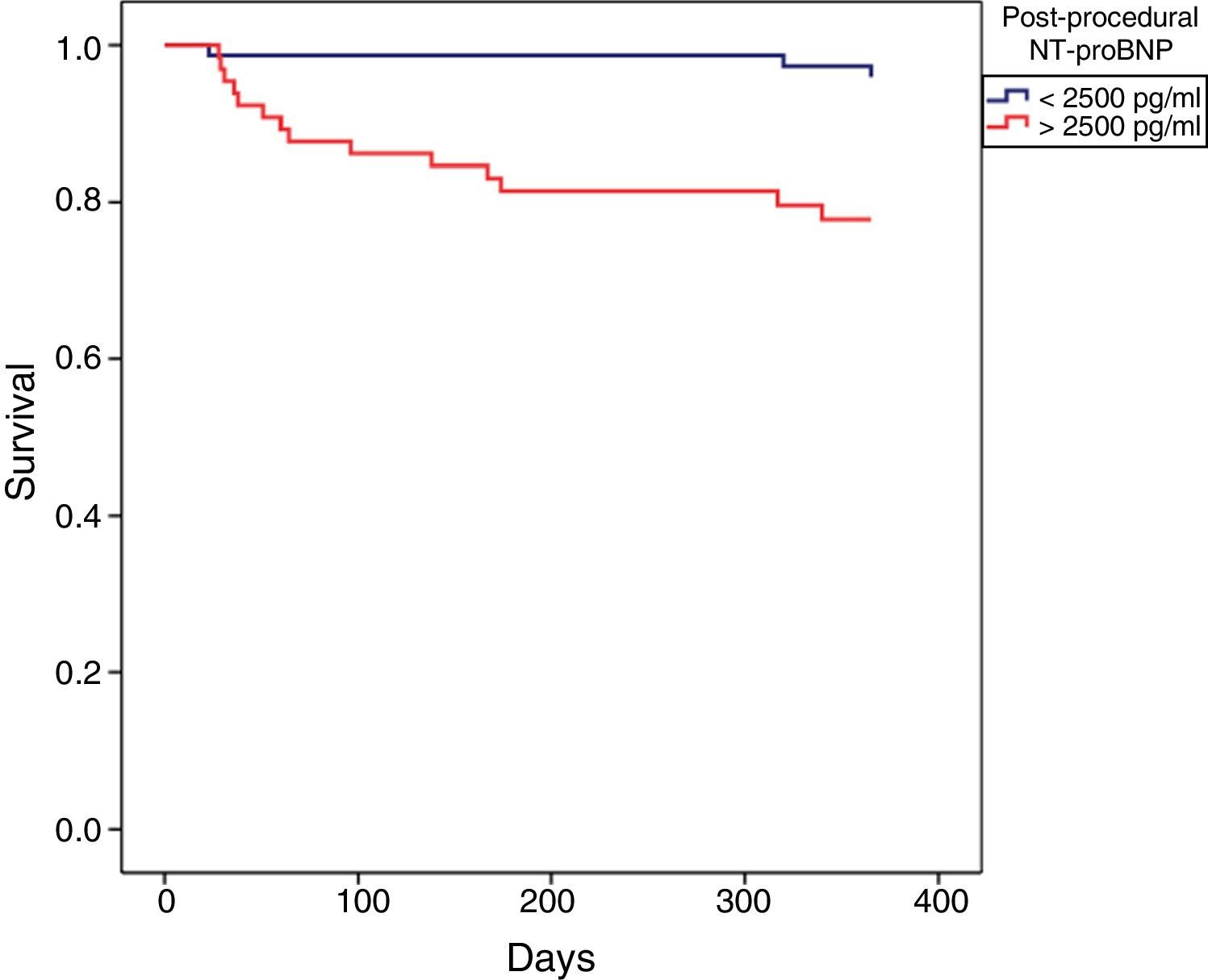
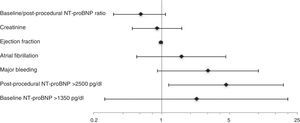
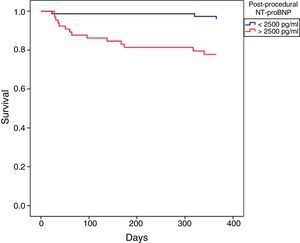
ResultsThe areas under the curve of baseline and post-procedural NT-proBNP for one-year mortality were 0.60 and 0.72, with the best cut-off values of 1350 and 2500 pg/ml, respectively. Atrial fibrillation, procedure-related major bleeding, baseline NT-proBNP higher than 1350 pg/ml, post-procedural NT-proBNP higher than 2500 pg/ml, higher creatinine and Society of Thoracic Surgeons score, and lower left ventricular ejection fraction were associated with one-year mortality. Only post-procedural NT-proBNP was independently and negatively associated with one-year survival (HR 5.9, 95% CI 1.6-21.7, p=0.008).
ConclusionsBaseline NT-proBNP did not predict one-year mortality; on the other hand one-month post-procedural NT-proBNP higher than 2500 pg/ml may identify a high-risk subset of patients, allowing better management, care and hypothetically outcome.
Os peptídeos natriuréticos são usados de forma ubíqua para o diagnóstico, seguimento e avaliação prognóstica em cardiologia. O NT-ProBNP correlaciona-se com a gravidade da estenose aórtica, porém o seu significado após VAP não está bem estabelecido.
ObjetivoAvaliar o valor prognóstico do NT-ProBNP nos doentes submetidos a VAP.
MétodosAnálise retrospetiva de 151 doentes, de um registo de 206 doentes consecutivos de novembro de 2008 a dezembro de 2014, com doseamentos de NT-ProBNP basal e após um mês da implantação de VAP. Os preditores independentes de mortalidade a um ano foram avaliados por regressão Cox.
ResultadosOs melhores valores discriminativos de NT-ProBNP basal e pós-procedimento foram 1.350 e 2.500, respetivamente. Somente um valor de NT-ProBNP pós-procedimento superior a 2.500pg/ml foi preditor independente e negativamente associado à sobrevida a um ano (HR 5,9; 95% IC 1,6-21,7; p = 0,008).
ConclusõesO NT-ProBNP basal não previu a mortalidade a um ano. Por outro lado, o NT-ProBNP superior a 2.500pg/ml após o procedimento identificou um subgrupo de doentes de alto risco, permitiu um melhor manejo, seguimento e possíveis resultados.
Transcatheter aortic valve implantation (TAVI) has emerged as a safe and effective alternative to surgical aortic valve replacement (SAVR) in high-risk or inoperable patients with severe aortic stenosis.1 Refinement in patient selection has prompted the use of multiple risk scores and analytical parameters to help predict outcomes. Most have been ineffective in that regard, with limited performance in this population with numerous comorbidities.2
Patients with severe aortic valve stenosis have elevated N-terminal pro-brain natriuretic peptide (NT-proBNP) levels, due to increased myocardial wall stress and pressure overload.3 Increased concentrations of this peptide have prognostic value in multiple heart conditions, and can be used for risk stratification.4,5 There is a correlation between NT-proBNP levels and severity of aortic stenosis.4 The post-procedural impact of NT-proBNP has been studied,6–9 and found to predict one-year mortality.10 However there is no established threshold beyond which outcomes worsen.
We sought to analyze the one-year prognostic value of NT-proBNP levels before and at one month after TAVI.
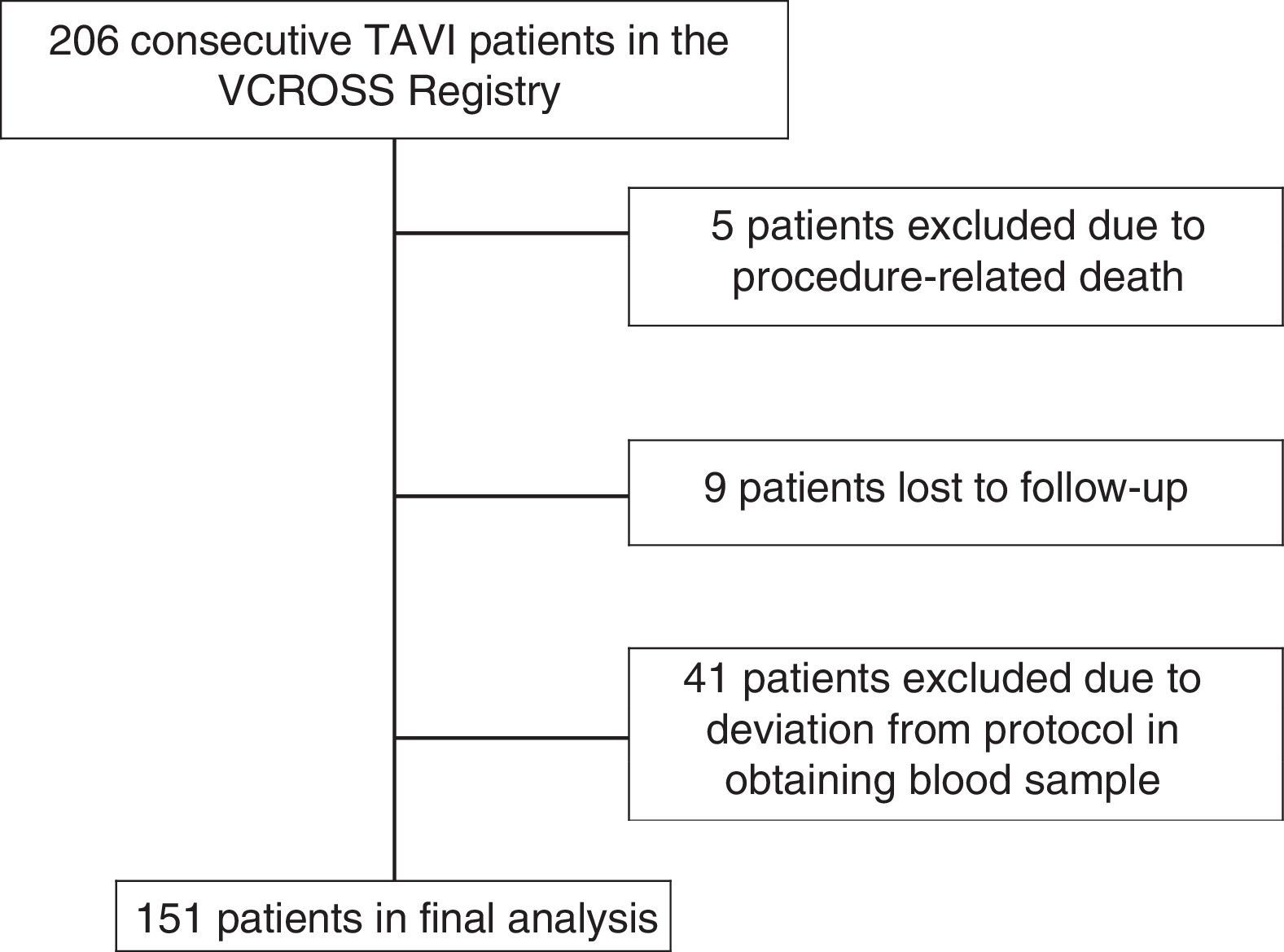
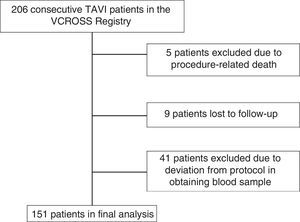
MethodsPatient population and data collectionThe Valve Catheter Restorative Operation on Santa cruz hoSpital (VCROSS) registry is an all-comer prospective single-center observational study that includes all consecutive patients with symptomatic aortic stenosis undergoing TAVI. Between November 2008 and December 2014 a total of 206 patients were treated, of whom 55 were excluded from this analysis (Figure 1): 46 patients deviated from the protocol for baseline or post-procedural NT-proBNP collection (five patients died before the 30-day assessment) and nine had follow-up in different institutions. A total of 151 patients thus entered the final analysis.
All data concerning demographic, clinical, laboratory and procedural characteristics were prospectively entered in our dedicated institutional database (CardiobaseTM, InforTUCANO). Post-discharge clinical follow-up was performed during scheduled outpatient visits or telephone interviews. NT-proBNP (chemiluminescence immunoassay, Roche, Minneapolis, MN; normal reference value <125 pg/ml) and other routine blood test parameters were measured in all analyzed patients in the week before and one month after the TAVI procedure. We calculated the difference and the ratio between pre- and post-procedural NT-proBNP and used them as independent variables.
A multidisciplinary heart team discussed and determined the implantation approach based on individual patient characteristics.11 Complications were reported according to the Valve Academic Research Consortium-2 classification.12
Statistical analysisContinuous variables were expressed as means and standard deviation when normally distributed and as medians and interquartile range (IQR) when not normally distributed. Normality was tested with the Kolmogorov-Smirnov test and/or visual assessment of Q-Q plots. Discrete variables were expressed as frequencies and percentages.
Baseline characteristics and outcomes were compared using the chi-square test or Fisher's exact test, when appropriate, for categorical variables, and the Student's t test or the Mann-Whitney U test for continuous variables, according to normality. Related non-normally distributed variables were compared by the Wilcoxon signed test.
The discriminative ability of baseline and post-procedural NT-proBNP was assessed by receiver operating characteristic (ROC) curve analysis. Areas under the curve (AUC) were compared by the method of DeLong et al. The best cut-off value of baseline and post-procedural NT-proBNP for one-year mortality determined by C-statistics was used to dichotomize the population, converting NT-proBNP into a categorical variable.
The ability of baseline and post-procedural NT-proBNP to predict one-year mortality above the best cut-off value was assessed by Cox regression including clinically significant variables shown to be associated with one-year mortality in univariate analysis.
Event-free survival was computed using Kaplan-Meier estimates and the log-rank test was used for comparison.
All tests were two-sided and differences were considered statistically significant at a p-value of 0.05. The statistical analysis was performed with SPSS 20.0 software (IBM SPSS Inc., Chicago, IL, USA).
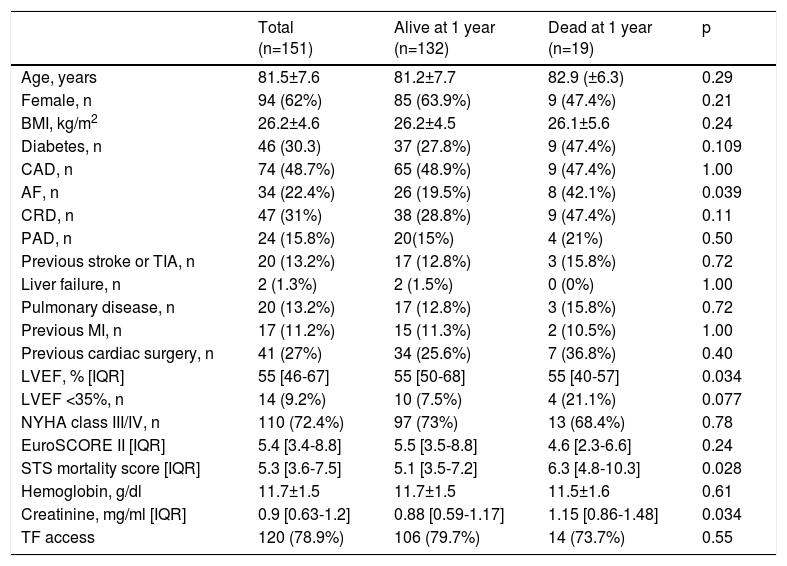
ResultsBaseline characteristicsThe overall baseline clinical characteristics of the study population are shown in Table 1.
Baseline characteristics of the study population.
| Total (n=151) | Alive at 1 year (n=132) | Dead at 1 year (n=19) | p | |
|---|---|---|---|---|
| Age, years | 81.5±7.6 | 81.2±7.7 | 82.9 (±6.3) | 0.29 |
| Female, n | 94 (62%) | 85 (63.9%) | 9 (47.4%) | 0.21 |
| BMI, kg/m2 | 26.2±4.6 | 26.2±4.5 | 26.1±5.6 | 0.24 |
| Diabetes, n | 46 (30.3) | 37 (27.8%) | 9 (47.4%) | 0.109 |
| CAD, n | 74 (48.7%) | 65 (48.9%) | 9 (47.4%) | 1.00 |
| AF, n | 34 (22.4%) | 26 (19.5%) | 8 (42.1%) | 0.039 |
| CRD, n | 47 (31%) | 38 (28.8%) | 9 (47.4%) | 0.11 |
| PAD, n | 24 (15.8%) | 20(15%) | 4 (21%) | 0.50 |
| Previous stroke or TIA, n | 20 (13.2%) | 17 (12.8%) | 3 (15.8%) | 0.72 |
| Liver failure, n | 2 (1.3%) | 2 (1.5%) | 0 (0%) | 1.00 |
| Pulmonary disease, n | 20 (13.2%) | 17 (12.8%) | 3 (15.8%) | 0.72 |
| Previous MI, n | 17 (11.2%) | 15 (11.3%) | 2 (10.5%) | 1.00 |
| Previous cardiac surgery, n | 41 (27%) | 34 (25.6%) | 7 (36.8%) | 0.40 |
| LVEF, % [IQR] | 55 [46-67] | 55 [50-68] | 55 [40-57] | 0.034 |
| LVEF <35%, n | 14 (9.2%) | 10 (7.5%) | 4 (21.1%) | 0.077 |
| NYHA class III/IV, n | 110 (72.4%) | 97 (73%) | 13 (68.4%) | 0.78 |
| EuroSCORE II [IQR] | 5.4 [3.4-8.8] | 5.5 [3.5-8.8] | 4.6 [2.3-6.6] | 0.24 |
| STS mortality score [IQR] | 5.3 [3.6-7.5] | 5.1 [3.5-7.2] | 6.3 [4.8-10.3] | 0.028 |
| Hemoglobin, g/dl | 11.7±1.5 | 11.7±1.5 | 11.5±1.6 | 0.61 |
| Creatinine, mg/ml [IQR] | 0.9 [0.63-1.2] | 0.88 [0.59-1.17] | 1.15 [0.86-1.48] | 0.034 |
| TF access | 120 (78.9%) | 106 (79.7%) | 14 (73.7%) | 0.55 |
AF: atrial fibrillation; BMI: body mass index; CAD: coronary artery disease; CRD: chronic renal disease; IQR: interquartile range; LVEF: left ventricular ejection fraction; MI: myocardial infarction; NYHA: New York Heart Association; PAD: peripheral arterial disease; STS: Society of Thoracic Surgeons; TF: transfemoral; TIA: transient ischemic attack.
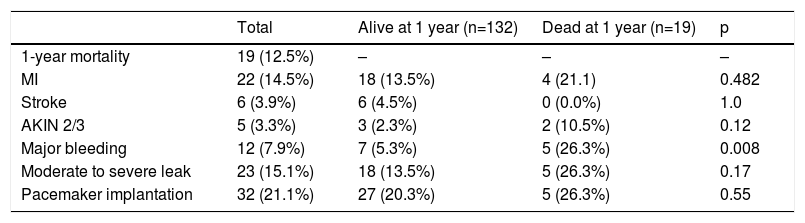
One hundred and twenty procedures (79%) were performed by a transfemoral approach. The devices implanted were 102 self-expandable valves (102 CoreValveTM, Medtronic®), 43 balloon-expandable valves (SapiensTM, Edwards®) and two LotusTM, Boston Scientific®, mechanical expandable and four PorticoTM, St Jude®. Procedural outcomes and complications are depicted in Table 2.
Complications according to the Valve Academic Research Consortium-2 classification.
| Total | Alive at 1 year (n=132) | Dead at 1 year (n=19) | p | |
|---|---|---|---|---|
| 1-year mortality | 19 (12.5%) | – | – | – |
| MI | 22 (14.5%) | 18 (13.5%) | 4 (21.1) | 0.482 |
| Stroke | 6 (3.9%) | 6 (4.5%) | 0 (0.0%) | 1.0 |
| AKIN 2/3 | 5 (3.3%) | 3 (2.3%) | 2 (10.5%) | 0.12 |
| Major bleeding | 12 (7.9%) | 7 (5.3%) | 5 (26.3%) | 0.008 |
| Moderate to severe leak | 23 (15.1%) | 18 (13.5%) | 5 (26.3%) | 0.17 |
| Pacemaker implantation | 32 (21.1%) | 27 (20.3%) | 5 (26.3%) | 0.55 |
AKIN: Acute Kidney Injury Network classification; MI: myocardial infarction.
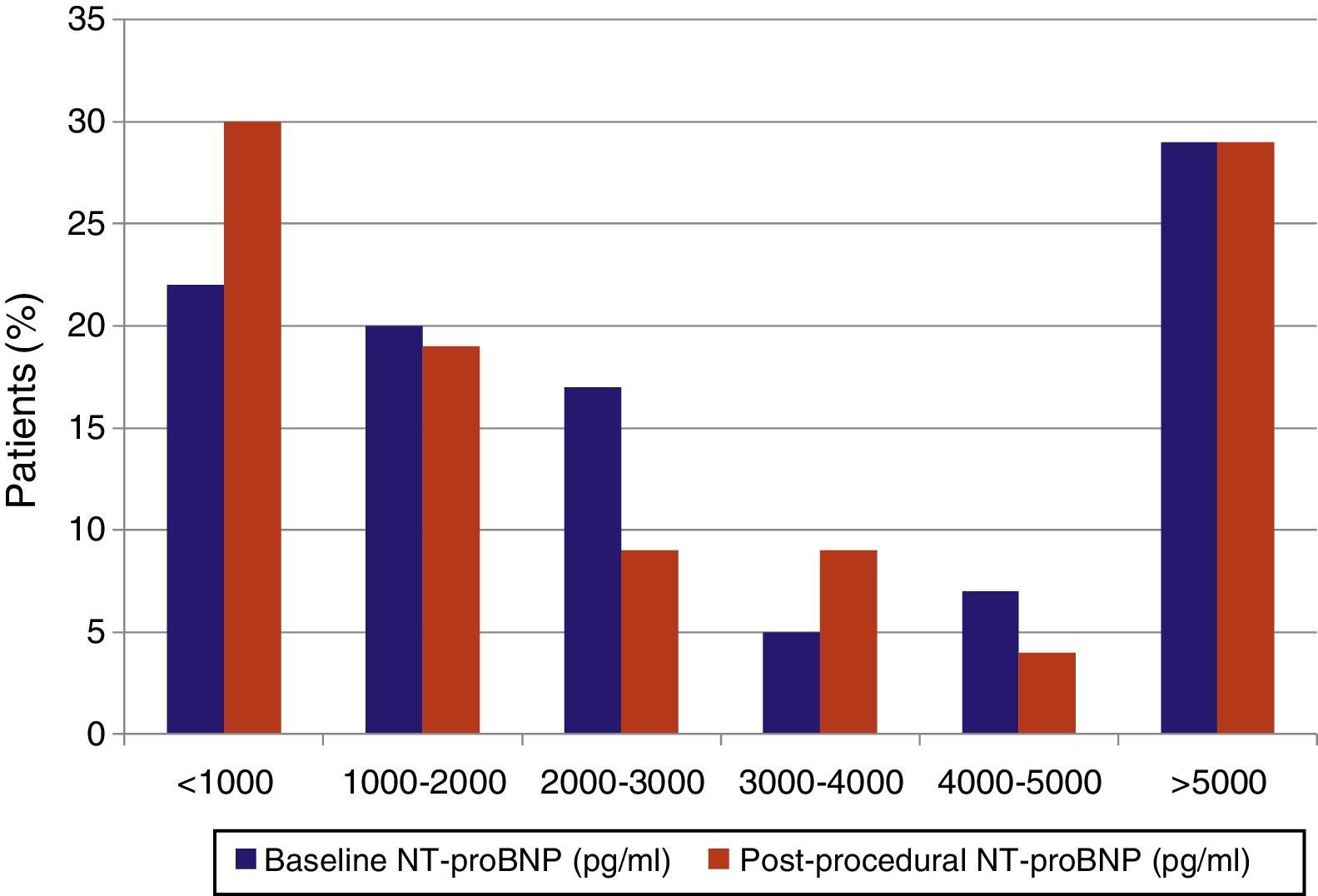
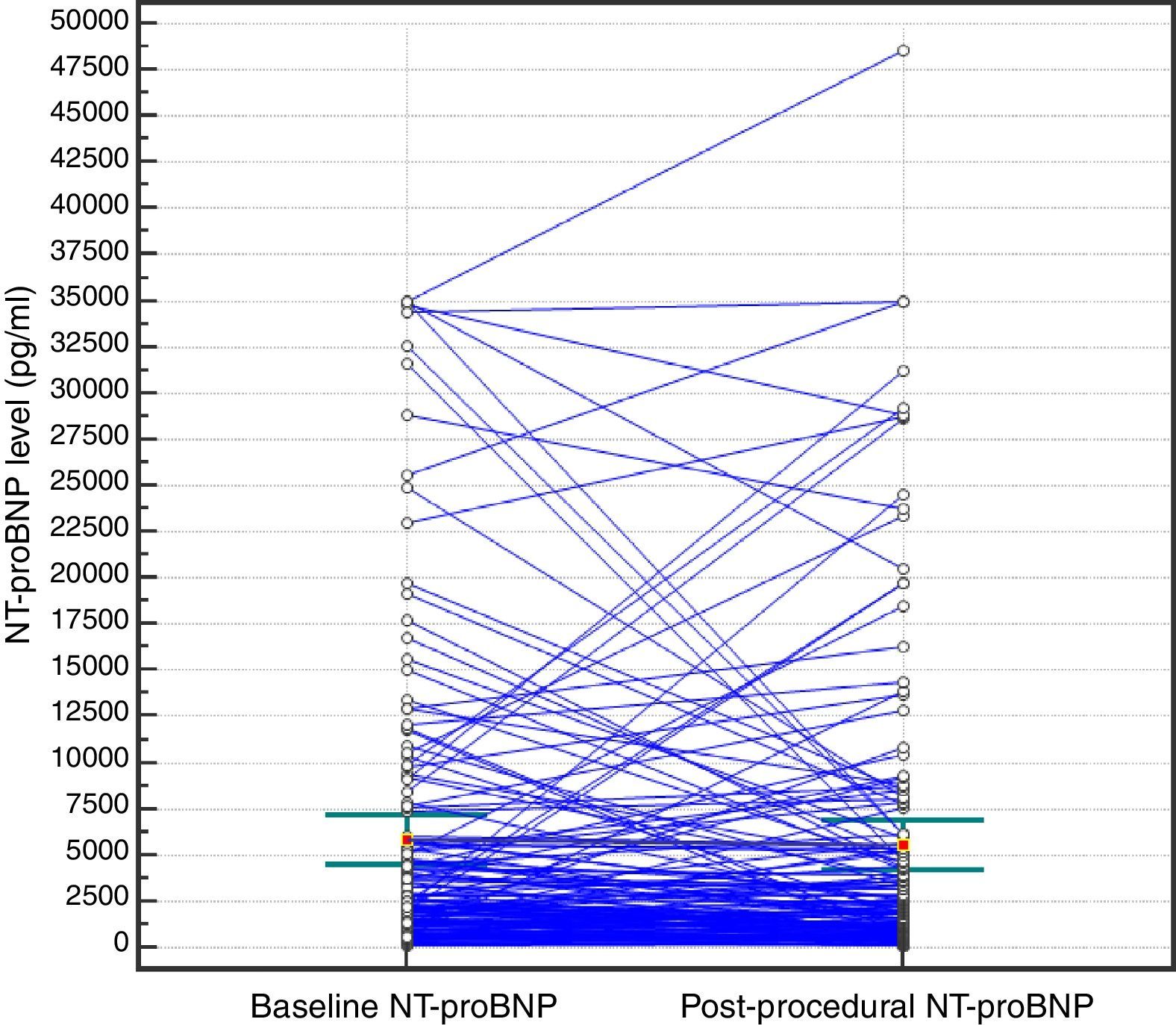
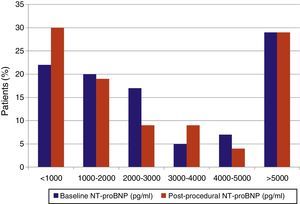
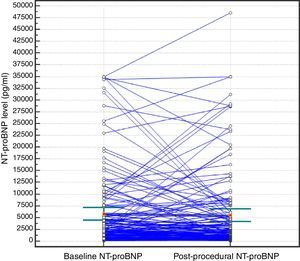
The median NT-proBNP levels pre- and post-procedure were 2335 pg/ml (IQR 1200-5787) and 2175 pg/ml (IQR 795-5589), respectively, and did not differ significantly (p=0.118). The median difference was 316 pg/ml (IQR [-125]-1708). The median of the ratio between NT-proBNP levels pre- and post-procedure was 1.2 (IQR 0.66-2.4). Ninety-six patients (63%) experienced a decrease in NT-proBNP after the procedure; the median decrease was 1110 pg/ml (IQR 349-3411). In patients with increased NT-proBNP (n=56, 37%), the median change was 1895 pg/ml (IQR 737-6240). NT-proBNP distribution and variation are shown in Figures 2 and 3.
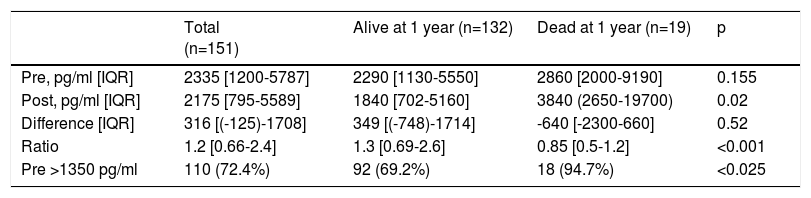
Overall one-year all-cause mortality was 12.6% (19/151). Patients who died had significantly higher Society of Thoracic Surgeons (STS) mortality scores, with more comorbidities including chronic renal disease and atrial fibrillation, and lower left ventricular ejection fraction and glomerular filtration rate (GFR) (Table 1). Periprocedural major bleeding was also associated with higher one-year mortality (Table 2). As for NT-proBNP as a continuous variable, only post-procedural values were shown to be associated with one-year mortality. We dichotomized both baseline and post-procedural NT-proBNP by the best cut-off value for one-year mortality determined by ROC curve analysis. The best cut-off values of baseline and post-procedural NT-proBNP were 1350 and 2500 pg/ml, respectively. Values above both thresholds were associated with one-year mortality (Table 3).
Association of N-terminal pro-brain natriuretic peptide levels with one-year survival.
| Total (n=151) | Alive at 1 year (n=132) | Dead at 1 year (n=19) | p | |
|---|---|---|---|---|
| Pre, pg/ml [IQR] | 2335 [1200-5787] | 2290 [1130-5550] | 2860 [2000-9190] | 0.155 |
| Post, pg/ml [IQR] | 2175 [795-5589] | 1840 [702-5160] | 3840 (2650-19700) | 0.02 |
| Difference [IQR] | 316 [(-125)-1708] | 349 [(-748)-1714] | -640 [-2300-660] | 0.52 |
| Ratio | 1.2 [0.66-2.4] | 1.3 [0.69-2.6] | 0.85 [0.5-1.2] | <0.001 |
| Pre >1350 pg/ml | 110 (72.4%) | 92 (69.2%) | 18 (94.7%) | <0.025 |
IQR: interquartile range; Pre: pre-procedural NT-proBNP level; Post: post-procedural NT-proBNP level.
Of the 19 patients who died within a year of the procedure, 18 (95%) had baseline NT-proBNP higher than 1350 pg/ml and 16 (84%) had post-procedural NT-proBNP above 2500 pg/ml (Table 3). The median baseline and post-procedural NT-proBNP of these patients were 2860 (IQR 2000-9190) and 3840 (IQR 2650-19700) pg/ml and did not differ significantly (p=0.227 for comparison).
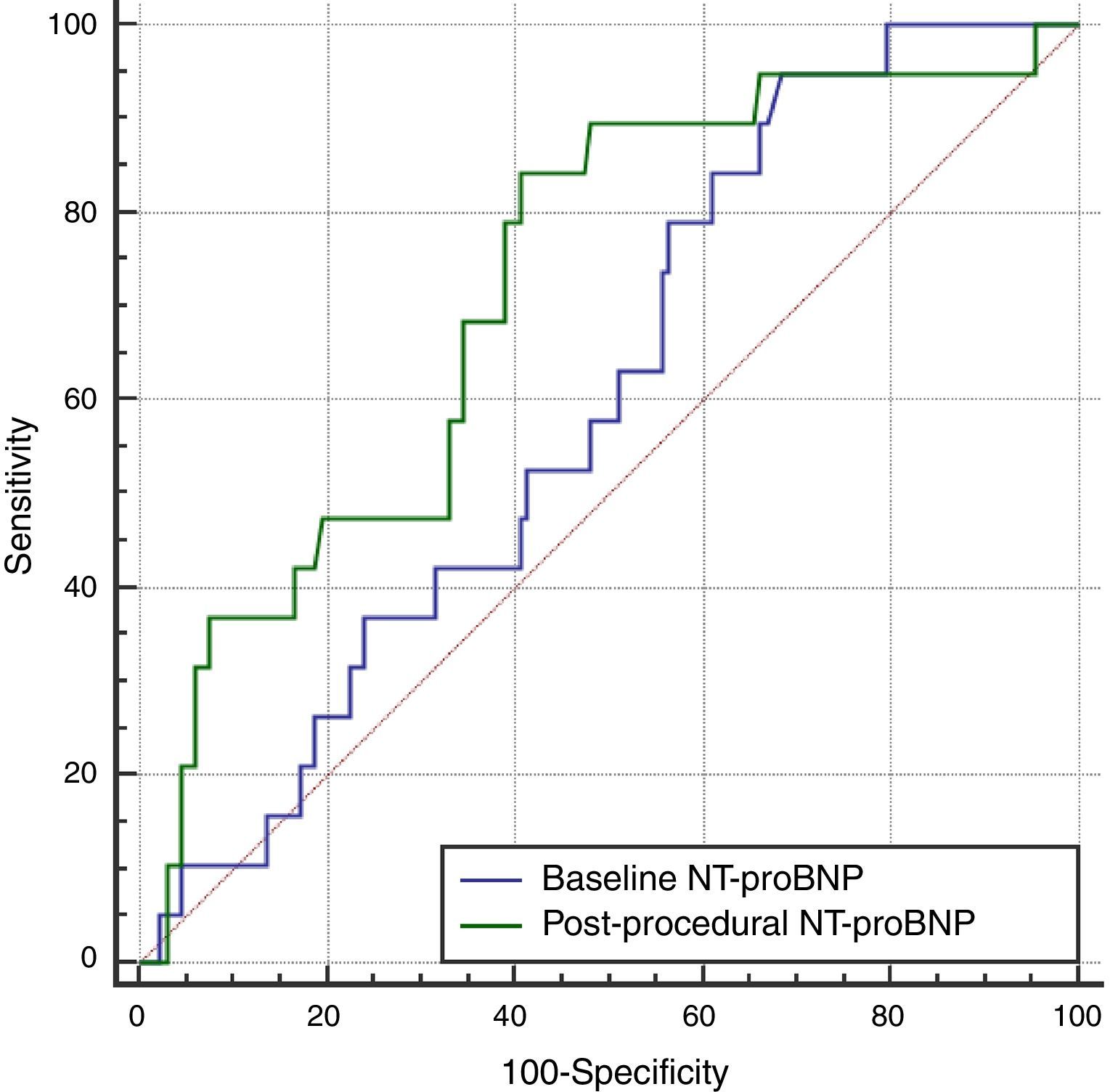
Discriminative abilityPost-procedural NT-proBNP discriminated one-year mortality numerically, but not significantly better than baseline NT-proBNP (AUC=0.72 for post-procedural NT-proBNP vs. AUC=0.60 for baseline NT-proBNP, p=0.12) (Figure 4).
Predictive abilityMultivariate Cox regression showed that only NT-proBNP higher than 2500 pg/ml (hazard ratio [HR] 5.9, 95% confidence interval 1.6-21.7, p=0.008) remained independently and negatively associated with one-year survival (Figures 5 and 6).
The main findings of the present study were: (1) early variation in NT-proBNP levels (during the first month after TAVI) was highly heterogeneous and the absolute value did not differ significantly from baseline; (2) baseline and post-procedural NT-proBNP above 1350 and 2500 pg/ml, respectively, were both associated with one-year mortality; (3) post-procedural NT-proBNP over 2500 pg/ml was the only independent predictor of one-year mortality on multivariate analysis.
In our population the variation between pre-procedural and one-month post-procedural NT-proBNP, although not significantly different, was highly heterogeneous (Figure 3). Only 63% of patients had lower NT-proBNP levels at 30 days, a smaller proportion than expected. As with SAVR,13 an immediate increase is often observed shortly after TAVI,14 due to hemodynamic fluctuations, fluid shifts and transient increases in wall tension during the procedure. Though a steady decrease is expected thereafter,7 it is not clear when this happens, as it may be affected by baseline clinical characteristics such as GFR, obesity, gender, other cardiac comorbidities and procedure-related features including access route, acute kidney injury and post-procedural bleeding. Improvement in afterload after TAVI is similar to that of SAVR patients,14 however baseline NT-proBNP is usually higher in the former as a result of TAVI being performed in older patients with more comorbidities, therefore the absolute reduction may be similar but the relative change is smaller. Notwithstanding, the lack of difference between baseline and post-procedural NT-proBNP in our cohort may be because patients in whom NT-proBNP increased (37%) had a higher absolute change in NT-proBNP values.
After dichotomization by the best cut-off value determined by ROC curve analysis, patients with NT-proBNP levels above these thresholds had higher mortality. However, after adjustment for other variables, only post-procedural NT-proBNP was independently associated with mortality (HR 5.9). Discrimination of patients who died from those who survived was numerically but not significantly better for post-procedural NT-proBNP. These findings suggest that post-procedural NT-proBNP has overall better predictive ability for one-year mortality.
The clinical significance of pre-procedural NT-proBNP regarding prediction of mortality remains controversial. One report showed that baseline NT-proBNP could predict mortality at two years,7 however in other studies, including a subgroup analysis of the Placement of AoRTic TraNscathetER Valve (PARTNER) I trial,15 baseline BNP levels did not predict one-year mortality. In our cohort we had similar findings to those of PARTNER I. These later results, along with the fact that the absolute difference and the ratio between baseline and one-month post-procedural NT-proBNP did not predict one-year mortality either, suggest that pre-procedural NT-proBNP is a good marker of cardiac overload but may not reflect the stage of myocardial disease and certainly not the overall mortality risk conferred by other comorbidities. On the other hand, one-month post-procedural NT-proBNP was associated with one-year mortality. Konstantinos et al. had previously reported that post-procedural NT-proBNP outperformed all other single measurements as a predictor of all-cause mortality at two years.7 Notwithstanding this known relationship, there is no established threshold at which outcomes worsen. In our population, one-month post-procedural NT-proBNP above 2500 pg/ml was the best cut-off value for one-year mortality and was shown to be a strong predictor (HR 5.9) of this endpoint in multivariate analysis. Thus post-procedural NT-proBNP might identify patients with advanced irreversible heart disease in whom overload reduction by aortic valve replacement does not change the natural history of the disease.
Predicted life expectancy is crucial in selecting patients for TAVI to minimize the futility of this procedure in very ill patients. We did not find a role for baseline NT-proBNP in predicting mortality, as it appeared to be ineffective in patient selection. Nevertheless, NT-proBNP shortly after a TAVI procedure can identify high-risk patients and help clinicians to predict outcomes and to optimize follow-up and management of heart failure and other comorbidities. Appropriate management may improve the overall prognosis.
LimitationsSome important limitations should be pointed out in our study. First, it has the inherent limitations of a single-center observational study. Second, the excluded patients may have limited the power of the statistical analysis. Third, the study time frame meant that only two types of valves were implanted in our center, using large sheaths for vascular access. This goes against contemporary practice, in which the trend is to use smaller sheaths. Fourth, both transapical and transfemoral access were used, introducing heterogeneity in the analysis, since the effect of apical scarring and remodeling on NT-proBNP levels in patients undergoing transapical TAVI is unknown. Fifth, it is not possible to ascertain the extent to which confounders intrinsic to specific selection criteria for TAVI influenced one-year mortality rates and thus the predictive ability of NT-proBNP. Sixth, patients who died before collection of post-procedural NT-proBNP were not assessed in our analysis, therefore we cannot exclude a possible association with baseline NT-proBNP.
ConclusionsIn a TAVI population that survived the early post-procedure period, baseline NT-proBNP did not predict one-year mortality, possibly making it less attractive for patient selection. Importantly, one-month post-procedural NT-proBNP higher than 2500 pg/ml identifies a high-risk subset of patients, allowing better management, care and hypothetically outcome.
Conflicts of interestThe authors have no conflicts of interest to declare