Left ventricular pseudoaneurysm is a rare complication of acute myocardial infarction, cardiac surgery, trauma or infection.
Since surgical repair is associated with high morbidity and mortality, percutaneous closure has been described as an alternative.
In this regard, we present a case in which a symptomatic large left ventricular pseudoaneurysm was treated by percutaneous closure due to the patient's high surgical risk, using a double snare technique.
Despite the technical difficulties, this procedure had a good final result followed by clinical success, confirming that this procedure is an effective alternative to surgery in high-risk patients.
O pseudoaneurisma do ventrículo esquerdo consiste numa complicação rara após enfarte agudo do miocárdio, cirurgia cardíaca, trauma ou infeção.
Dado que a sua correção cirúrgica se associa a uma elevada morbi-mortalidade, o encerramento percutâneo tem sido descrito como uma possível alternativa.
Neste contexto, apresentamos um caso de um volumoso pseudoaneurisma do ventrículo esquerdo, o qual fora encerrado percutaneamente, utilizando uma técnica de duplo snare, devido ao elevado risco cirúrgico da doente.
Apesar de algumas dificuldades técnicas, este procedimento teve um bom resultado final, com sucesso clínico a longo prazo, confirmando que o encerramento percutâneo constitui uma alternativa efetiva à cirurgia, em doentes de alto risco operatório.
Left ventricular (LV) pseudoaneurysm is a rare complication of acute myocardial infarction, cardiac surgery, trauma or infection.1
The risk of rupture of a LV pseudoaneurysm, according to the literature, ranges from 30% to 45% during the first year.2
Open surgical repair has been accepted as the standard of care, but it is associated with significant morbidity and mortality, related to anatomic complexity and patient characteristics, particularly older age and comorbidities.1,2 Consequently, percutaneous closure has been described as a viable alternative to surgical intervention in high-risk patients.1–7
In this regard, we present the case of a patient at high surgical risk in which it was necessary to use a double snare technique for percutaneous closure of a giant LV pseudoaneurysm.
Case reportAn 81-year-old woman, with a history of surgical correction of an interventricular septal defect following anterior myocardial infarction (four years previously) and chronic obstructive pulmonary disease, complained of atypical thoracic pain. The physical examination revealed a grade II/VI systolic murmur, loudest at the apex.
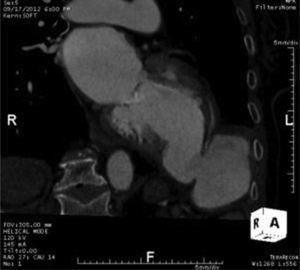
The diagnostic investigation, including computed tomography (CT) angiography (Figure 1) and left ventricular angiography (Figure 2), showed a large (52 mm×48 mm×55 mm) left ventricular wall pseudoaneurysm and a 21 mm×24 mm defect in the ventricular wall.
Since the patient was considered to have a high risk of mortality, she was not accepted for surgery and was consequently referred to percutaneous treatment, which was performed under transesophageal echocardiographic guidance.
An initial attempt at a retrograde approach (through the left femoral artery) was unsuccessful because the delivery sheaths were too small, so an anterograde approach was adopted. A 260 cm 0.35″ hydrophilic wire (ZIPwire®) was positioned retrogradely in the left atrium with an Amplatz left diagnostic catheter from the left femoral artery. After transseptal puncture through the right femoral vein, this wire was snared and brought into the inferior vena cava (Video 1). From the right jugular vein, the wire was then snared a second time and exteriorized (Videos 2 and 3), creating an arteriovenous loop (left femoral artery – right jugular vein).
A 10F Amplatzer® TorqueVue® delivery sheath was then advanced from the right jugular vein, crossing both the interatrial septum and mitral valve and subsequently entering the left ventricle.
The pseudoaneurysm was engaged with a standard 0.035″ wire and a left mammary diagnostic catheter inside the delivery sheath that successfully entered its cavity.
Finally, a 24 mm Amplatzer® ASD occluder was implanted in a stable position, closing the free wall defect (Videos 4-7).
At six-month follow-up, the patient remains asymptomatic, with no adverse events, and the device is in the appropriate position confirmed by CT (Figures 3 and 4).
This case report illustrates a rare complication of cardiac surgery, namely an LV pseudoaneurysm.
Considering the patient's high surgical risk, she was treated by percutaneous closure of the pseudoaneurysm, as described in the literature.1–7
Since a retrograde approach (via the left femoral artery) was not possible due to the fact that the delivery sheaths were too small, an anterograde approach by transseptal puncture (through the right femoral vein) with a double snare technique (the first snare from the left atrium to the inferior vena cava and the second snare to the right jugular vein) was chosen. This had the additional advantage of creating a direct non-tortuous path to the left ventricular chamber, facilitating sheath maneuvers and advancing and positioning of the device.
This technique enabled successful implantation of an Amplatzer® ASD device to close the free wall defect.
Despite all the technical difficulties, percutaneous closure of the ventricular wall defect with a double snare technique had both imaging and clinical success, rendering the patient asymptomatic and event-free.
Consequently, this result confirms that this procedure is an effective alternative to surgery in patients at high surgical risk.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.