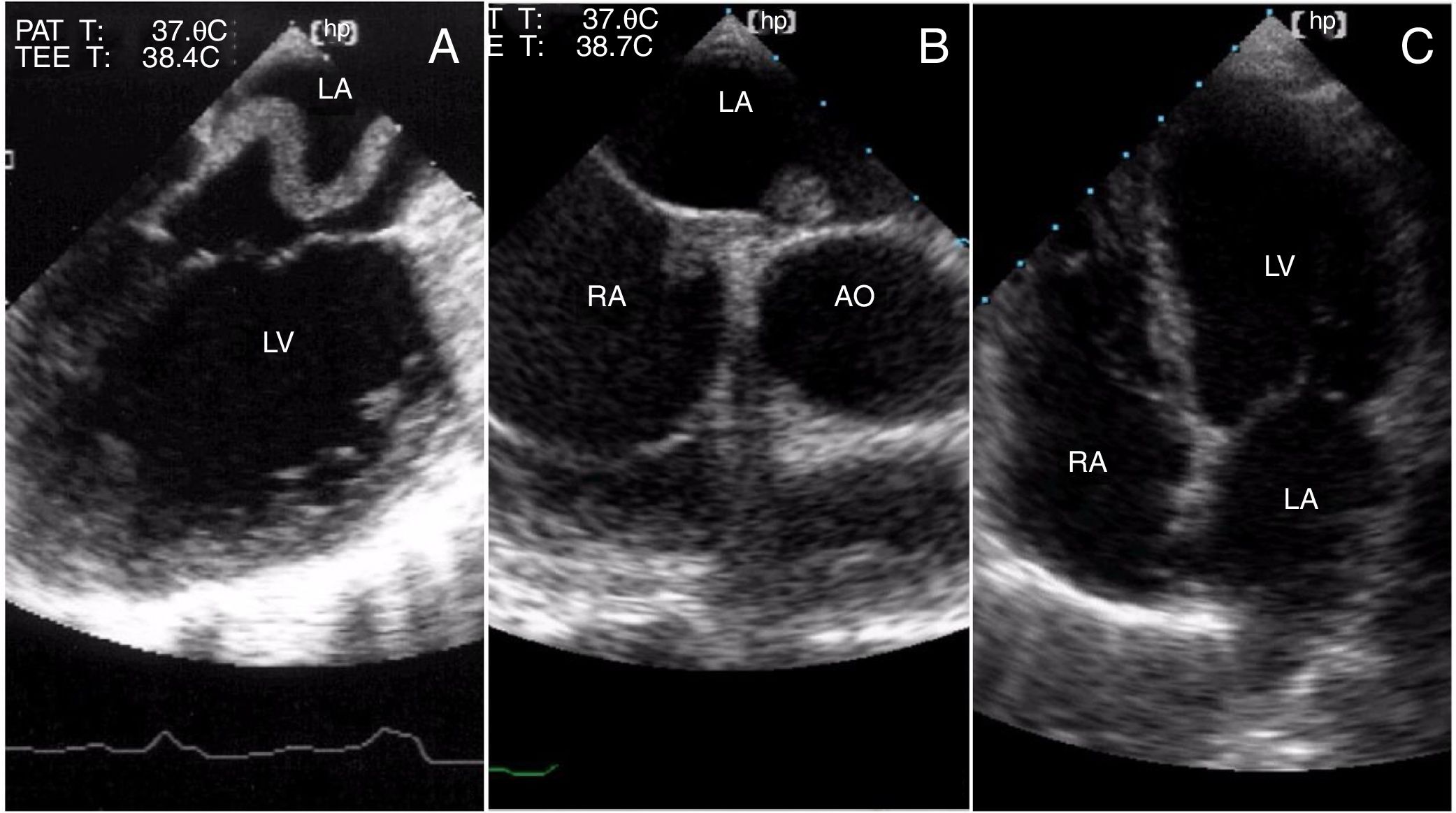
A 65-year-old woman was admitted to the hospital with fever and decompensated heart failure. She had long-lasting peripheral venous insufficiency and had been experiencing heart failure symptoms for six months. She had no history of hypertension, diabetes mellitus, coronary heart disease, atrial fibrillation, stroke or transient ischemic attack. Six days after admission, she developed acute pulmonary edema. A transesophageal echocardiography (TEE) revealed severe left ventricular dysfunction and an intracardiac thrombus measuring 5-6 cm, traversing a small patent foramen ovale (PFO) (Figure 1A). Unfractionated heparin was promptly initiated. Nevertheless, one week later, she woke up aphasic with right-sided hemiparesis. A brain computed tomography scan showed a left hemispheric stroke, while the patient's blood work, a cervical duplex scan and cardiac catheterization revealed no significant findings. The TEE was repeated and a smaller thrombus found (Figure 1B). Two months after discharge, the thrombus was undetectable (Figure 1C).
PFO is not considered to be a major cause of cardioembolic stroke, especially in the elderly, since other potential causes exist. Our case, however, shows that a causative thrombus resulting from a paradoxical PFO embolism could be detected before giving rise to a stroke. This case is important as it allowed direct thrombus imaging within the PFO before it led to a stroke, which is not always possible, as well as revealing a smaller thrombus trapped inside the PFO after the stroke. The first thrombus visualized probably arose from the venous system of the lower limbs and passed through a small ostium, giving us the exceptional opportunity to prove the stroke's cardioembolic etiology through a PFO in an elderly patient.
Conflicts of interestThe authors have no conflicts of interest to declare.