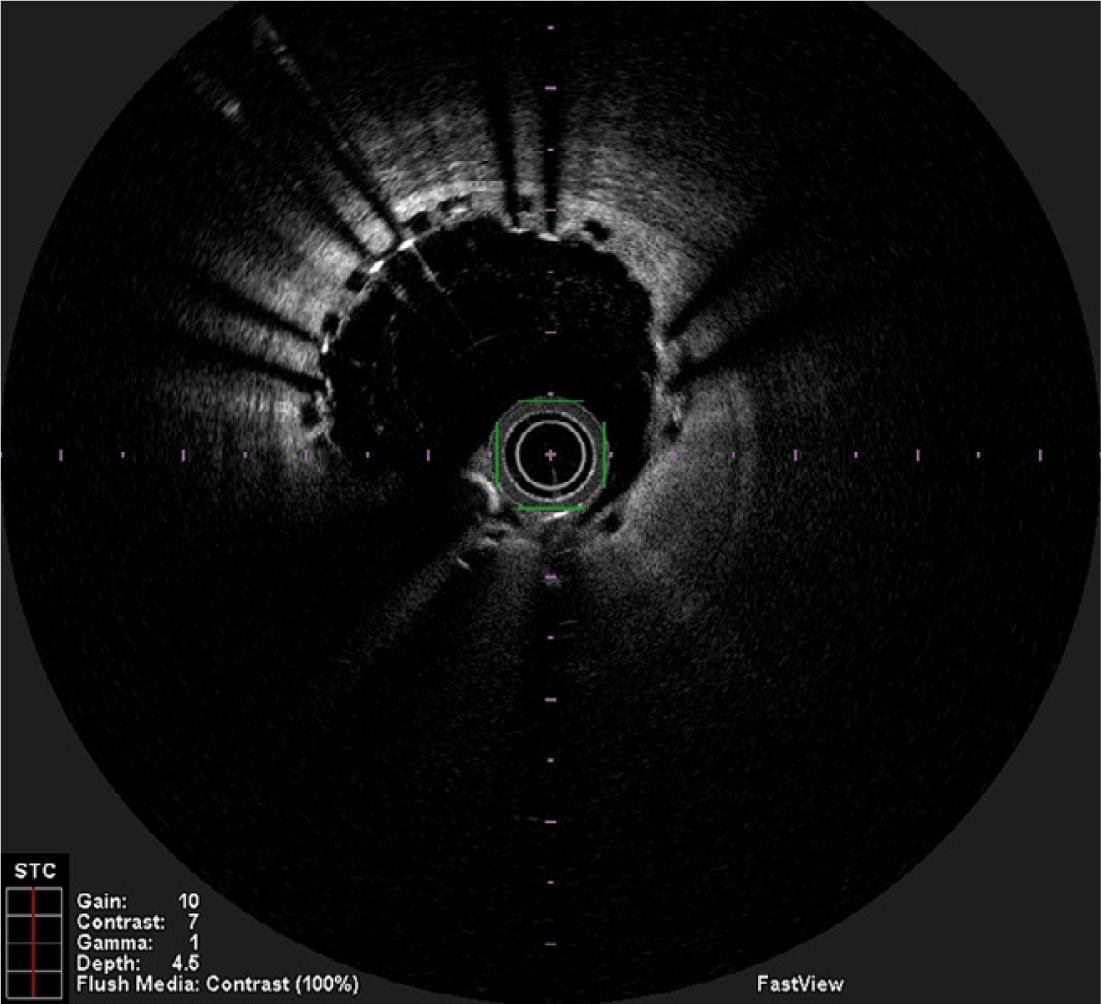
A 49-year-old Caucasian woman with prior history of hypertension, diabetes and smoking presented with an inferior ST-elevation myocardial infarction in Killip class I. Ischemia time was four hours. Primary percutaneous coronary intervention (PCI) was performed with thrombus aspiration and direct stenting with a drug-eluting stent (DES). She subsequently underwent PCI with bioresorbable vascular scaffolds (BVS) in the circumflex artery (Cx). After deployment of the BVS a coronary perforation was seen at the distal edge of the device. A stent graft was implanted overlapping the edge of the BVS. The perforation was resolved, nevertheless the distal lesion on the CX artery needed to be revascularized. As another BVS did not cross the proximal BVS, we implanted another metal DES overlapping the stent graft. Optical coherence tomography (OCT) images confirmed right stent expansion and apposition.
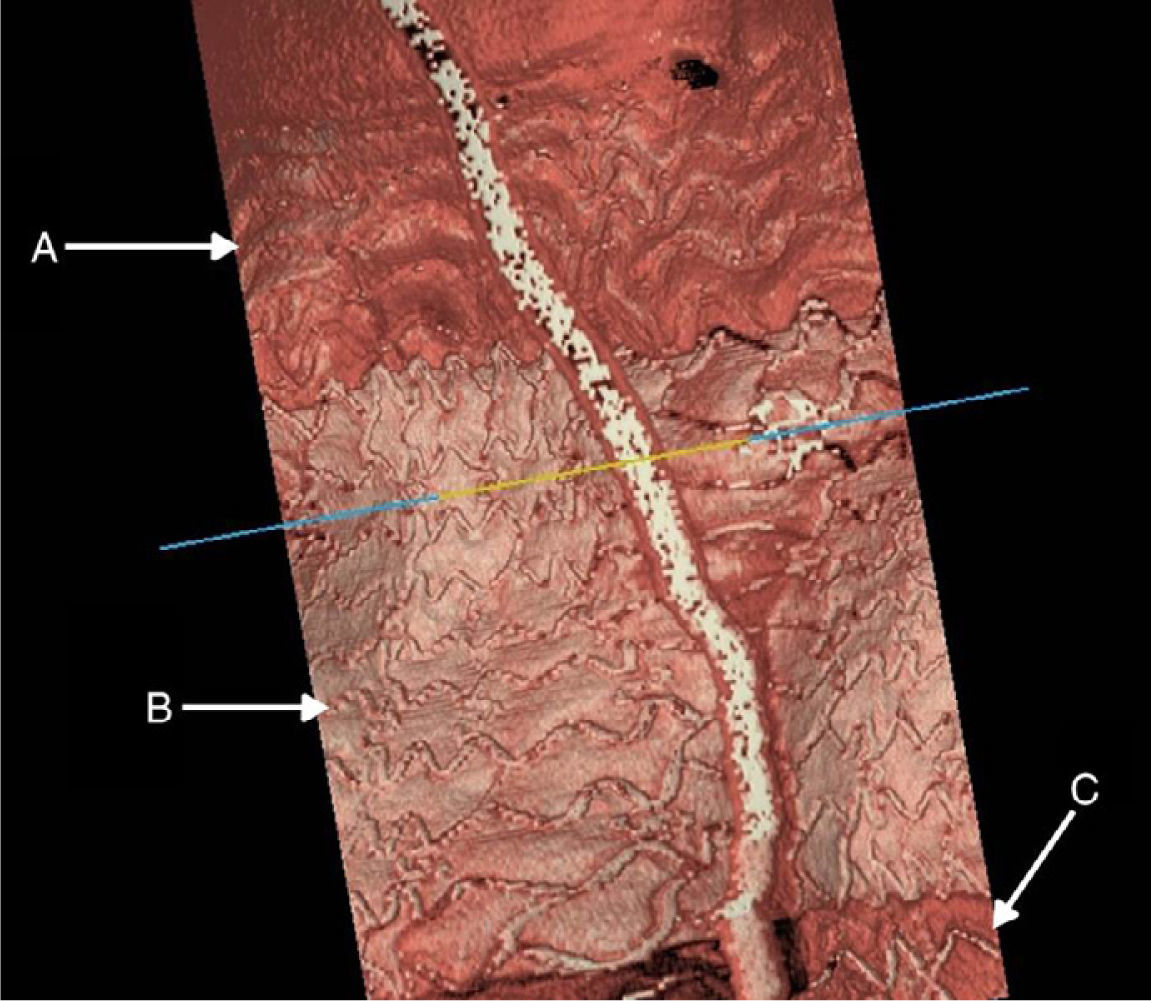
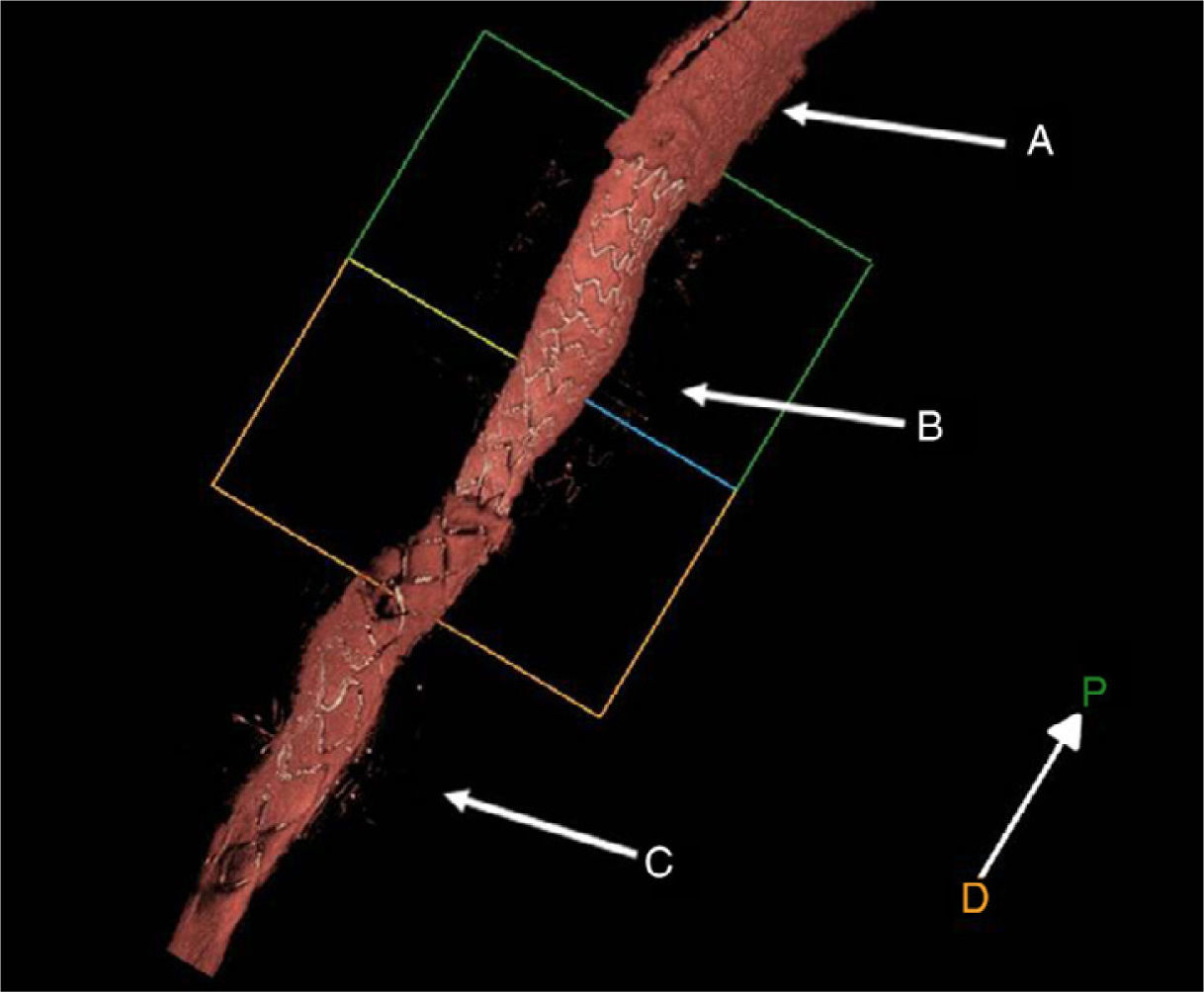
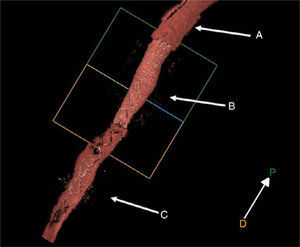
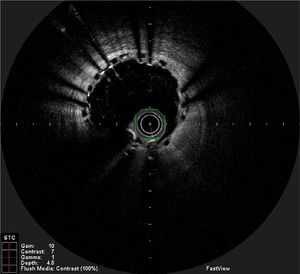
We report an example of successful treatment of a coronary intervention complication with three different kinds of stent. Currently BVS are much less navigable than metal DES; this case is a good example on this characteristic. OCT images show the interface between the resorbable scaffold, the polymer layer of the stent graft and the metal strut of the distal DES (Figures 1 and 2). Figure 3 shows the stent graft overlapping the BVS.
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.