An 83-year-old woman with a 10-year history of rheumatoid arthritis was admitted for urinary tract infection with exacerbation of chronic kidney disease and decompensated heart failure of unknown etiology. Transesophageal echocardiography (TEE) showed a vegetation involving the posterior mitral valve leaflet, and a hypothesis of infective endocarditis was proposed. Empirical antibiotic therapy was initiated. TEE was repeated after antibiotic therapy, and showed persistence of the original vegetation and revealed the presence of another, smaller vegetation. Clinical investigation revealed no infectious process, and so a diagnosis of nonbacterial thrombotic endocarditis (NBTE) was established. Anticoagulant therapy was started immediately. The NBTE lesion had disappeared on the follow-up echocardiogram two months after anticoagulant therapy.
Doente de 83 anos, sexo feminino, com antecedentes de artrite reumatoide há 10 anos, foi internada por infecção do trato urinário com lesão renal aguda em doença renal crónica e insuficiência cardíaca descompensada de etiologia não esclarecida. Ecocardiograma transesofágico (ETE) com vegetação apensa ao folheto posterior da válvula mitral, colocando-se a hipótese de endocardite infecciosa, tendo-se iniciado antibioterapia empírica. Repetição de ecocardiograma transesofágico após antibioterapia com manutenção da vegetação referida e menção a outra de menores dimensões, sendo colocada a hipótese de endocardite trombótica não bacteriana. A investigação clínica não evidenciou qualquer processo infeccioso. Após hipocoagulação durante dois meses, foi repetido o ecocardiograma transesofágico com desaparecimento das vegetações anteriormente apresentadas.
Nonbacterial thrombotic endocarditis (NBTE), which has also been termed abacterial, minimal, verrucal, degenerative, terminal or marantic endocarditis, is an uncommon disorder characterized by the presence of aseptic vegetations composed of fibrin and platelets on the cardiac valves.1 These lesions result from various types of insult secondary to disorders that include hypercoagulable states, malignancy (especially adenocarcinoma), and autoimmune diseases such as systemic lupus erythematosus, antiphospholipid syndrome and rheumatoid arthritis (RA).2
NBTE usually affects patients between the fourth and eighth decades of life, with no difference between genders, although some studies have found a predominance of females.3 The absence of diagnostic signs and the fact that patients are asymptomatic until they suffer an embolic event (which occurs in 42% of cases) mean that the condition is underdiagnosed antemortem.4,5
Although NBTE is rare and difficult to diagnose, requiring a high degree of suspicion, early diagnosis is crucial in preventing thromboembolic events and improving patients’ quality of life. It may also lead to the diagnosis of an underlying disease, such as occult malignancy. The authors therefore believe that sharing this clinical case may shed more light on this entity, highlighting its importance when considering different diagnoses of cardiac vegetations.
Case reportAn 83-year-old Caucasian woman was admitted for urinary tract infection with exacerbation of chronic kidney disease (CKD) and decompensated heart failure (HF). Her medical history included essential hypertension, dyslipidemia, morbid obesity (body mass index 62.5 kg/m2), permanent atrial fibrillation not under anticoagulant therapy, HF of unknown etiology, RA for 10 years and stage 3 CKD. Physical examination revealed joint deformities in the hand including interosseous atrophy and ulnar deviation but no other relevant alterations.
During hospitalization empirical antibiotic therapy with ceftriaxone and diuretic therapy were initiated, leading to clinical and laboratory improvement. The exams included urine culture, from which Escherichia coli sensitive to the antibiotic prescribed was isolated, negative blood cultures, and renal-gallbladder ultrasound that showed signs of CKD.
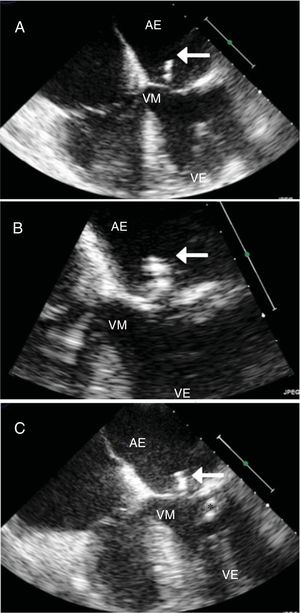
Transthoracic echocardiography (TTE) was performed in order to determine the cause of the patient's HF and to assess her cardiac function. This revealed findings compatible with hypertensive heart disease (left atrial dilatation, moderate left ventricular hypertrophy, mild mitral regurgitation and grade 2 diastolic dysfunction) and preserved biventricular systolic function, and also identified a mobile mass attached to the mitral valve leaflets. Transesophageal echocardiography (TEE) confirmed this mass to be a vegetation around 19 mm×4 mm in size, adhering to the atrial face of the posterior valve leaflet and highly mobile (Figure 1A and B).
Transesophageal echocardiography (TEE) showing nonbacterial thrombotic endocarditis. (A and B) Initial TEE showing a vegetation on the mitral valve posterior leaflet (arrow); (C) following a course of antibiotic therapy, the vegetation can still be observed on the mitral valve posterior leaflet (arrow) and a new vegetation around 10 mm in size has appeared attached to the chordae tendineae of the posterior leaflet (asterisk). AD: right atrium; AE: left atrium; VD: right ventricle; VE: left ventricle; VM: mitral valve.
In view of these findings, the patient's HF was characterized as HF with preserved ejection fraction in a patient with hypertensive heart disease. A diagnosis of infectious endocarditis was proposed and new blood cultures were taken, while gentamicin was added empirically to the previously prescribed antibiotic ceftriaxone. On the fifth day of combined antibiotic therapy, the patient's renal function worsened, taken to be related to the nephrotoxicity of gentamicin, which was discontinued. The results of various blood cultures were all negative.
After four weeks of therapy with ceftriaxone, TEE was repeated and showed persistence of the original vegetation and revealed the presence of another, smaller vegetation, around 10 mm in size, attached to the posterior mitral valve leaflet (Figure 1C).
Studies performed during hospitalization revealed elevated rheumatoid factor (26 IU/ml) and the A1298C mutation in the MTHFR gene in homozygosity. Laboratory exams, including blood panel and coagulation and biochemical tests, were normal, as were screening for lupus erythematosus cells, lupus anticoagulant, complement levels, and serological response to VDRL, antinuclear, antiphospholipid and anti-HIV antibodies. The thoracic-abdominal-pelvic computed tomography (CT) scan showed no relevant alterations. Further blood cultures were performed after discontinuation of antibiotic therapy, once again failing to isolate any agent.
A diagnosis of NBTE was established and anticoagulation with low molecular weight heparin adjusted for renal function was instituted.
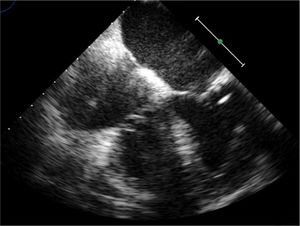
The patient was discharged under oral anticoagulation with warfarin and referred for outpatient consultations. At two months after discharge she was asymptomatic and the TEE revealed no vegetations (Figure 2).
DiscussionNBTE is an uncommon but underdiagnosed clinical entity. It was first described by Ziegler in 1888 as thromboendocarditis.6 It is characterized by friable vegetations made up of fibrin, platelets and red blood cells on the cardiac valves, most often on the mitral valve, followed by the aortic valve. It is differentiated from infectious endocarditis by the absence of any underlying infectious process.5 Its clinical manifestations are non-specific and a new cardiac murmur is only detected in 33% of cases, and so diagnosis is usually postmortem; its reported incidence in autopsy studies ranges from 0.3% to 9.3%.7
TEE is the method of choice to diagnose endocarditis, since it is the most sensitive in visualizing vegetations (90% vs. 70% for TTE). However, a definitive diagnosis is currently only possible through histological study of the mass.
NBTE is frequently associated with cancer in postmortem studies (80%), while autoimmune diseases, particularly antiphospholipid syndrome, predominate in antemortem studies (46%).2,8 It has often been reported in association with chronic debilitating diseases such as acquired immune deficiency syndrome, systemic lupus erythematosus and RA. The pathogenesis of NBTE is not fully understood, but endothelial damage resulting from hypercoagulable states is thought to be crucial to its development. The patient in the case described had the A1298C mutation in the MTHFR gene in homozygosity. This mutation leads to elevated levels of homocysteine, and thus predisposes to thrombotic events.9
RA is a common systemic autoimmune disease characterized by chronic inflammation of the synovial structures. This inflammation is thought to be related to the 1.5- to 6-fold increased risk of thromboembolism in patients with RA. The main proinflammatory cytokines (interleukin-6, interleukin-8 and tumor necrosis factor alpha) are believed to be responsible for this increase, both by activating coagulation pathways and by altering thrombotic tendency.10
When the diagnosis is of possible endocarditis according to the modified Duke criteria, further clarification can be obtained by 18F fluoro-2-deoxyglucose positron emission tomography or CT or by single-photon emission computed tomography or CT with radioisotope-labeled leukocytes. However, the patient in the case presented did not give her consent for these exams.
The fact that our patient remained apyretic throughout hospitalization, together with the persistence of the echocardiographic findings after antibiotic therapy, the exclusion of an infectious process, the presence of the A1298C mutation in the MTHFR gene in homozygosity and her history of RA, were strong evidence for a diagnosis of NBTE. Accordingly, after the main differential diagnosis of infective endocarditis was excluded, anticoagulant therapy was initiated, which resulted in the disappearance of all lesions within two months. The target international normalized ratio for this patient was 2-3, since there is no evidence that other target values show a better relationship between thrombotic and bleeding risk in patients with thrombophilia.11
To the best of our knowledge, this is one of the few case reports in the literature on NBTE in patients with RA in whom the mitral valve was involved and who were diagnosed before the occurrence of a thromboembolic event.12,13
It is crucial to perform systematic prospective studies in populations of patients with cancer or autoimmune disease in order to improve our knowledge of NBTE, to determine its real prevalence, and to assess the morbidity and mortality associated with this condition.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Campos ID, Marques AR, Sousa L, Fonseca S, Oliveira C, Vieira C, et al. Endocardite trombótica não bacteriana. Rev Port Cardiol. 2019;38:511–514.