We read the exhaustive review by Machado and Vaz Silva entitled “Benign and pathological electrocardiographic changes in athletes”1 with great interest.
As stated in the article, the Seattle criteria2 are among the most commonly used tools for assessing the electrocardiogram (ECG) of athletes, in order to detect and differentiate pathological alterations from those related to intense exercise. They have improved the false-positive rate while maintaining diagnostic accuracy in particular populations,3–5 compared to the previous recommendations for the interpretation of the ECG in athletes published by the European Society of Cardiology (ESC), initially in 20056 and updated in 2010.7
However, although the Seattle criteria were the first to address the influence of race, with specific recommendations for individuals of African and Afro-Caribbean origin (who have a higher risk of sudden cardiac death8), the false-positive rate remains high, especially in black athletes.3–5,9,10 This increases the cost of pre-participation screening,7 besides the consequences of exclusion from competitive sports in terms of the professional and emotional impact on athletes’ lives.
Sheikh et al.10 compared ECG changes between black and white athletes and proposed a set of ‘refined’ criteria which, without losing sensitivity, improved specificity, particularly in black athletes. These new criteria are predicated on the idea that isolated ECG findings of left or right atrial dilatation, left or right axis deviation, and/or right ventricular hypertrophy are of dubious value in athletes without symptoms, family history or abnormalities on physical examination (Table 1). Sheikh et al.’s study retrospectively assessed the ECGs of 5505 elite athletes (4297 white and 1208 black), most of them male. The ECGs were analyzed according to the ESC recommendations,7 the Seattle criteria,2 and the new refined criteria.10 Abnormalities were identified in 21.5%, 9.6% and 6.6% of the total population, respectively. The reduction in ECGs classified as abnormal was more marked in black athletes (40.4% by the ESC criteria, 18.4% by the Seattle criteria and 11.5% by the refined criteria), and was also seen in white individuals, although to a lesser extent (16.2%, 7.1% and 5.3%, respectively). The reduction in abnormal ECGs compared to the Seattle criteria was thus 37.5% in black athletes and 25.4% in white athletes. The specificity of the refined criteria was 94.1% for white athletes and 84.2% for black athletes, better than the ESC criteria (73.8% and 40.3%, respectively) and the Seattle criteria (92.1% and 79.3%). This improvement in specificity was achieved without compromising sensitivity, all three sets of criteria identifying all athletes with major cardiac disorders and 98.1% of athletes with hypertrophic cardiomyopathy.
Definition of abnormal ECGs using the refined criteria.
| Training-related normal variants (not warranting further investigation in asymptomatic athletes with no family history or abnormal physical findings) |
|---|
| • Sinus bradycardia • First-degree atrioventricular block • Incomplete right bundle branch block • Early repolarization • Isolated QRS voltage criteria for left ventricular hypertrophy |
| Borderline variants (potentially warranting further investigation if two or more are present) |
| • Left atrial enlargement • Right atrial enlargement • Left axis deviation • Right axis deviation • Right ventricular hypertrophy • T-wave inversion up to V4 in black athletes (when preceded by characteristic convex ST-segment elevation) |
| Training-unrelated changes (warranting further investigation) |
| • ST-segment depression • Pathological Q-waves • Ventricular pre-excitation • T-wave inversion beyond V1 in white athletes and beyond V4 in black athletes • Complete left bundle branch block or complete right bundle branch block • QTc ≥470 ms in males and ≥480 ms in females • Brugada-like early repolarization • Atrial or ventricular arrhythmias • ≥2 premature ventricular complexes per 10 s tracing |
The study by Sheikh et al.10 has certain limitations: although it assessed the clinical history, physical exam and ECGs of 5505 athletes (1208 black and 4297 white), the analysis was retrospective and the criteria were based on data from elite athletes, and so it is uncertain whether the findings can be generalized to nonelite athletes. Furthermore, echocardiographic data were not available in all individuals, which may have led to underestimation of the prevalence of some minor abnormalities.
Nevertheless, these findings have been confirmed in a population of male athletes (1367 Arab, 748 black and 376 Caucasian), in which the refined criteria performed better (5.3% abnormal ECGs) than the Seattle criteria (11.6%) and the ESC criteria (22.3%), all three sets presenting 100% sensitivity.9 Black athletes continue to present a higher prevalence of abnormal ECGs compared with Arab and Caucasian athletes (10% vs. 3.6% and 2.1%, respectively), although lower than by the Seattle criteria (16.6%, 9.7% and 8.5%, respectively) and the ESC criteria (29.9%, 19.1% and 18.6%, respectively).
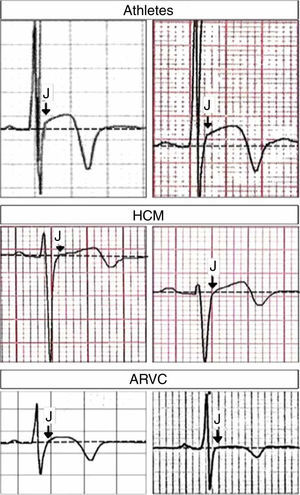
It should also be noted that after the article by Machado and Vaz Silva1 was accepted for publication, new data appeared suggesting that a combination of J-point elevation and T-wave inversion not extending beyond V4 differentiated between physiological adaptation and cardiomyopathy in this population.11 This study compared ECG patterns of T-wave inversion (≥1 mm) in ≥2 contiguous anterior leads (V1–V4) in 80 healthy athletes; 95 patients with hypertrophic cardiomyopathy (HCM), including 26 athletes; and 58 patients with arrhythmogenic right ventricular cardiomyopathy (ARVC), including nine athletes. A J-point elevation <1 mm in the anterior leads and T-wave inversion extending beyond V4 were independent predictors for both ARVC and HCM, while the combination of J-point elevation ≥1 mm and T-wave inversion not extending beyond V4 excluded these cardiomyopathies with 100% sensitivity and 55% specificity (Figure 1).11
Close-up of lead V3 in different clinical conditions. Top: J-point elevation preceding T-wave inversion (both panels from healthy athletes); middle: ST-segment elevation (without J-point elevation) preceding T-wave inversion (both panels from patients with hypertrophic cardiomyopathy); bottom: ST-segment elevation (without J-point elevation) preceding T-wave inversion (both panels from patients with arrhythmogenic right ventricular cardiomyopathy). Arrows indicate the J-point. ARVC: arrhythmogenic right ventricular cardiomyopathy; HCM: hypertrophic cardiomyopathy. Adapted from Calore et al.11 with permission from Oxford University Press.
Although Machado and Vaz Silva1 state that the exclusion of “certain ECG alterations that are still deemed abnormal even when found in isolation” could improve the false-positive rate, in view of the study by Sheikh et al.,10 it is our opinion that insufficient emphasis was given to the new refined criteria, which, although not yet incorporated into the guidelines, will in all likelihood soon be, and will help reduce false positives without compromising diagnostic sensitivity.
Please cite this article as: Rodrigues RC, Serrão G, Gomes S, Pereira D. Novos «critérios refinados» eletrocardiográficos na avaliação de atletas. Rev Port Cardiol. 2016;35:711–713.