Easy access to echocardiography and its extensive and repeated use (as is the case in Portugal) now facilitates the early diagnosis of cardiac myxoma (CM).
ObjectiveTo re-evaluate the clinical and pathological profile of CM under current diagnostic conditions.
MethodsWe performed a retrospective study of 40 patients consecutively referred for surgery (between January 2003 and January 2010) with a histologically confirmed diagnosis of CM – 26 female (F) and 14 male (M), with a mean age of 64±12 years (range 12–81; 53% over 65, 43% over 70); 39 patients were operated (one was not operable due to major neurological deficit). Clinical characteristics, surgical protocols, follow-up records of survivors (range 1–76 months, with serial echocardiograms), and histological data were reviewed.
ResultsThe apparent incidence was 2.6 cases/million/year; the overall F/M ratio was 1.9:1 (1.3:1 in those aged over 65, similar to the general population). The CM was located in the left atrium (LA) in 92.5%, with insertion in the fossa ovalis of the interatrial septum (IAS) in 53% (only 57% of LA myxomas), and outside the IAS in 30%. The mean size was 4.6cm×3.7cm. Asymptomatic tumors occurred in 48% of the total population (sessile and/or atypically inserted in 74%; 63% of large size, over 3cm×3cm), 61% were in patients referred in the last 25 months of the study; 23% of patients showed constitutional symptoms (all with very large CMs – mean 6.7cm×5.1cm), 35% had hemodynamic/obstructive symptoms, and 15% presented with embolic events. There was evidence of CM-related mitral valve (MV) disease in 20% of patients, resulting in moderate to severe mitral regurgitation requiring associated MV surgery in 13%. Significant comorbidities were present in 69%. Surgical procedures included simple excision in 74%; septoplasty/atrioplasty associated with extensive resection of the insertion site in 26%; and combined surgery (CM excision plus other procedures) in 28%. There were significant postoperative complications in 38%. In-hospital mortality was 10%; postoperative mortality was 7.7%. Mean follow-up was 30 months (100% of survivors, 44% for >2 years); late mortality was 5.6% and no CM recurrences were observed.
Conclusions(1) CM has a higher incidence than described in the literature and mainly affects patients aged over 65; the reported predominance of female patients disappears after the age of 65. (2) Most CM cases are now asymptomatic at presentation as a result of earlier diagnosis. (3) CM is the cause of MV disease requiring surgical correction in more than 10% of cases, and is associated with significant postoperative mortality, mainly due to the presence of comorbidities.
O acesso fácil à ecocardiografia (ECOCG) e o seu uso extensivo e repetido (como acontece em Portugal) facilitará atualmente o diagnóstico precoce dos mixomas cardíacos (MC).
ObjetivoReavaliar os perfis clínico e anatomopatológico dos MC à luz das actuais condições diagnósticas.
Material e métodosEstudo retrospetivo de 40 doentes (dts) consecutivamente propostos para cirurgia (entre janeiro 2003 e janeiro 2010), com o diagnóstico confirmado histologicamente de MC – 26 dts do sexo feminino (F) e 14 do sexo masculino (M), com idade média de 64+-12 anos (12-81; 53% com > 65 anos, 43% com > 70 anos); 39 dts foram operados (um dt inoperável, por sequelas neurológicas major). Efetuou-se a revisão das características clínicas dos dts, dos protocolos operatórios e do seguimento (1-76 meses, com ECOCG seriada) dos sobreviventes, e ainda dos dados histológicos.
Resultados1) Incidência aparente de 2,6 casos/milhão/ano; relação F/M (global)= 1,9:1; relaçãoF/M (dts com > 65 anos)= 1,3:1 (sobreponível à da população geral). 2) Localização: aurícula esquerda (AE) em 92,5% dts; inserção na fossa ovalis do SIA (AE) em 53% dts (apenas 57% dos MC da AE) e fora do SIA em 30% dts. Tamanho médio=4,6x3,7cm 3). Dts assintomáticos – 48% (MC séssil e/ou com inserção atípica em 74% dos casos; 63% com dimensão > 3x3cm), sendo 61% nos últimos 25 meses; 23% com sintomas constitucionais (MC sempre muito volumoso – média de 6,7x5,1cm), 35% com sintomas hemodinâmicos/obstrutivos e 15% com fenómenos embólicos (83% dts com MC viloso; todos com localização atípica; 83% com MC volumoso). 4) Presença de patologia da válvula mitral (VM) relacionada diretamente com o MC em 20% dts, resultando em insuficiência mitral moderada/grave, com indicação para cirurgia VM associada, em 13% dts. 5) Comorbilidades significativas em 69% dts. 6) Protocolo operatório: excisão simples - 74% dts; septoplastia/atrioplastia associada à excisão alargada da base do MC – 26% dts; cirurgia combinada (ressecção do MC + outros procedimentos) – 28% dts. Complicações pós-operatórias significativas: 38% dts. Mortalidade hospitalar global: 10% (4 dts); mortalidade pós-operatória global=7,7% (3 dts; 2,6% aos 30 dias). 7) Seguimento pós-operatório (100% dts; média de 30 meses, 44% com mais de 2 anos): mortalidade tardia – 5,6% (2 dts); ausência de recorrência de MC.
Conclusões1) O MC tem uma incidência superior à estimada na bibliografia clássica e afeta maioritariamente dts com mais de 65 anos. O proclamado predomínio no sexo feminino desaparece acima dos 65 anos. 2) Atualmente, a maioria dos MC apresenta-se na forma assintomática, como consequência de um diagnóstico muito mais precoce. 3) O MC associa-se diretamente a patologia valvular mitral merecedora de correção cirúrgica em mais de 10% dos casos e tem uma mortalidade pós-operatória relevante, marcada pela influência das comorbilidades.
Cardiac myxoma (CM) has conventionally been considered to have an incidence of 0.5 cases/million/year,1 to be symptomatic in 75–90% of cases2–6 (constitutional symptoms in 30–90%,4,6 embolic events in 16–50%2–4,6 and hemodynamic/obstructive symptoms in 40–60%2,3,6), to be more common in women, and inserted in the fossa ovalis (left atrial side) of the interatrial septum (IAS) in 64–85% of patients.2,7 There is some disagreement as to the mean age of patients at diagnosis: in the US, Burke et al. (2001–2007) and McManus et al. (2008) reported that most patients present between the ages of 30 and 60 (mean: 50 years),1–3 while in Europe, Thiene et al. (2009) found that the peak occurs in those aged over 60 years.6
Easy access to echocardiography and its extensive and repeated use (as is the case in Portugal), particularly in hypertensive and/or diabetic patients, now facilitates the early diagnosis of CM.
ObjectiveThe aim of this study is to re-evaluate the clinical and pathological profile of CM under current diagnostic conditions.
MethodsWe performed a retrospective observational study of 40 patients consecutively referred for surgery between January 2003 and January 2010 (85 months), with a histologically confirmed diagnosis of CM – 26 female (F) and 14 male (M), mean age 64±12 years (range 12–81; 53% over 65 and 43% over 70). Twenty-two patients were referred for surgery in the first 60 months of the study, while 18 were referred in the last 25 months. Thirty-nine were operated (18, 45% of the total, in the last 25 months of the recruitment period) and the diagnosis of CM was confirmed by anatomopathological study of the surgical specimens. One case was considered inoperable due to major neurological deficit (the CM was manifested by multiple systemic emboli followed by major stroke and occlusion of the abdominal aortic bifurcation) but the diagnosis was confirmed by anatomopathological study of the emergency aortic embolectomy specimen. Clinical characteristics, surgical protocols and postoperative follow-up records of survivors (range 1–76 months, with serial echocardiographic assessment every one or two years) were reviewed, together with available anatomopathological data.
Fisher's exact test was used to analyze discontinuous variables.
ResultsIn the period immediately prior to our study (1985–2002), the annual mean number of cases of CM admitted to our cardiothoracic surgery department was 2.3 (range: 0–5). During the study period, this figure rose to 5.6 cases per year (range: 3–9), which is a dramatic increase even bearing in mind that the area from which patients were referred to our department became much larger.
Based on the demographic characteristics of the geographical area currently served by our department (a third of Greater Lisbon and large areas of districts to the north and south of the River Tagus, with a total population of around two and a half million), the apparent overall incidence of CM for the period 2003–2009 was 2.6 cases/million/year. During the first 60 months of the recruitment period, the apparent incidence was 1.8 cases/million/year, but this almost doubled to 3.5 cases/million/year for the last 25 months of the study period.
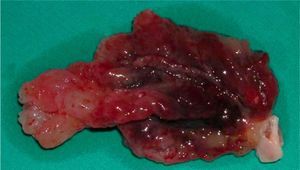
The overall F/M ratio was 1.9:1, falling to 1.3:1 in those aged over 65 (similar to that reported for the general population – 1.4:18).
Anatomical dataThe CM was located in the left atrium (LA) in 37 patients (92.5%), in the right atrium in two (5%), and in the left ventricle (inserted in the posterior papillary muscle of the mitral valve [MV]) in one (2.5%). Insertion was in the fossa ovalis (left atrial side) in 53% of cases (but only 57% of LA myxomas had this typical presentation) and outside the IAS in 30%. The CM stalk was short and wide or nonexistent (sessile) in 16 patients (40%). Macroscopically, the CM presented a villous surface (papillary or pseudopapillary anatomical substrate) in 35% of cases (14 patients) (Figure 1); in the others, the tumor was ovoid or spherical, with a smooth surface (Figure 2). The mean size of the tumors was 4.6cm×3.7cm.
Clinical manifestationsAround half the patients were asymptomatic (19 cases, 48%) at the time of diagnosis. However, the prevalence of asymptomatic patients rose dramatically from 36% (8/22) in the first 60 months of the recruitment period to 61% (11/18) in the last 25 months. The diagnosis was made during routine transthoracic echocardiography in 15 of the 19 asymptomatic patients (confirmed by transesophageal echocardiography in one and by cardiac magnetic resonance imaging in two), by goal-directed transesophageal echocardiography in two (assessment of aortic stenosis in one and investigation of stroke due to paradoxical embolism in the other), and by chest computed tomography in two (during investigation of chronic cough caused by severe gastroesophageal reflux in a 75-year-old patient with asymptomatic chronic atrial fibrillation, previously considered idiopathic, and of chronic obstructive pulmonary disease complicated by hemoptysis in a 60-year-old man). Although asymptomatic, these tumors were large (over 3cm×3cm) in 63% of patients, and were sessile or equivalent (non-mobile, with short wide stalks) in 53% of these cases (10 patients); they were pedunculated, with atypical insertion (not in the LA side of the fossa ovalis) in three of these patients (16%); only 26% of asymptomatic patients (5/19) presented mobile pedunculated tumors with typical insertion.
Nine patients (23%) showed constitutional symptoms (fatigue on minimal exertion, weakness, intermittent mild fever, anorexia or weight loss), or equivalent signs (mild normocytic anemia or elevated erythrocyte sedimentation rate and/or C-reactive protein) not explained by comorbidities, that had begun from a few months to around three years previously. All had large CMs (mean of 6.7cm×5.1cm). Fourteen patients (35%) had hemodynamic/obstructive symptoms, beginning between 24hours (in a patient presenting with paroxysmal atrial fibrillation) and a few days previously (in a patient with acute left ventricular failure resulting from acute severe mitral regurgitation due to chordal rupture) to more than a year. Embolic events occurred in only 15% (6 patients), all with atypical CM insertion; the tumors were large in 83% of these cases (5/6) and had a villous surface in 83% (5/6); in five of these six patients, the embolic event was the first clinical manifestation of CM, and the tumor was large in four of these five cases.
There was evidence or clinical suspicion of arrhythmias in six patients (15%) (included in the group with hemodynamic symptoms), five of whom were aged over 70. Three patients had atrial fibrillation (paroxysmal in one and sustained in two, being considered chronic – over a year's duration – in one of the latter), all with CM-related valve disease; there was a strong suspicion in three other patients (not documented electrocardiographically) of recurrent salvos of paroxysmal tachyarrhythmia, possibly atrial. In a third of these cases (2 patients), the arrhythmic manifestations were the only symptoms of CM. The atrial electrogram revealed abnormalities (intra-atrial block) in only two of the five patients with baseline sinus rhythm. The CM was inserted in the IAS in four patients and in or near the mitral annulus in the other two.
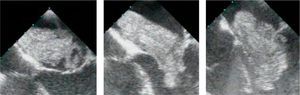
CM-related valve diseaseThere was evidence of CM-related MV disease in 20% of cases (8 patients, with a mean age of 63 years but a wide range): five due to trauma caused by a mobile CM protruding through the MV into the left ventricle in diastole (Figures 3 and 4), probably weakening the valve itself or the mitral annulus; two, with a CM in or near the mitral annulus, due to deformation of the mitral annulus caused by the drag exerted by the tumor; and one, with CM insertion in the posterior papillary muscle of the MV (mobile and partially obstructing the left ventricular outflow tract during systole), due to deformation of the valve apparatus in systole. All had mitral regurgitation, which was moderate or severe, with indication for surgery, in five patients (63% of those with MV dysfunction and 13% of the total study population), and two patients had chordal rupture of the anterior leaflet, representing 5% of cases in our series and 1.6% of all patients with normal coronary arteries operated for chordal rupture of the mitral apparatus during the study period.
Sequence (left to right) of transesophageal echocardiographic video images showing diastolic motion of a large solid myxoma, protruding into the left ventricle through the mitral valve apparatus in a movement resembling a piledriver, causing structural and functional changes to the valve resulting in intermittent mitral regurgitation.
There were significant comorbidities in 69% of patients operated, including type 2 diabetes in 31%, chronic renal failure (mild or moderate) in 18% and coronary artery disease in 10%. In one case CM was associated with papillary fibroelastomas, in a 64-year-old woman with a history of chronic pulmonary microthromboembolism admitted for embolic stroke, and diagnosed as paradoxical embolism due to patent foramen ovale, in whom transthoracic echocardiography showed an asymptomatic pedunculated CM, measuring 4cm×4cm, inserted in the LA posterior wall, and intraoperative transesophageal echocardiography revealed two small (<1cm maximum diameter), asymptomatic, papillary fibroelastomas of the left coronary and non-coronary cusps of the aortic valve. The prevalence of hypertension in this population was 60%.
Surgical proceduresSimple excision of the tumor was performed in 74% of patients with atrial CM, while septoplasty or atrioplasty was performed in the other 26%, together with extensive resection of the insertion site (not because of the surgeon's preference but for technical reasons in cases of sessile or wide-stalked CMs and tumors that were difficult to access). In the case of the CM inserted in the posterior papillary muscle of the MV, tumor excision was accompanied by resection of the papillary muscle. CM excision was combined with other procedures in 28% of cases, including MV surgery in six patients (valve replacement in three, two mechanical and one biological prosthesis, mitral valvuloplasty in two, and mitral commissurotomy in one patient with a history of rheumatic mitral disease), myocardial revascularization in three, foramen ovale closure in four, and aortic valve surgery in two (valve replacement in one case of severe aortic stenosis and asymptomatic CM, and leaflet shaving in the patient with associated papillary fibroelastomas). There were significant postoperative complications in 38% of cases, and overall postoperative mortality was 7.7% (2.6% at 30 days). Nine patients (28%) had arrhythmias in the postoperative period; the incidence of atrial fibrillation was twice as high in patients with CM excision associated with valve surgery compared to those undergoing simple tumor resection (38% vs. 19%), while the combination of septoplasty or atrioplasty with extensive resection of the CM insertion site did not appear to increase the risk of arrhythmias (1/7 patients with postoperative atrial fibrillation).
Overall in-hospital mortality was 10% (four patients, including the inoperable case). Causes of death were: (a) extensive embolic stroke (inoperable patient); (b) staphylococcal sepsis (on the 11th postoperative day in a 63-year-old diabetic patient); (c) multiple organ failure (on the 40th postoperative day, following sepsis complicating acute liver and renal failure in a 66-year-old patient with chronic alcoholic liver disease); and (d) multiple organ failure (on the 89th postoperative day following a series of major complications – sepsis with aortic valve bacterial endocarditis, ischemic stroke and nosocomial pneumonia – in a 75-year-old patient).
Follow-upMean follow-up was 30±24 months in survivors discharged from hospital (36 patients), with 44% followed for >2 years. There were no recurrences of CM or suspected cases of familial CM. Late mortality was 5.6% (two patients): one patient died 13 months after surgery following worsening neurological sequelae of a major preoperative stroke; and a kidney transplant patient died three months after undergoing combined surgery (CM resection, aortic valve replacement and myocardial revascularization) as a result of MRSA sepsis. No other cardiovascular events were recorded, with the exception of recurrent atrial fibrillation in the patient who presented with transient sustained atrial tachyarrhythmia.
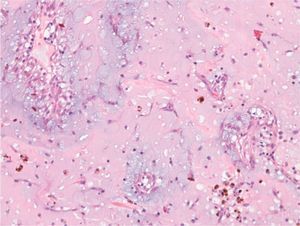
Histological dataThe histological characteristics observed in this series of 40 patients were those usually described for this entity9–12: elongated spindle, stellate, and polygonal mesenchymal cells in a myxoid stroma (Figure 5). Myxoma cells contain only a moderate amount of eosinophilic cytoplasm, with oval, round or elongated nuclei, and typically mitosis is rare. Cellularity is variable, with isolated cells in small clusters, cords or rings, the latter frequently surrounding vessels, in single or multiple layers. The most common patterns observed in our population were perivascular or small clusters. There was one case of epithelioid glandular structures, and another resembling multinucleated giant cells, but these may have been cell clusters.
In addition to CM cells, macrophages, lymphocytes, plasmocytes, polymorphonuclear leukocytes, dendritic cells and mast cells are frequently observed in varying numbers, as well as fibroblasts, myofibroblasts and smooth muscle cells. In our series, the inflammatory infiltrate was predominantly lymphocytic/plasmocytic, together with neutrophils in 13 and eosinophils in four patients; inflammation was moderate to severe in 16 cases (40%) and mild or absent in the remainder.
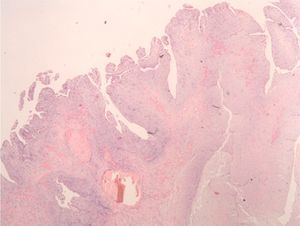
The myxoid stroma is positive for Alcian blue as it contains acid mucin and can include varying amounts of collagen and elastin. There is generally abundant vascularization, and the vessels may lack pericytes or be cavernous. It is common to find extravasation of erythrocytes, hemorrhagic foci (recent or organized), hemosiderin deposits (extra- and intracellular), Gamna-Gandy bodies and cystic areas. In our study population, there was moderate to severe bleeding in 30 cases (75%, extensive in 32.5% of tumors), and mild or no bleeding in the remainder. Two cases had extramedullary hematopoiesis; there were calcifications in four patients and ossification in two.
The tumors are usually covered with a single layer of flat cells, but the outer layer may be stratified with small buds. Thrombi are frequently found adhering to the tumor surface. In our series, an at least partly papillary or villous surface (Figure 6) was observed in 14 cases (35%).
Clinicopathological correlationThere was a significant correlation between embolic complications and a papillary or villous tumor surface (p<0.05), but no association between such complications and CM size, presence and extent of bleeding or inflammatory infiltrate. There was a significant association between constitutional symptoms and tumor size (p<0.05), but not between these and extent of inflammatory infiltrate.
Extensive bleeding may be the consequence of chronic trauma caused by the tumor, particularly since 45% of cases had extremely mobile CMs, protruding into the underlying ventricular chamber in diastole through an atrioventricular valve. With a repetitive motion, particularly in the case of a solid tumor, which on transesophageal echocardiography resembles a piledriver, the mass strikes the valve apparatus, which can cause two-way trauma (the tumor against the valve and the valve annulus against the tumor). Nevertheless, no association was found between extensive bleeding and highly mobile atrial CMs protruding into the ventricle: extensive bleeding was present in only 26% of such tumors, as opposed to 47% of cases with completely or relatively immobile CMs (sessile or with short, wide stalks). Furthermore, extensive bleeding did not occur more frequently in CMs with a friable (29%) or gelatinous (18%) appearance. The lack of correlation between major or extensive bleeding and particular clinical or morphological characteristics is in fact to be expected since these tumors have a tendency to bleed due to their high proportion of angioblasts.6
DiscussionExtrapolating our results to calculate the apparent overall incidence of CM in Portugal suggests that it has been greatly underestimated in the past, since there are no new etiopathogenic or epidemiological factors that would lead to a real increase in incidence. Although not impossible, it is unlikely that the referral rate to our department increased progressively over the study period, and analysis of the provenance of our CM patients did not reveal any difference in geographical distribution compared to patients with coronary or valve disease referred for surgery to our department in the same period. On the other hand, in parallel with the sharp rise in the annual incidence of CM in the last two years of the study period there was also a significant increase in the prevalence of asymptomatic CM. This clearly points to an increase in the number of cases diagnosed, mainly asymptomatic individuals, in whom use of cardiac imaging techniques for whatever reason revealed the unexpected finding of an intracardiac mass. These results are not surprising given that general practitioners have increasingly referred patients for echocardiography in recent years. We therefore believe that health centers’ relatively easy access to echocardiography and its extensive and repeated use, particularly in hypertensive, diabetic and elderly patients, is the main reason for the increased number of cases of CM diagnosed in recent years. The high prevalence of hypertension and diabetes in our series and the fact that over half of patients were over 65 years old tend to support this hypothesis.
We suspect that the clinical course of most undiagnosed CMs in the past would have been as follows: constitutional symptoms would have appeared and were not given due weight and/or hemodynamic/obstructive symptoms were mistakenly interpreted to be the result of comorbidities, particularly in elderly individuals, which progressed until they caused a cardiovascular event (embolic or otherwise) that was either terminal or presaged a probably fatal recurrence. This would be particularly true of elderly patients in whom, given the overall clinical picture, the cardiovascular event would not be thoroughly investigated, particularly in terms of imaging studies (for example, stroke would not prompt echocardiographic assessment as frequently as it does today) and the presence of an intracardiac mass would not be detected or, if it were, the finding would not necessarily lead to further investigation and referral for surgery. CM was only sporadically diagnosed on autopsy.
The increase in the number of cases of asymptomatic CM over the study period, becoming the most common form in its last two years, is in stark contrast to the data found in the literature.2–6 The fact that around half of the patients in our series were asymptomatic points to generally earlier diagnosis. As our study shows, early diagnosis of CM results in a markedly lower number of cases associated with embolic events, as well as a significant reduction in the prevalence of constitutional symptoms, as the latter are caused by the production of cytokines, especially interleukin-6, by CM cells,1,6 and clearly indicate the presence of a large longstanding CM. However, if early diagnosis is used to refer to CMs of recent evolution and hence of relatively small size, the number of asymptomatic cases meeting this criterion in our series was small, only seven patients (18%).
CMs are diagnosed with increasing frequency in elderly patients; the reported predominance of female patients disappears after the age of 65, which may well have a genetic basis, possibly a specific braking mechanism of CM precursor cells in men, which no longer functions at advanced ages.
CM-related MV disease, only occasionally mentioned in the literature,14 was unexpectedly common in our series, requiring valve surgery together with CM resection in over 10% of cases. Advanced age and concomitant calcific MV disease do not explain this and it is likely that the cause lies in fragility of the MV or annulus; ethnicity may be a factor.
Our series included one case, described above, of CM associated with multiple papillary fibroelastomas of the aortic valve. The association of heterogeneous cardiac tumors is extremely rare; all cases have been of CM with papillary fibroelastoma.15 To the best of our knowledge, this is the sixth reported case.15–18
Documented or suspected tachyarrhythmias in patients with CM is not a common clinical finding in the preoperative phase. Most involve elderly patients and those with associated mitral disease.
Typical CM insertion in the left atrial side of the fossa ovalis was far less common in our series than expected (only around half of cases), insertion outside the IAS being observed in 30% of patients. The reason for this is unclear.
The diagnosis is usually confirmed histologically after total surgical excision of the tumor. Differential diagnosis can include various entities,13 but focuses mainly on distinguishing between CM and thrombus, the latter being characterized by local fibrin deposition and the absence of myxoma cells. Other conditions that may be confused with CM include: myxoid sarcoma, which presents pleomorphic spindle cells, abundant mitosis and absence of hemosiderophages; papillary fibroelastoma (on valves, with avascular papillae covered by endothelium); calcified amorphous tumor (CAT), with extensive calcification and absence of myxoma cells; mesothelial/monocytic incidental cardiac excrescence (MICE), with no myxoid stroma, in patients with a history of cardiac intervention; fibroma (typically located in the ventricle, with abundant collagenous stroma); intracavitary hemangioma (characterized by absence of myxoid stroma and a lobular arrangement of vessels, surrounded by pericytes positive for actin); and metastatic carcinoma (which can mimic a rare form of CM rich in glandular structures). Immunohistochemical study can also provide useful information for differential diagnosis: CM cells are positive for calretinin in 75–100% of cases, but have variable positivity for vimentin, alpha-1-antichymotrypsin, alpha-1-antitrypsin, S100 protein, smooth muscle actin, desmin, synaptophysin, NSE and endothelial markers; only epithelioid structures (corresponding to heterologous elements) may be positive for epithelial markers (AE1/AE3, CAM5.2, CK34βE12, CK7, CK20, EMA and CEA).13
Postoperative prognosis is highly variable, depending mainly on the patient's age, presence of significant comorbidities (in over two-thirds of our patients), preoperative clinical status and need to combine additional surgical procedures with CM resection (the case in 30% of our patients). Our population was made up of high-risk patients, reflected in overall postoperative mortality of around 8%, the result of noncardiovascular complications in all cases. The overall prevalence of postoperative atrial tachyarrhythmias in our series was no higher (around 30%) than that reported for isolated coronary surgery in patients of the same age-group; unexpectedly, the combination of septoplasty or atrioplasty with extensive resection of the CM insertion site did not increase the risk of atrial arrhythmias.
Beyond the postoperative period, the medium- to long-term prognosis (in a mean follow-up of 30 months) was good for survivors without serious chronic comorbidities, with no CM recurrences.
Based on all that has been said above, it seems clear that at the beginning of the 21st century, the clinical aspects of CM are changing in Portugal. This is due to a radical change in the use of noninvasive diagnostic cardiac imaging techniques in clinical practice, which, as a result of easy access and extensive and repeated use, have enabled early diagnosis of many cases of CM, a substantial number of which might otherwise never have been detected. As a result, most CMs are now clinical findings in asymptomatic patients. Surgical centers receiving CM patients referred for surgery have seen an increase in apparent incidence but fewer cases associated with embolic events or constitutional symptoms. A new clinical paradigm is thus emerging of patients with CM – elderly, no predominant gender, asymptomatic, and frequently with serious comorbidities that increase surgical risk, resulting in significant operative mortality (mainly from noncardiovascular causes).
ConclusionsThe incidence of CM in Portugal is considerably higher than reported in the literature. Most patients are aged over 65 at the time of diagnosis and the predominance of female patients observed in younger individuals disappears in this age-group. Most CMs are now asymptomatic at presentation (a finding on imaging studies), as a result of earlier diagnosis. The classic constitutional symptoms exhibited by patients with large longstanding CMs are now much less frequent.
CM-related MV disease is not uncommon and requires surgical correction together with tumor excision in more than 10% of cases.
Postoperative prognosis is strongly influenced by comorbidities and age, with significant postoperative mortality (around 8% in our series).
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Bordalo ÁDB, et al. Terão os mixomas cardíacos uma nova face clínica? Estudo de reavaliação clínico-patológica. Rev Port Cardiol. 2012. http://dx.doi.org/10.1016/j.repc.2012.05.008.