Coronary to pulmonary fistula is an uncommon cardiac anomaly seen in 0.05-0.25% of patients undergoing diagnostic coronary angiography. Coronary artery fistulae are usually asymptomatic but larger and multiple fistulae can lead to ischemia, congestive heart failure, myocardial infarction and pulmonary hypertension. Although usually congenital, they may be acquired. They most frequently arise from the right coronary artery system (55%), less often from the left coronary artery system (35%), and rarely from both coronary arteries (5%). The most common locations into which they drain are, in decreasing order, the right ventricle, right atrium, pulmonary artery, coronary sinus, left atrium, left ventricle, and superior vena cava. Although most fistulae are single, multiple fistulae have been reported. The most common type of coronary artery fistula in one study was to the pulmonary artery, but multiple fistulae of all three coronary arteries to the pulmonary artery and concomitant anomalous coronary origin have not been previously reported. We present a rare case of a symptomatic patient with congenital multiple coronary arteriovenous fistulae originating from the left anterior descending artery (LAD), left circumflex artery (LCX) and right coronary artery (RCA) draining into the pulmonary artery, and concomitant anomalous coronary origin, with the LCX arising from the right coronary system.
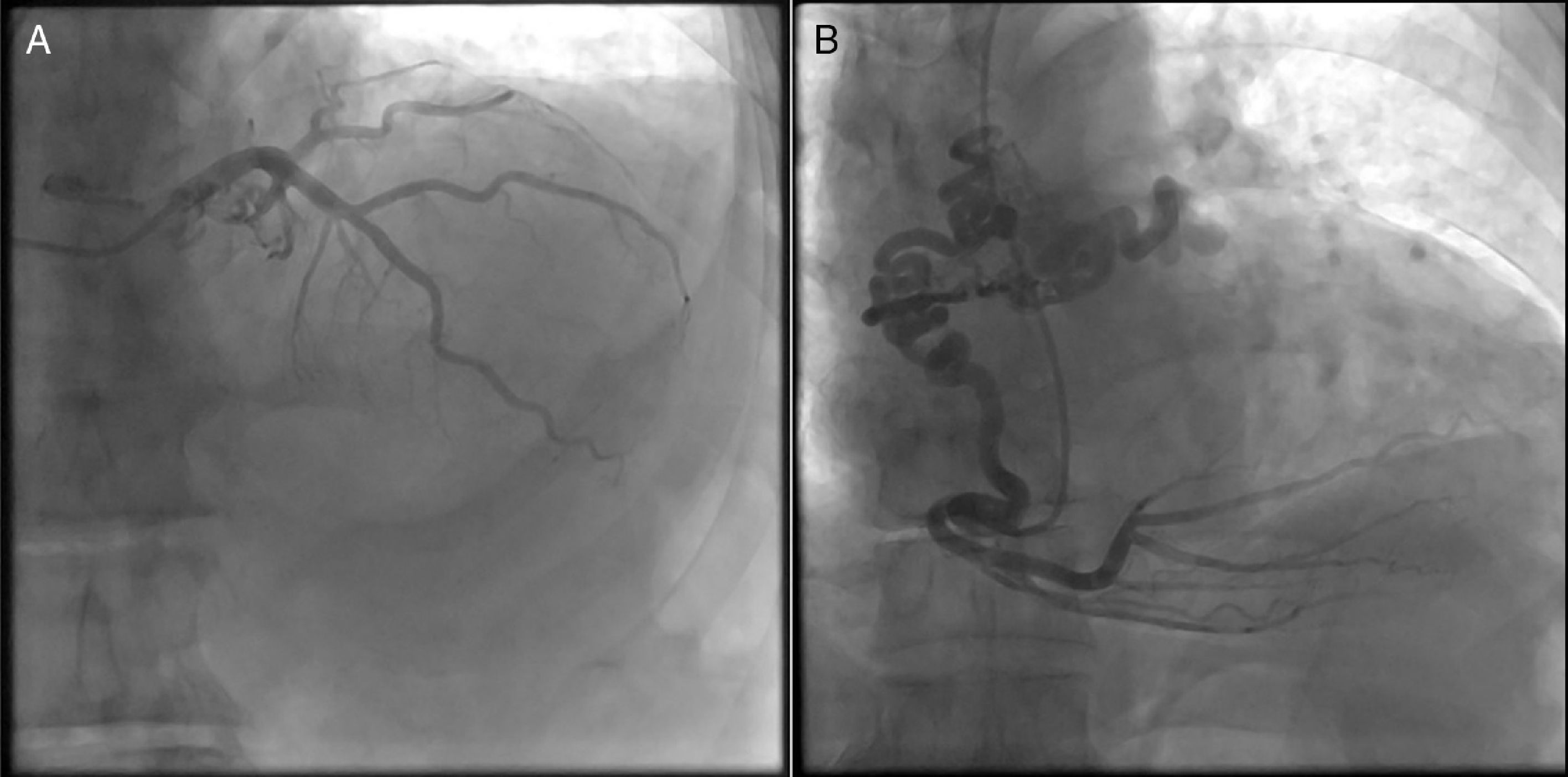
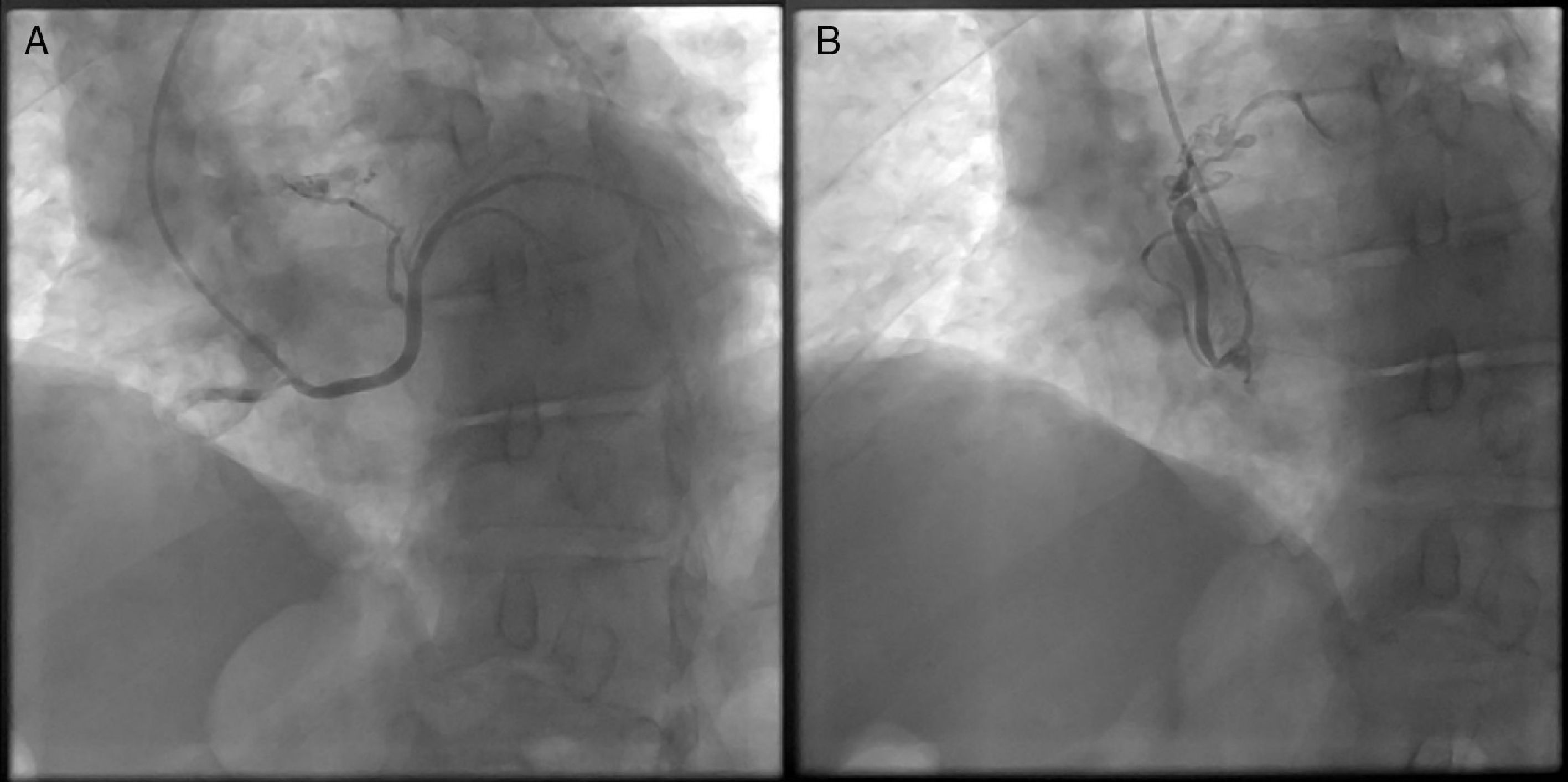
A 65-year-old man was admitted with severe dyspnea and typical chest pain. Clinical examination revealed a grade 2 continuous murmur in the mesocardiac area. His medical history included hypertension and dyslipidemia as risk factors for coronary artery disease. A standard 12-lead electrocardiogram revealed no significant alterations. Transthoracic echocardiography demonstrated impaired left ventricular relaxation, left ventricular ejection fraction of 65%, no significant valvular disease and pulmonary artery systolic pressure of 45 mmHg. Subsequently, coronary angiography showed multiple fistulae of all three coronary arteries, which drained into the pulmonary artery (Figure 1A and B) and concomitant coronary anomaly with the LCX originating from the right coronary system (Figure 2A). Furthermore, the RCA was the origin of fistulae in two different locations, at mid level and the conus branch (Figure 2B). We recommended percutaneous coil embolization and a vascular plug for the fistulae but the patient refused interventional treatment, so he was given optimal medical treatment (beta-blockers and anti-hypertensive and lipid-lowering medication).
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.