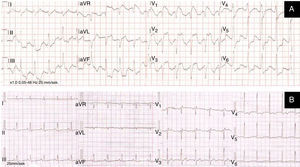
A 50-year-old man with long-standing type 1 diabetes was admitted directly to the cardiac catheterization laboratory with a preliminary diagnosis of ST-segment elevation myocardial infarction (STEMI). He presented with chest discomfort and vomiting. The initial ECG transmitted from an ambulance showed sinus tachycardia, prominent ST-segment elevation in V1–V3 and aVR and ST-segment depression in leads II, III, aVF and V5–V6 (Figure 1A).
Prompt coronary angiography documented normal coronary arteries. Echocardiography excluded left ventricular wall motion abnormalities.
Laboratory tests revealed hyperglycemia (80.2 mmol/l, 1444 mg/dl), metabolic acidosis (pH 7.18), hyperkalemia (6.2 mmol/l), hyponatremia (118 mmol/l), ketonemia, non-significantly elevated high-sensitivity troponin (up to 210 pg/ml) and increased creatinine (272 μmol/l, 3.08 mg/dl).
A diagnosis of diabetic ketoacidosis was ultimately made. The precipitating event was found to be excessive alcohol intake several days before. The ST-segment changes disappeared after normalization of water-electrolyte and acid-base imbalances (Figure 1B). The patient was discharged on the sixth day after full recovery.
Direct and immediate transport to the nearest catheterization laboratory when paramedics diagnose STEMI is beneficial for most patients, nevertheless it may pose a serious threat to patients with a pseudo-myocardial infarction ECG pattern.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.