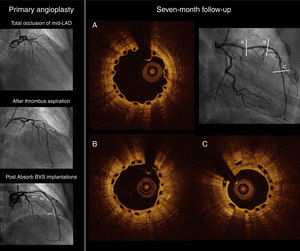
A 44-year-old female was admitted for an anterior ST-segment elevation myocardial infarction (STEMI) and emergency coronary angiography revealed total occlusion of the mid segment of the left anterior descending artery (LAD). After thrombus aspiration, intracoronary nitrate administration and balloon predilatation, two overlapping Absorb™ bioresorbable vascular scaffolds (BVS) (3 mm×18 mm and 2.5 mm×28 mm; Abbott Vascular, Santa Clara, CA, USA) were implanted in the proximal, mid and distal LAD segments. A more distal obstructive lesion was treated with a 2.5 mm×18 mm Absorb™ BVS (Abbott Vascular, Santa Clara, CA, USA).
Seven months later, the patient was admitted with anemia (hemoglobin 7.9 g/dl) associated with subacute genital tract bleeding. In order to improve risk stratification of temporary discontinuation of dual antiplatelet therapy (DAPT), intracoronary imaging was performed. Optical coherence tomography (OCT) showed fully covered scaffolds with good apposition (Figure 1). Neointimal coverage was heterogeneous with an asymmetric distribution around the circumference of the vessel wall. Furthermore, neointimal hyperplasia was more marked in the distal segments, possibly because the hemodynamic microenvironment and endothelial shear stress are involved in its regulation.
This case suggests the feasibility of implanting several BVS in long lesions of the culprit vessel in STEMI patients, achieving optimal results even without intracoronary imaging guidance at primary PCI. Assessment of scaffold endothelialization on OCT study influenced therapeutic decisions in this particular setting, as there are few data related to the minimum duration of DAPT after BVS implantation.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.