While cardiac amyloidosis (CA) is a rare systemic disease characterized by extracellular deposition of protein-derived fibrils, hypertrophic cardiomyopathy (HCM) is histopathologically characterized by myocyte hypertrophy and disarray, interstitial fibrosis, and small intramural coronary arteriole dysplasia. The aim of the present study was to compare left atrial (LA) volumetric and functional characteristics between light-chain (AL) CA and HCM by three-dimensional (3D) speckle-tracking echocardiography (STE).
MethodsThe AL-CA group initially consisted of 17 patients with AL-CA, but one patient was excluded due to inadequate image quality, and so the study population consisted of 16 patients (mean age: 64.0±9.6 years, five men). Their results were compared with data on 20 age-matched HCM patients (mean age: 59.8±5.2 years, 10 men) and on 16 age-matched healthy controls (mean age: 58.2±7.2 years, six men). Complete two-dimensional Doppler echocardiography and 3D-STE were performed in all cases.
ResultsSignificantly increased LA volumes were observed in both AL-CA and HCM compared with the control group. Only active atrial emptying fraction was found to be significantly reduced in AL-CA patients compared to controls. Peak global and mean segmental circumferential, longitudinal and area strains showed significant reductions in AL-CA patients compared with controls, but only peak mean segmental longitudinal strain differed significantly between HCM patients and controls. While no differences were demonstrated in global and mean segmental strain at atrial contraction between HCM patients and controls, AL-CA patients showed reductions in certain strain parameters compared to controls and HCM patients.
ConclusionsDifferent patterns of LA functional characteristics were demonstrated in AL-CA and HCM patients by 3D-STE.
A amiloidose cardíaca (CA) é uma doença sistémica rara, caracterizada pela deposição extracelular de fibrilhas derivadas das proteínas; por outro lado, a miocardiopatia hipertrófica (HCM) é caracterizada do ponto de vista histopatológico por hipertrofia e desorganização dos miócitos, fibrose intersticial e displasia das pequenas arteríolas coronárias intramurais. No presente estudo fomos comparar as características volumétricas e funcionais da aurícula esquerda (AE) entre a CA de cadeias leves (AL) e a HCM com ecocardiografia speckle-tracking tridimensional (3DSTE).
MétodosA população do estudo foi constituída por 17 doentes com AL-CA, foi excluído um doente por deficiente qualidade de imagem. Desse modo, o grupo final de AL-CA consistiu em 16 doentes (média de 64,0 ± 9,6 anos, cinco homens). Os resultados desse grupo foram comparados com os de 20 doentes com HCM emparelhados por idade (idade média: 59,8 ± 5,2 anos, 10 homens) e com 16 controlos saudáveis igualmente emparelhados por idade média: 58,2 ± 7,2 anos, seis homens). Em todos os doentes foi feito ecocardiograma Doppler bidimensional e 3DSTE.
ResultadosOs volumes da AE foram significativamente maiores nos doentes com AL-CA e com HCM comparados com o grupo controlo. Apenas a fração de esvaziamento auricular ativo foi significativamente mais baixa nos doentes com AL-CA em comparação com o grupo de controlo. Apesar de os strains de pico e médio segmentares, circunferenciais, longitudinais e em área serem significativamente mais baixos nos doentes com AL-CA por comparação com o grupo controlo, apenas o strain longitudinal segmentar médio de pico foi significativamente diferente entre os doentes com HCM e os do grupo de controlo. Apesar de não ter sido possível demonstrar diferenças no strain segmentar global e médio entre os doentes com HCM e o grupo de controlo, no caso dos doentes com AL-CA observou-se redução em alguns parâmetros de strain por comparação quer com o grupo de doentes com HCM quer com o grupo de controlo.
ConclusãoFoi possível demonstrar a presença de diferentes padrões funcionais da AE por 3DSTE em doentes com amiloidose cardíaca e miocardiopatia hipertrófica.
While cardiac amyloidosis (CA) is a rare systemic disease characterized by extracellular deposition of protein-derived fibrils,1 hypertrophic cardiomyopathy (HCM) is a relatively common genetic cardiac disease histopathologically characterized by myocyte hypertrophy and disarray, interstitial fibrosis, and small intramural coronary arteriole dysplasia.2 CA and HCM are both known to be associated with left atrial (LA) dysfunction. Three-dimensional (3D) speckle-tracking echocardiography (STE) has been demonstrated to have unique potential for detailed ventricular and atrial volumetric and functional analysis.3 The specific aim of this study was to compare volumetric and functional characteristics of the left atrium between light-chain (AL) CA and HCM by 3D-STE.
MethodsSubjectsThe AL-CA group initially consisted of 17 patients with AL-CA, but one patient was excluded due to inadequate image quality, and so the study population consisted of 16 patients (mean age: 64.0±9.6 years, five men). Their results were compared with data on 20 age-matched HCM patients (mean age: 59.8±5.2 years, 10 men) and on 16 age-matched healthy controls (mean age: 58.2±7.2 years, six men). The diagnosis of AL-CA was confirmed by biopsy in all CA cases. The first positive biopsy site was the myocardium in four cases, bone marrow in three, the duodenum in one, the salivary gland in one, the colon in one, the rectum in one, the kidney in four and skin and subcutaneous tissue in three cases (there were 2 confirmation sites in 2 patients). AL amyloidosis was diagnosed in patients with multiple myeloma in 12 cases, with plasma cell dyscrasia in one case, with marginal zone lymphoma in one case and with nephrotic syndrome in two cases. In these patients, in whom the histopathological report confirmed the diagnosis of AL amyloidosis, two-dimensional (2D) echocardiography was performed. If cardiac involvement with AL amyloidosis was suspected according to the data below, 3D-STE was performed. AL-CA was defined in accordance with current consensus criteria and practice.4,5 Current guidelines were also used for diagnosis of HCM.6 Hypertrophy proved to be asymmetric and septally located in all HCM patiens. Healthy subjects met the following criteria: no history of cardiac symptoms, hypertension, diabetes or hypercholesterolemia, not under medication, and normal physical examination, electrocardiogram (ECG) and echocardiogram. Complete 2D Doppler echocardiography with 3D-STE-derived data acquisition were performed in all patients and healthy subjects. The results are included in the Motion Analysis of the heart and Great vessels bY three-dimensionAl speckle-tRacking echocardiography in Pathological cases (MAGYAR-Path) study (‘Magyar’ means ‘Hungarian’ in the Hungarian language), carried out to examine the diagnostic and prognostic value of 3D-STE-derived parameters in different disorders. Informed consent was obtained from all subjects, the study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki, and the institution's human research committee approved the study.7
Two-dimensional echocardiographyA commercially available ultrasound system (Toshiba ArtidaTM, Toshiba Medical Systems, Tokyo, Japan) equipped with a broadband (1-5MHz) PST-30SBP phased-array transducer was used for standard transthoracic echocardiographic examinations. Measurements of left ventricular (LV) dimensions, volumes and ejection fraction were obtained in accordance with the recommendations of the American Society of Echocardiography.8 The degree of mitral regurgitation (MR) was graded visually by color Doppler echocardiography.
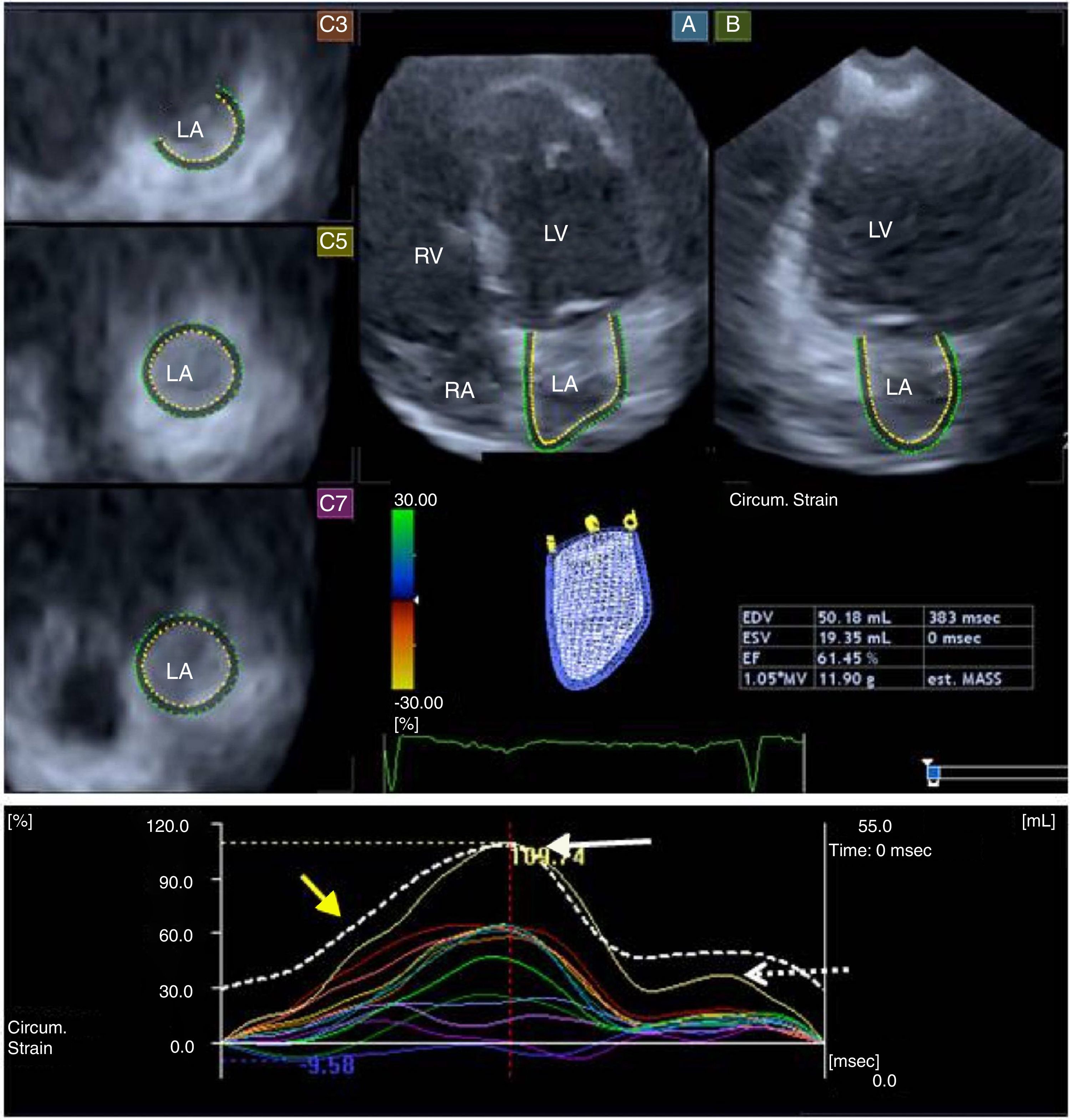
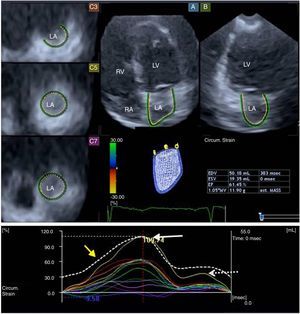
Three-dimensional speckle-tracking echocardiographyDuring the same echocardiographic examination, 3D datasets were acquired in apical view using a commercially available 1-4MHz PST-25SX matrix-array transducer (Toshiba Medical Systems, Tokyo, Japan).3 During end-expiratory breath-hold and six ECG-gated beats, six wedge-shaped subvolumes were acquired to create the LV full volume. Off-line analysis of the 3D datasets was performed using 3D Wall Motion Tracking software, version 2.5 (Toshiba Medical Systems, Tokyo, Japan). Apical 2-chamber (AP2CH), 4-chamber (AP4CH), and short-axis views at different levels of the left atrium (basal, mid, and superior) were automatically selected at end-diastole (Figure 1). Non-foreshortened AP2CH and AP4CH views were determined by finding the largest long-axis LA dimensions, then the mitral annulus and the LA apex were marked manually. The LA appendage and pulmonary veins were excluded from the examination. Following LA border detection at the end-diastolic reference frame, wall motion tracking was performed automatically in 3D space throughout the cardiac cycle. The shape of the LA was corrected if needed. Due to the absence of an LA-specific segmentation model, the left atrium was automatically divided into 16 segments using standard LV segmentation.9
Apical 4-chamber (A) and 2-chamber views (B), and different parasternal short-axis views at basal (C3), mid (C5) and superior (C7) left atrial regions, extracted from the three-dimensional volume. A three-dimensional wireframe reconstruction of the left atrium based on three-dimensional speckle-tracking echocardiographic analysis together with volumetric data and segmental (circumferential) time-strain curves are also presented. White, dashed and yellow arrows represent segmental (systolic) peak strain, (late-diastolic) strain at atrial contraction and global time-volume curve, respectively. LA: left atrium; LV: left ventricle; RA: right atrium; RV: right ventricle.
Using the ECG-gated 3D-LA model, end-systolic maximum volume (Vmax), diastolic volume before atrial contraction (VpreA) and end-diastolic minimum volume (Vmin) were measured in each case10–16 (Figure 1). From the three volumes, the following features of different phases of LA function were also calculated:
For (systolic) reservoir function:
Total atrial stroke volume (TASV): Vmax−Vmin
Total atrial emptying fraction (TAEF): TASV/Vmax×100
For (early diastolic) conduit function:
Passive atrial stroke volume (PASV): Vmax–VpreA
Passive atrial emptying fraction (PAEF): PASV/Vmax×100
For (late diastolic) active contraction:
Active atrial stroke volume (AASV): VpreA−Vmin
Active atrial emptying fraction (AAEF): AASV/ VpreA×100
The following parameters of LA deformation were assessed13–18: global, mean segmental and regional (basal, mid and superior) radial (RS), longitudinal (LS), circumferential (CS), area (AS) and 3D (3DS) strain. Using LA time-strain curves, the first peak (feature of systolic LA reservoir function) and the second peak (strain at atrial contraction, a characteristic of LA booster pump function) were calculated in each patient.
Statistical analysisContinuous variables were presented as mean ± standard deviation and tested for normality. Categorical data were expressed as percentages. A value of p<0.05 was considered statistically significant. Variables were compared using the independent samples Student's t test and the chi-square test as appropriate. Recently, data from the MAGYAR-Path Study confirmed excellent intraobserver and interobserver agreements for 3D-STE-derived LA volumetric and strain data.12,15 MedCalc software was used for statistical calculations (MedCalc, Mariakerke, Belgium).
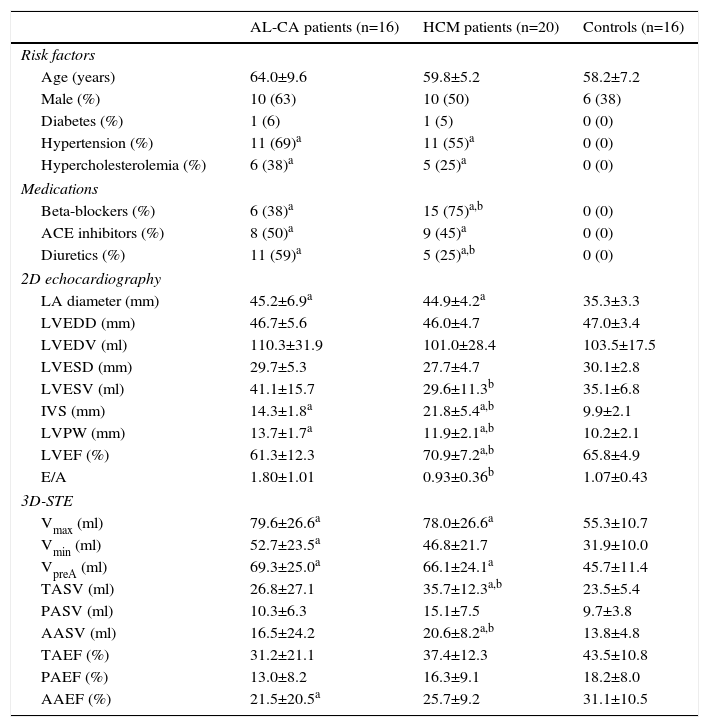
ResultsClinical characteristics of light-chain cardiac amyloidosis and hypertrophic cardiomyopathy patientsThe prevalence of cardiovascular risk factors and medications prescribed in patients with AL-CA and with HCM are presented in Table 1. Six of the 20 HCM patients had a significant (>30mmHg) resting peak LV outflow tract gradient (mean: 83.5±23.0mmHg), while eight HCM patients presented systolic anterior motion of the mitral valve anterior leaflet. One HCM patient had an implantable cardioverter-defibrillator for prophylaxis of malignant arrhythmia and two HCM patients had previous percutaneous transluminal septal myocardial ablation. Genetic study had been completed in two of the 20 HCM patients (10%), one of whom carried a TCAP gene mutation while the other had no sarcomeric gene mutation. Genetic study of the other patients is currently underway. Magnetic resonance imaging confirmed the diagnosis of HCM in five cases.
Clinical and two-dimensional echocardiographic characteristics of patients with light-chain cardiac amyloidosis and with hypertrophic cardiomyopathy and of controls.
| AL-CA patients (n=16) | HCM patients (n=20) | Controls (n=16) | |
|---|---|---|---|
| Risk factors | |||
| Age (years) | 64.0±9.6 | 59.8±5.2 | 58.2±7.2 |
| Male (%) | 10 (63) | 10 (50) | 6 (38) |
| Diabetes (%) | 1 (6) | 1 (5) | 0 (0) |
| Hypertension (%) | 11 (69)a | 11 (55)a | 0 (0) |
| Hypercholesterolemia (%) | 6 (38)a | 5 (25)a | 0 (0) |
| Medications | |||
| Beta-blockers (%) | 6 (38)a | 15 (75)a,b | 0 (0) |
| ACE inhibitors (%) | 8 (50)a | 9 (45)a | 0 (0) |
| Diuretics (%) | 11 (59)a | 5 (25)a,b | 0 (0) |
| 2D echocardiography | |||
| LA diameter (mm) | 45.2±6.9a | 44.9±4.2a | 35.3±3.3 |
| LVEDD (mm) | 46.7±5.6 | 46.0±4.7 | 47.0±3.4 |
| LVEDV (ml) | 110.3±31.9 | 101.0±28.4 | 103.5±17.5 |
| LVESD (mm) | 29.7±5.3 | 27.7±4.7 | 30.1±2.8 |
| LVESV (ml) | 41.1±15.7 | 29.6±11.3b | 35.1±6.8 |
| IVS (mm) | 14.3±1.8a | 21.8±5.4a,b | 9.9±2.1 |
| LVPW (mm) | 13.7±1.7a | 11.9±2.1a,b | 10.2±2.1 |
| LVEF (%) | 61.3±12.3 | 70.9±7.2a,b | 65.8±4.9 |
| E/A | 1.80±1.01 | 0.93±0.36b | 1.07±0.43 |
| 3D-STE | |||
| Vmax (ml) | 79.6±26.6a | 78.0±26.6a | 55.3±10.7 |
| Vmin (ml) | 52.7±23.5a | 46.8±21.7 | 31.9±10.0 |
| VpreA (ml) | 69.3±25.0a | 66.1±24.1a | 45.7±11.4 |
| TASV (ml) | 26.8±27.1 | 35.7±12.3a,b | 23.5±5.4 |
| PASV (ml) | 10.3±6.3 | 15.1±7.5 | 9.7±3.8 |
| AASV (ml) | 16.5±24.2 | 20.6±8.2a,b | 13.8±4.8 |
| TAEF (%) | 31.2±21.1 | 37.4±12.3 | 43.5±10.8 |
| PAEF (%) | 13.0±8.2 | 16.3±9.1 | 18.2±8.0 |
| AAEF (%) | 21.5±20.5a | 25.7±9.2 | 31.1±10.5 |
2D: two-dimensional; 3D-STE: three-dimensional speckle-tracking echocardiography; AAEF: active atrial emptying fraction; AASV: active stroke volume; ACE: angiotensin-converting enzyme; AL-CA: light-chain cardiac amyloidosis; HCM: hypertrophic cardiomyopathy; IVS: interventricular septum; LA: left atrial; LV: left ventricular; LVEDD: left ventricular end-diastolic diameter; LVEDV: left ventricular end-diastolic volume; LVEF: left ventricular ejection fraction; LVESD: left ventricular end-systolic diameter; LVESV: left ventricular end-systolic volume; LVPW: left ventricular posterior wall; PAEF: passive atrial emptying fraction; PASV: passive atrial stroke volume; TAEF: total atrial ejection fraction; TASV: total atrial stroke volume; Vmax: maximum left atrial volume; Vmin: minimum left atrial volume; VpreA: left atrial volume before atrial contraction.
Standard 2D echocardiographic data are summarized in Table 1. Significant (grade ≥2) MR was detected in seven HCM patients (35%) and in two AL-CA patients (13%).
Three-dimensional speckle-tracking echocardiography-derived left atrial volumetric and volume-based functional parametersIncreased LA volumes were demonstrated in AL-CA and HCM patients compared to controls. None of the LA stroke volumes showed alterations in AL-CA patients, while TASV and AASV were found to be increased in HCM patients compared to controls and AL-CA patients. Only AAEF was found to be significantly reduced in AL-CA patients compared to controls. However, emptying fractions of HCM patients were between the values of AL-CA patients and those of controls.
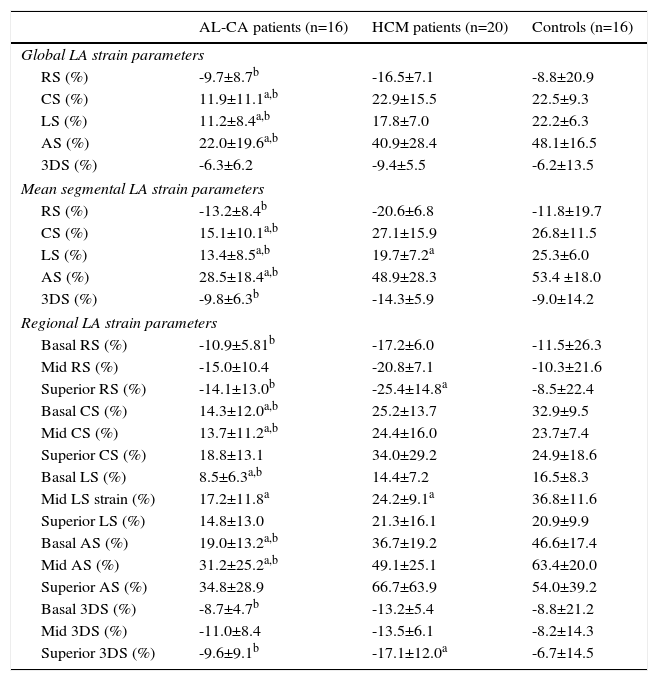
Three-dimensional speckle-tracking echocardiography-derived peak global, mean segmental and regional left atrial strainPeak global and mean segmental CS, LS and AS showed significant reductions in AL-CA patients compared to controls (Table 2). Differences were observed in certain global and mean segmental peak strains of AL-CA and HCM patients. Only peak mean segmental LS was significantly decreased in HCM patients compared to controls. Regional peak strains of age-matched AL-CA and HCM patients and controls are presented in Table 2.
Comparison of three-dimensional speckle-tracking echocardiography-derived global, mean segmental and regional peak left atrial strain parameters in patients with cardiac amyloidosis and with hypertrophic cardiomyopathy and in controls.
| AL-CA patients (n=16) | HCM patients (n=20) | Controls (n=16) | |
|---|---|---|---|
| Global LA strain parameters | |||
| RS (%) | -9.7±8.7b | -16.5±7.1 | -8.8±20.9 |
| CS (%) | 11.9±11.1a,b | 22.9±15.5 | 22.5±9.3 |
| LS (%) | 11.2±8.4a,b | 17.8±7.0 | 22.2±6.3 |
| AS (%) | 22.0±19.6a,b | 40.9±28.4 | 48.1±16.5 |
| 3DS (%) | -6.3±6.2 | -9.4±5.5 | -6.2±13.5 |
| Mean segmental LA strain parameters | |||
| RS (%) | -13.2±8.4b | -20.6±6.8 | -11.8±19.7 |
| CS (%) | 15.1±10.1a,b | 27.1±15.9 | 26.8±11.5 |
| LS (%) | 13.4±8.5a,b | 19.7±7.2a | 25.3±6.0 |
| AS (%) | 28.5±18.4a,b | 48.9±28.3 | 53.4 ±18.0 |
| 3DS (%) | -9.8±6.3b | -14.3±5.9 | -9.0±14.2 |
| Regional LA strain parameters | |||
| Basal RS (%) | -10.9±5.81b | -17.2±6.0 | -11.5±26.3 |
| Mid RS (%) | -15.0±10.4 | -20.8±7.1 | -10.3±21.6 |
| Superior RS (%) | -14.1±13.0b | -25.4±14.8a | -8.5±22.4 |
| Basal CS (%) | 14.3±12.0a,b | 25.2±13.7 | 32.9±9.5 |
| Mid CS (%) | 13.7±11.2a,b | 24.4±16.0 | 23.7±7.4 |
| Superior CS (%) | 18.8±13.1 | 34.0±29.2 | 24.9±18.6 |
| Basal LS (%) | 8.5±6.3a,b | 14.4±7.2 | 16.5±8.3 |
| Mid LS strain (%) | 17.2±11.8a | 24.2±9.1a | 36.8±11.6 |
| Superior LS (%) | 14.8±13.0 | 21.3±16.1 | 20.9±9.9 |
| Basal AS (%) | 19.0±13.2a,b | 36.7±19.2 | 46.6±17.4 |
| Mid AS (%) | 31.2±25.2a,b | 49.1±25.1 | 63.4±20.0 |
| Superior AS (%) | 34.8±28.9 | 66.7±63.9 | 54.0±39.2 |
| Basal 3DS (%) | -8.7±4.7b | -13.2±5.4 | -8.8±21.2 |
| Mid 3DS (%) | -11.0±8.4 | -13.5±6.1 | -8.2±14.3 |
| Superior 3DS (%) | -9.6±9.1b | -17.1±12.0a | -6.7±14.5 |
3DS: three-dimensional strain; AL-CA: light-chain cardiac amyloidosis; AS: area strain; CS: circumferential strain; HCM: hypertrophic cardiomyopathy; LA: left atrial; LS: longitudinal strain; RS: radial strain.
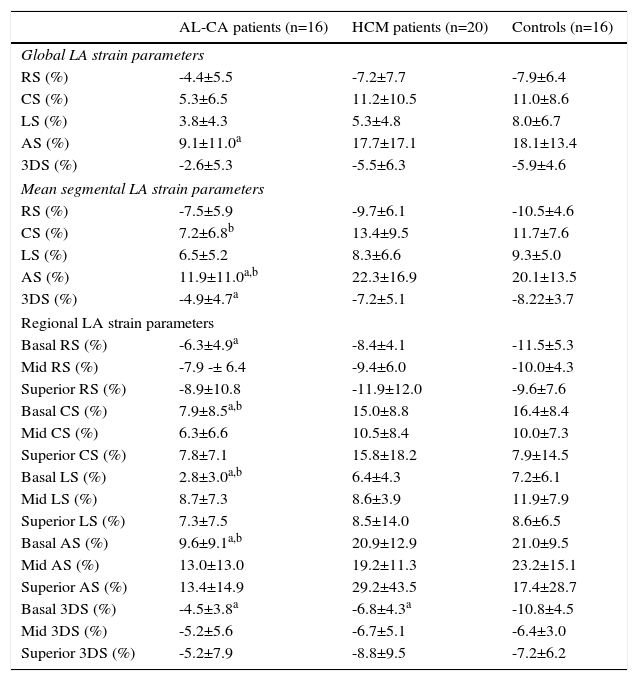
While no differences were demonstrated in global and mean segmental strain at atrial contraction between HCM patients and controls, AL-CA patients showed reductions in certain strain parameters compared to controls and HCM patients. Results of detailed regional analysis are presented in Table 3.
Comparison of three-dimensional speckle-tracking echocardiography-derived global, mean segmental and regional left atrial strain parameters at atrial contraction in patients with cardiac amyloidosis and with hypertrophic cardiomyopathy and in controls.
| AL-CA patients (n=16) | HCM patients (n=20) | Controls (n=16) | |
|---|---|---|---|
| Global LA strain parameters | |||
| RS (%) | -4.4±5.5 | -7.2±7.7 | -7.9±6.4 |
| CS (%) | 5.3±6.5 | 11.2±10.5 | 11.0±8.6 |
| LS (%) | 3.8±4.3 | 5.3±4.8 | 8.0±6.7 |
| AS (%) | 9.1±11.0a | 17.7±17.1 | 18.1±13.4 |
| 3DS (%) | -2.6±5.3 | -5.5±6.3 | -5.9±4.6 |
| Mean segmental LA strain parameters | |||
| RS (%) | -7.5±5.9 | -9.7±6.1 | -10.5±4.6 |
| CS (%) | 7.2±6.8b | 13.4±9.5 | 11.7±7.6 |
| LS (%) | 6.5±5.2 | 8.3±6.6 | 9.3±5.0 |
| AS (%) | 11.9±11.0a,b | 22.3±16.9 | 20.1±13.5 |
| 3DS (%) | -4.9±4.7a | -7.2±5.1 | -8.22±3.7 |
| Regional LA strain parameters | |||
| Basal RS (%) | -6.3±4.9a | -8.4±4.1 | -11.5±5.3 |
| Mid RS (%) | -7.9 -± 6.4 | -9.4±6.0 | -10.0±4.3 |
| Superior RS (%) | -8.9±10.8 | -11.9±12.0 | -9.6±7.6 |
| Basal CS (%) | 7.9±8.5a,b | 15.0±8.8 | 16.4±8.4 |
| Mid CS (%) | 6.3±6.6 | 10.5±8.4 | 10.0±7.3 |
| Superior CS (%) | 7.8±7.1 | 15.8±18.2 | 7.9±14.5 |
| Basal LS (%) | 2.8±3.0a,b | 6.4±4.3 | 7.2±6.1 |
| Mid LS (%) | 8.7±7.3 | 8.6±3.9 | 11.9±7.9 |
| Superior LS (%) | 7.3±7.5 | 8.5±14.0 | 8.6±6.5 |
| Basal AS (%) | 9.6±9.1a,b | 20.9±12.9 | 21.0±9.5 |
| Mid AS (%) | 13.0±13.0 | 19.2±11.3 | 23.2±15.1 |
| Superior AS (%) | 13.4±14.9 | 29.2±43.5 | 17.4±28.7 |
| Basal 3DS (%) | -4.5±3.8a | -6.8±4.3a | -10.8±4.5 |
| Mid 3DS (%) | -5.2±5.6 | -6.7±5.1 | -6.4±3.0 |
| Superior 3DS (%) | -5.2±7.9 | -8.8±9.5 | -7.2±6.2 |
3DS: three-dimensional strain; AL-CA: light-chain cardiac amyloidosis; AS: area strain; CS: circumferential strain; HCM: hypertrophic cardiomyopathy; LA: left atrial; LS: longitudinal strain; RS: radial strain.
To the best of the authors’ knowledge, this is the first time 3D-STE-derived LA functional properties have been compared by volumetric and strain analysis between AL-CA and HCM. Several features of the three different phases of LA function were assessed by 3D-STE during the same examination: systolic reservoir phase (by TASV, TAEF and peak strains); early-diastolic conduit phase (by PASV and PAEF); and late-diastolic booster pump function (by AASV, AAEF and strains at atrial contraction). The present analysis showed different patterns of LA dysfunction: impairment of the systolic LA reservoir phase occurs in both diseases, because reduced peak strain was found both in CA and HCM, but impairment in LA active contraction phases occurred only in CA (reductions in AAEF and strain at atrial contraction).
Several imaging methodologies have been demonstrated to be useful for non-invasive assessment of LA dimensions, volumes and function. 3D-STE is based on a block-matching algorithm of myocardial speckles on the endocardial border during their frame-to-frame motion.3,19,20 It is a relatively new echocardiographic technique that aims to incorporate all the benefits of STE and 3D echocardiography, including LA volumetric10–16 and strain13–18 assessments.
LA functional remodeling in AL-CA appears to be more extensive than in HCM. This could be explained by the fact that while HCM represents a myopathic process affecting ventricular and atrial myocardium, CA results in much more diffuse and ubiquitous involvement,1,2 due to mainly interstitial, nodular and branching deposition of amyloid, which can have a major impact on LV diastolic function that directly impairs LA structure and function. Moreover, hemodynamic reasons could not be excluded; higher MR grades were detected in 13-35% of AL-CA and HCM patients, which could also have an effect on atrial remodeling.
Increased LA volumes and impaired LA myocardial deformation are well-known features in HCM.13,21 Moreover, increased LA volume is a predictor of adverse outcome and impaired LA function is presumed to be due to LV diastolic dysfunction as a result of hypertrophy and myocardial fibrosis.22 LA volumes and strains were found to be more affected in patients with obstruction.22 In a recent 3D-STE study of volumetric and strain functional properties, only TAEF differed significantly between HCM patients with vs. without grade ≥2 MR, but no differences were found between the same parameters in HCM patients with vs. without classic risk factors.13 On the other hand, LA enlargement was found to be an independent predictor of long-term mortality, aiding risk stratification and management of patients presenting with amyloidosis.23 LA dysfunction was also observed in AL amyloidosis patients without other echocardiographic features of cardiac involvement using conventional and strain echocardiography for measuring LA ejection force, LA strain and strain rate.24 All these results suggest increased LA volumes and reduced LA functional properties in both HCM and CA. In the present study, detailed analysis of LA dysfunction was performed by 3D-STE in CA and HCM patients. Different patterns of LA dysfunction demonstrate that 3D-STE theoretically has potential for differentiating these patient populations. However, further studies in larger patient populations are warranted to confirm our findings.
LimitationsDespite recent improvements in 3D echocardiographic analysis, one of the main limitations of 3D-STE is its relatively low temporal and spatial resolution compared to 2D techniques.
Although 3D-STE has been validated for the assessment of LA volumes and functional properties including strain assessments against different reference techniques,10–12,15 further studies are warranted to confirm its accuracy. Since no 2D-STE or other imaging technique was used together with 3D-STE and no clinical or prognostic correlations were performed between these methodologies, the accuracy of 3D-STE could not be established in this study.
The diversity of HCM patients, including genetic background, development of dynamic obstructions and arrhythmias, may also have had an effect on the results.
It is important to emphasize the effects of age on LA parameters. In a recent study using the same methodology, LA functional properties of HCM patients were compared with those of controls, and more significant differences were found in volume-based functional parameters; the mean age of the participants was significantly lower in this previous study. In the present study, the mean age of the control group was greater than in the previous study, and differences in TAEF and PAEF disappeared due to impaired LA functional parameters of this older control group.13 These findings highlight the importance of age in influencing the results.
Only visual grading of MR was used, which could lead to misgrading; other parameters were not calculated in this study.
Moreover, dependence on the place of measurement, even in healthy subjects, should be taken into account when interpreting results.25
ConclusionsDifferent patterns of LA functional characteristics were demonstrated between AL-CA and HCM patients by 3D-STE. This may be explained by the different nature of the diseases: while HCM represents a myopathic process, AL-CA results in much more diffuse and ubiquitous involvement of the myocardial tissue with amyloid deposition.
Ethical standardsThe authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committee of the University of Szeged.
Author contributionsAttila Nemes – study design, writing paper
Dóra Földeák – study design, writing paper
Árpád Kormányos – patient management, performing 3D-STE examinations
Péter Domsik – patient management, performing 3D-STE examinations
Anita Kalapos – patient management, performing 3D-STE examinations
Nóra Ambrus – supervision
Zénó Ajtay – supervision
Róbert Sepp – supervision, writing paper
Zita Borbényi – supervision, writing paper
Tamás Forster – supervision, writing paper
FundingThis research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to thank Roland Nagy-László, MS, for his assistance in managing data, and Andrea Orosz, MD, PhD, for linguistic corrections.