Oral anticoagulants have proved to be highly effective in preventing atrial fibrillation (AF)-related strokes. The occurrence of stroke despite oral anticoagulation is unexpected and little is known about the mechanisms responsible. The aim of this study was to assess possible mechanisms for stroke occurrence, such as poor treatment adherence and inappropriate dosage, in patients chronically anticoagulated for AF.
MethodsWe performed a prospective observational study of 60 consecutive patients with non-valvular AF, chronically medicated with an oral anticoagulant and admitted due to ischemic stroke. Treatment adherence was assessed through the Brief Medication Questionnaire (BMQ) and the Medição da Adesão ao Tratamento (MAT) scales. Patient characteristics, stroke etiology, and appropriacy of anticoagulant dosage were also assessed.
ResultsPatients’ mean age was 78.6±8.0 years, and 51.7% were male. Overall, the proportion of patients with good adherence to anticoagulants was 63.3%. Adherent patients were more frequently illiterate (26.3% vs. 4.5%, p=0.012). The proportion of patients under vitamin K antagonists (VKAs) with good treatment adherence was significantly higher than that of patients under novel oral anticoagulants (NOACs) (83.3% vs. 54.8%, respectively, for BMQ, p=0.035). However, 91.7% of patients under VKAs presented an admission INR <2. Subtherapeutic prescriptions were found in 43% of patients under NOACs.
ConclusionIn the majority of patients, stroke occurrence despite chronic anticoagulation appears to be explained by subtherapeutic dosage, poor treatment adherence or non-cardioembolic etiology, and not by inefficacy of the anticoagulants.
Os anticoagulantes orais demonstraram ser altamente eficazes na prevenção do acidente vascular cerebral (AVC) associado a fibrilhação auricular (FA). A ocorrência de AVC apesar da hipocoagulação oral não é expectável, existindo escassa informação sobre os mecanismos responsáveis pela sua ocorrência. O objetivo deste estudo foi avaliar possíveis mecanismos para a ocorrência de AVC isquémico, como a má adesão à terapêutica e a não adequação da dosagem dos anticoagulantes em doentes cronicamente hipocoagulados por FA.
MétodosEstudo prospetivo observacional, de 60 doentes consecutivos com FA não valvular, cronicamente medicados com anticoagulante oral, internados por AVC isquémico. Avaliação da adesão terapêutica através das escalas Brief Medication Questionnaire (BMQ) e Medição da Adesão ao Tratamento (MAT). Avaliação das características dos doentes, etiologia do AVC e adequação da dosagem do anticoagulante.
ResultadosA idade média era de 78,6 ± 8,0 anos, com 51,7% dos doentes do sexo masculino. Globalmente, a proporção de doentes com boa adesão terapêutica aos anticoagulantes foi de 63,3%. Os doentes aderentes eram mais frequentemente analfabetos (26,3% vs. 4,5, p = 0,012). A proporção de doentes sob antivitamínicos K (AVK) com boa adesão terapêutica era significativamente superior à dos doentes sob anticoagulantes orais não antivitamínicos K (NOAC) (respetivamente, 83,3% versus 54,8%, p = 0,035 para BMQ). No entanto, 91,7% dos doentes sob AVK apresentavam INR < 2 na admissão. Identificaram-se prescrições subterapêuticas em 43% dos doentes sob NOAC.
ConclusõesNa maioria dos doentes, a ocorrência de AVC apesar da hipocoagulação parece ser explicada por subdosagem, má adesão terapêutica ou etiologia não cardioembólica e não por ineficácia dos anticoagulantes.
It is estimated that around 33 million individuals worldwide have been diagnosed with atrial fibrillation (AF). The diagnosis is frequently made only after the occurrence of complications such as stroke or systemic thromboembolism.1 The CHA2DS2-VASc score is recommended for assessment of the risk of cerebral ischemic events of cardioembolic origin associated with AF, and anticoagulation therapy is indicated for men with a score of 1 or more and for women with a score of 2 or more. Compared to vitamin K antagonists (VKAs), the novel oral anticoagulants (NOACs) have the advantages of a better efficacy/safety ratio, no need to monitor the patient's international normalized ratio (INR), and rapid onset of action. However, the direct costs of NOACs are higher, and their half-life is shorter. It should be noted that although it is more convenient for the patient not to have to undergo INR monitoring, this makes it more difficult to ascertain whether the treatment is being adhered to, while the short half-life of NOACs means that there is a greater risk of thrombotic events if patients fail to adhere to their prescribed dosage.2–4
The few studies carried out to date on adherence to NOAC therapy give conflicting results, with figures ranging from 57% to 96%, and no predictors of poor adherence have been identified.2,3,5–14
Although long-term oral anticoagulation significantly reduces the risk of AF-associated ischemic stroke, every year 1-2% of AF patients under NOAC therapy and 1.6% of those taking VKAs still suffer embolic stroke despite their therapy.15,16
In view of these findings, it is important to determine what mechanisms may be responsible for the occurrence of ischemic stroke in patients with non-valvular AF despite being under oral anticoagulation. Potential causes could include poor treatment adherence and subtherapeutic doses of NOACs. It would also be valuable to identify the factors associated with poor adherence, which could enable selection of the best anticoagulant in accordance with the profile of the individual patient.
The aim of this study was to assess possible mechanisms for stroke occurrence, such as poor treatment adherence and inappropriate dosage, in patients chronically anticoagulated for AF.
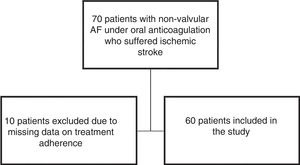
MethodsStudy design and patient selectionThis prospective observational study analyzed 60 consecutive patients admitted to the neurology department of Coimbra Hospital and University Center between November 2016 and August 2017 for ischemic stroke associated with non-valvular AF, despite chronic anticoagulation with warfarin, dabigatran, apixaban, rivaroxaban or edoxaban.
Ischemic stroke was diagnosed on the basis of evidence of acute focal neurological deficit lasting longer than 24 hours and cerebral ischemia identified by neuroimaging methods (computed tomography or brain magnetic resonance imaging).17 Stroke was classified in etiological subtypes according to the Trial of Org 10172 in Acute Stroke Treatment (TOAST) criteria as (1) large-artery atherosclerosis, (2) cardioembolism, (3) small-vessel occlusion (lacune), (4) stroke of other determined etiology, or (5) stroke of undetermined etiology.17 Severity of neurological damage at admission was assessed by a neurologist using the National Institutes of Health Stroke Scale. The patient selection process is illustrated in Figure 1.
The study was approved by the ethics committee of the Central Region health authority and was conducted in accordance with the international guidelines for clinical research of the Declaration of Helsinki of the World Medical Association. All patients provided written informed consent.
Study protocolThe following information was collected for each patient: demographic data, socioeconomic status as measured by the Graffar scale, educational level, personal history (hypertension; dyslipidemia; diabetes; sedentary lifestyle; heart failure; thromboembolism, stroke or transient ischemic attack; previous coronary disease or myocardial infarction), CHA2DS2-VASc score, smoking status, alcohol consumption, renal function assessed by the Cockcroft-Gault formula, and medication, including type and dosage of oral anticoagulation, INR if applicable, and other drug therapies. Adequacy of dosage of NOACs was assessed on the basis of the recommended doses for each drug and the renal function, age, weight, and concomitant medication of the individual patient, with dosages being classified as adequate, subtherapeutic, or supratherapeutic. On the basis of the patient's overall medication, their Medication Regimen Complexity Index was calculated. This validated tool assesses the complexity of drug therapy independently of socioeconomic, pharmacological and clinical factors, based on types of prescribed dosage forms, dosing frequency, and additional directions given by the prescriber and that patients need to take into consideration to ensure that the drug is administered correctly.18
Adherence to anticoagulant therapy in each patient was assessed by the application of two instruments, both validated for the Portuguese language: the Brief Medication Questionnaire (BMQ)19 and Medição da Adesão ao Tratamento (Measure of Treatment Adherence, MAT).20
The BMQ consists of three sets of questions that assess treatment adherence by asking patients how they take their medication, their beliefs, and how they remember, classifying adherence as high (no positive responses), probably high (one positive response), probably low (two positive responses), or low (three or more positive responses). For the purposes of this study, two or more positive responses were considered to indicate non-adherence.
The MAT includes seven items assessing patients’ behavior concerning daily drug use, the response to each item being scored on a six-point Likert scale from 1 (always) to 6 (never). The level of adherence is obtained by adding together the scores for each item and dividing by the number of items, giving a total score between 1 and 6, with higher numbers indicating better adherence.
Statistical analysisCategorical variables (demographics, clinical characteristics and type of anticoagulant) were expressed as frequency and percentage, and continuous variables were presented as means and standard deviation.
Patients under VKAs were compared to those under NOACs. The MAT score and the BMQ results (dividing the study population into adherers and non-adherers according to the above criteria) were used to identify potential predictors of poor treatment adherence. Dichotomous (categorical) variables were compared with the chi-square test or Fisher's exact test, and continuous variables were compared using the Student's t test or the Mann-Whitney test, depending on normality of distribution.
Spearman's correlation was used to compared the accuracy of the two adherence scores.
A p-value <0.05 was considered statistically significant in all tests. The statistical analysis was performed in IBM SPSS® version 23.
ResultsOverall characteristics of the study populationPatients’ mean age was 78.6±8.0 years, and 51.7% were male. Regarding socioeconomic status, 56.6% were middle or upper-middle class and none were upper class. The illiteracy rate was 18.3% and most subjects had only completed primary education; none had an educational level higher than a bachelor's degree. Mean CHA2DS2-VASc score was 4.3±1.4, minimum 1 and maximum 7. Subtherapeutic doses were identified in 43% of patients taking NOACs: 44% of those taking dabigatran, 22% apixaban and 34% rivaroxaban. The overall characteristics of the study population are presented in Table 1.
Overall characteristics of the study population.
| Patients, n | 60 | Previous MI, % | 11.7 |
| Age (years), mean±SD | 78.6±8.0 | Coronary disease, % | 15 |
| Male, % | 51.7 | Heart failure, % | 28.3 |
| Cardioembolic stroke, % | 86.4 | Excessive alcohol consumption, % | 25 |
| Socioeconomic class, % | Smoking, % | 20 | |
| Low | 16.7 | Pack-years, mean±SD | 40.3±34.0 |
| Lower-middle | 26.7 | ||
| Middle | 38.3 | ||
| Upper-middle | 18.3 | CrCl (ml/min), mean±SD | 65.5±23.2 |
| Educational level, % | |||
| Illiterate | 18.3 | OAC, % | |
| Primary | 58.3 | VKAs | 30 |
| Secondary | 11.7 | NOACs | 70 |
| Bachelor's degree | 11.7 | Subtherapeutic NOAC dose, % | 43 |
| CHA2DS2-VASc score, mean±SD | 4.3±1.4 | ||
| NIHSS, mean±SD | 10.1±8.2 | ||
| Sedentary lifestyle, % | 46.7 | MRCI, mean±SD | 20.6±9.7 |
| Dyslipidemia, % | 71.7 | ||
| Diabetes, % | 28.3 | BMQ (adherent/non-adherent), % | 63.3/36.7 |
| Hypertension, % | 81.7 | ||
| Previous stroke/TIA, % | 28.3 | MAT, mean±SD | 5.64±0.62 |
BMQ: Brief Medication Questionnaire; CrCl: creatinine clearance; MAT: Medição da Adesão ao Tratamento score; MI: myocardial infarction; MRCI: Medication Regimen Complexity Index; NIHSS: National Institutes of Health Stroke Scale; NOACs: novel oral anticoagulants; OAC: oral anticoagulation; SD: standard deviation; TIA: transient ischemic attack; VKAs: vitamin K antagonists.
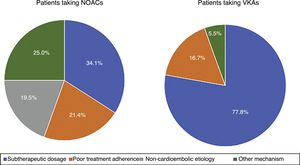
Eighteen patients (30%) were anticoagulated with VKAs and 42 (70%) with NOACs, of whom 15.0% were taking apixaban, 23.3% dabigatran, 1.7% edoxaban and 30.0% rivaroxaban. In those taking VKAs, all cases of stroke were of cardioembolic etiology. Also in this group, mean INR at admission for stroke was 1.5±0.4, and 91.7% of them presented INR <2. Among patients taking NOACs, 19.5% of cases of stroke were non-cardioembolic in origin (all due to small-vessel disease). In the subgroup of patients taking NOACs who suffered cardioembolic stroke, a large proportion (33.3% of those on NOACs, 14 patients) were taking subtherapeutic doses (five on dabigatran 110 mg instead of 150 mg twice daily, three on apixaban 2.5 mg instead of 5 mg twice daily, and six on rivaroxaban 15 mg instead of 20 mg daily). Among patients with cardioembolic stroke and appropriate NOAC dosage, treatment adherence was poor in 47% (nine patients, 21.4% of those on NOACs) (Figure 2).
No drugs that potentially could interact with oral anticoagulation were recorded. Comparison between patients taking VKAs and those taking NOACs showed differences in the proportions of adherent patients and in those with a history of MI or heart failure, with more in the VKA group (Table 2).
Comparison of patient characteristics according to oral anticoagulant class.
| VKAs | NOACs | p | |
|---|---|---|---|
| Patients, n (%) | 18 (30) | 42 (70) | |
| Stroke etiology (%) | 0.092 | ||
| Cardioembolic | 100 | 80.5 | |
| Non-cardioembolic | 0 | 19.5 | |
| Age (years), mean±SD | 79.2±10.4 | 78.4±6.9 | 0.740 |
| Male/female, % | 55.6/44.4 | 50.0/50.0 | 0.693 |
| Socioeconomic class, % | 0.396 | ||
| Low | 16.7 | 16.7 | |
| Lower-middle | 33.3 | 23.8 | |
| Middle | 44.4 | 35.7 | |
| Upper-middle | 5.6 | 23.8 | |
| Educational level, % | 0.447 | ||
| Illiterate | 27.8 | 14.3 | |
| Primary | 44.4 | 64.3 | |
| Secondary | 16.7 | 9.5 | |
| Bachelor's degree | 11.1 | 11.9 | |
| CHA2DS2-VASc score, mean±SD | 4.4±1.0 | 4.2±1.5 | 0.497 |
| NIHSS, mean±SD | 9.6±6.9 | 10.3±8.7 | 0.742 |
| Sedentary lifestyle, % | 38.9 | 50.0 | 0.429 |
| Dyslipidemia, % | 77.8 | 69.0 | 0.492 |
| Diabetes, % | 27.8 | 28.6 | 0.950 |
| Hypertension, % | 88.9 | 78.6 | 0.478 |
| Previous stroke/TIA, % | 22.2 | 31.0 | 0.492 |
| Previous MI, % | 27.8 | 4.8 | 0.011 |
| Heart failure, % | 44.4 | 21.4 | 0.070 |
| Smoking, % | 22.2 | 19.0 | 0.778 |
| Pack-years, mean±SD | 36.1±42.9 | 42.6±31.4 | 0.777 |
| Excessive alcohol consumption, % | 27.8 | 23.8 | 0.745 |
| CrCl (ml/min), mean±SD | 57.4±23.1 | 68.6±22.8 | 0.114 |
| MRCI, mean±SD | 23.7±10.4 | 19.4±9.2 | 0.135 |
| BMQ (adherent/non-adherent), % | 83.3/16.7 | 54.8/45.2 | 0.035 |
| MAT, mean±SD | 5.87±0.3 | 5.54±0.7 | 0.044 |
BMQ: Brief Medication Questionnaire; CrCl: creatinine clearance; MAT: Medição da Adesão ao Tratamento score; MI: myocardial infarction; MRCI: Medication Regimen Complexity Index; NIHSS: National Institutes of Health Stroke Scale; NOACs: novel oral anticoagulants; SD: standard deviation; TIA: transient ischemic attack; VKAs: vitamin K antagonists.
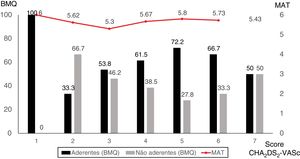
There was excellent correlation between the two scores used to assess treatment adherence (r=-0.955, p<0.001). According to the BMQ, 63.3% of the overall population presented good treatment adherence, while the mean MAT score was 5.6±0.6, minimum 2.4 and maximum 6.0 (Table 1). Of adherent patients, 26.3% were illiterate, in contrast to only 4.5% of non-adherent patients (p=0.012). The CHA2DS2-VASc score was similar in both adherent and non-adherent patients as determined by the BMQ (Figure 3). The characteristics of the study population according to treatment adherence are shown in Table 3.
Characteristics of the study population according to treatment adherence as assessed by the BMQ.
| Adherent | Non-adherent | p | |
|---|---|---|---|
| Patients, n | 38 (63.3) | 22 (36.7) | |
| Age (years), mean±SD | 79.1±8.9 | 77.8±6.3 | 0.553 |
| Male/female, % | 55.3/44.7 | 45.5/55.3 | 0.317 |
| Socioeconomic class, % | 0.123 | ||
| Low | 23.7 | 4.5 | |
| Lower-middle | 26.3 | 27.3 | |
| Middle | 28.9 | 54.5 | |
| Upper-middle | 21.1 | 13.7 | |
| Educational level, % | 0.012 | ||
| Illiterate | 26.3 | 4.5 | |
| Primary | 44.7 | 81.8 | |
| Secondary | 18.5 | 0 | |
| Bachelor's degree | 10.5 | 13.6 | |
| CHA2DS2-VASc score, mean±SD | 4.34±1.38 | 4.18±1.37 | 0.665 |
| NIHSS, mean±SD | 11.1±8.6 | 8.2±7.1 | 0.195 |
| Sedentary lifestyle, % | 52.6 | 36.4 | 0.224 |
| Dyslipidemia, % | 71.1 | 72.7 | 0.890 |
| Diabetes, % | 23.7 | 36.4 | 0.294 |
| Hypertension, % | 81.6 | 81.8 | 1.00 |
| Previous stroke/TIA, % | 34.2 | 18.2 | 0.184 |
| Previous MI, % | 13.2 | 9.1 | 1.00 |
| Heart failure, % | 26.3 | 31.8 | 0.649 |
| Smoking, % | 23.7 | 13.6 | 0.507 |
| Pack-years, mean±SD | 38±32 | 47±46 | 0.710 |
| Excessive alcohol consumption, % | 23.7 | 27.3 | 0.757 |
| CrCl (ml/min), mean±SD | 64.2±21.9 | 68.1±26.2 | 0.57 |
| OAC, % | 0.035 | ||
| VKAs | 39.5 | 13.6 | |
| NOACs | 60.5 | 86.4 | |
| Subtherapeutic NOAC dose, % | 47.8 | 36.8 | 0.815 |
| MRCI, mean±SD | 21.6±10.0 | 18.8±9.0 | 0.297 |
| MAT, mean±SD | 5.99±0.03 | 5.03±67 | |
BMQ: Brief Medication Questionnaire; CrCl: creatinine clearance; MAT: Medição da Adesão ao Tratamento score; MI: myocardial infarction; MRCI: Medication Regimen Complexity Index; NIHSS: National Institutes of Health Stroke Scale; NOACs: novel oral anticoagulants; OAC: oral anticoagulation; SD: standard deviation; TIA: transient ischemic attack; VKAs: vitamin K antagonists.
Of the 30% of patients taking VKAs, 83.3% were adherent to anticoagulant therapy according to the BMQ (mean MAT score 5.9±0.3), while of the 70% taking NOACs, only 54.8% were adherent (mean MAT score 5.5±0.7) (p=0.035 and p=0.044 for BMQ and MAT, respectively) (Table 2).
Potential mechanisms for stroke despite oral anticoagulationAlthough the proportion of patients taking VKAs with poor treatment adherence was relatively low (30%), most (91.7%) presented subtherapeutic INR at admission.
Among patients taking NOACs, a non-cardioembolic stroke etiology was identified in 19.5% of cases, which may explain why oral anticoagulation was ineffective in preventing these strokes. Furthermore, another 33.3% of patients on NOACs were receiving subtherapeutic doses, and of those with appropriate dosages, almost half (amounting to 21.4% of patients on NOACs) presented poor adherence to the drugs they were prescribed (Figure 2). Thus, among patients who suffered stroke despite chronic therapy with NOACs, a non-cardioembolic etiology and/or subtherapeutic dosages and/or poor treatment adherence were observed in 74.2% of cases.
DiscussionThe main findings of this study are that in patients suffering stroke despite taking oral anticoagulants, poor treatment adherence is more common in those taking NOACs than in those taking VKAs (even though most patients on VKAs had subtherapeutic INR on admission), and most cases of cardioembolic stroke despite NOAC therapy are associated with subtherapeutic dosages or poor treatment adherence.
In our study population, considerably more patients suffered ischemic stroke while under NOACs than those taking VKAs. This is likely due to the increasing use of NOACs, which are recommended rather than VKAs in the current European Society of Cardiology guidelines as the first-line treatment for non-valvular AF.21 Among the NOAC drug class, rivaroxaban was most often used, possibly because it is the market leader in Portugal, while stroke was less commonly recorded in patients taking apixaban and edoxaban, which were launched more recently than the other two NOACs.
The overall rate of non-adherence to anticoagulant therapy was almost 40%, which is in line with previously published studies. In patients with stroke despite oral anticoagulation, treatment adherence was significantly better in those taking VKAs, suggesting that the regular monitoring of these patients’ INR has a positive effect on their adherence, and that mechanisms other than non-adherence are responsible for the occurrence of stroke despite anticoagulant therapy in these patients.2,3,5–14 Indeed, INR in this subgroup was almost always subtherapeutic, which may account for their greater vulnerability to thromboembolism.
Overall, adherence to anticoagulant therapy appears to be better in patients with a minimal educational level than in those who have completed primary education and those with a university degree, which may be because the former are more likely to be supervised by others when taking their medication.
Although laboratory tests can determine an individual's coagulation status and are used to monitor INR in patients taking VKAs, they cannot be used to assess adherence to NOAC therapy, since the results are more complicated to interpret and are highly dependent on the timing of testing in respect to the last intake of the drug.2,21 It is essential to educate patients at every consultation about mode of dosage (once or twice daily, with meals in the case of rivaroxaban), to emphasize the importance of full adherence to the prescribed treatment, and to explain how the patient's thromboembolic risk will increase if the NOAC is not taken, due to the rapid fall-off of its anticoagulant action. Measures that can improve treatment adherence include educating the patient about the importance of full adherence to anticoagulant therapy; involving family members, making sure that they too understand the importance of adhering to the prescribed dosage and thereby encourage the patient; producing an Anticoagulation Card that is provided to all of the patient's caregivers (including physicians, nurses, pharmacists and other health professionals); developing electronic systems to monitor treatment adherence; and providing technological aids to help patients remember to take their medication, including smartphone apps and electronic pill boxes. If poor adherence is still suspected despite several attempts at proper education and additional tools, conversion from an NOAC to a VKA may be considered.2
The prescribing errors found in our study demonstrate the importance of reviewing medication at outpatient visits in order to ensure that the effectiveness of oral anticoagulation and hence of thromboembolic protection are maintained.
The study's limitations include the small number of patients and its single-center nature, memory bias arising from the use of questionnaires to assess treatment adherence, and the acute clinical status of patients following stroke, which often means that data relevant to adherence must be collected from family members. There is the further limitation that information on type of AF was not available.
ConclusionIn patients who suffer ischemic stroke despite chronic anticoagulation for AF, INR is subtherapeutic in the great majority of those taking VKAs, whereas in patients taking NOACs the cardioembolic event may often be explained by poor treatment adherence. Dosages of these anticoagulants are also frequently subtherapeutic. In the majority of patients, stroke occurrence despite chronic anticoagulation appears to be explained by subtherapeutic dosage, poor treatment adherence or non-cardioembolic etiology, and not by inefficacy of the anticoagulants.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Fernandes L, Sargento-Freitas J, Milner J, Silva A, Novo A, Gonçalves T, et al. Acidente vascular cerebral isquémico em doentes previamente anticoagulados por fibrilhação auricular não valvular: por que acontece?. Rev Port Cardiol. 2019;38:117–124.