Cardiovascular disease, and particularly myocardial infarction (MI), carries a significant economic burden, through productivity losses (indirect costs) associated with temporary absence from work, that has not yet been adequately studied in Portugal. Our objective was to quantify the indirect costs of MI in the first year after admission.
MethodsConsecutive patients admitted to a single center aged <66 years who survived to discharge during a one-year period were included. Employment status on admission was assessed and for every employed patient, their monthly wage was estimated from market wage rates taken from the Ministry of Labor database according to gender and age. The duration of temporary absence from work was assessed in follow-up contacts for up to one year. Indirect costs were calculated in this sample and the results were applied to the number of MIs in Portugal during 2016 and separately to ST-elevation MI (STEMI) and non-ST-elevation acute coronary syndrome.
ResultsA total of 219 patients were included, of whom 66.2% were working. The mean monthly labor cost was 1802 euros. A total cost of 760 521.55 euros was obtained. At national level there were 4133 patients aged <66 years admitted with acute MI who survived to discharge. Costs were higher in STEMI patients and the total indirect cost was estimated at 10.12 million euros.
ConclusionsIn Portugal, the costs to society of disability-generated productivity losses exceed ten million euros in the first year after MI. Strategies to promote an earlier return to work are needed to lower these costs.
As doenças cardiovasculares, em particular o enfarte do miocárdio (EM), podem causar uma sobrecarga económica por perdas de produtividade (custos indiretos) associadas a ausência temporária do emprego, ainda não suficientemente estudada em Portugal. Foi nosso objetivo quantificar os custos indiretos do EM no primeiro ano após admissão.
MétodosIncluíram-se doentes consecutivos admitidos num único centro com < 66 anos durante um ano e que sobreviveram até à alta. Foi avaliado o estado de emprego na admissão e em cada doente empregado, foi estimado o salário mensal com base em dados de fontes públicas nacionais de acordo com sexo e idade. A duração de ausência de trabalho foi avaliada nos contactos de seguimento até um ano. Os custos indiretos foram calculados nesta amostra e aplicados para o número de EM em Portugal durante o ano de 2016 e separadamente para enfarte com supra-ST (EMST) e síndromes coronárias agudas sem supra-ST.
ResultadosForam incluídos 219 doentes, dos quais 66,2% estavam a trabalhar. O custo mensal médio foi de 1802 euros. Obtivemos um custo total de 760.521,55 euros. A nível nacional, foram admitidos 4133 doentes com < 66 anos com EM que sobreviveram até à alta. Os custos foram superiores nos doentes com EMST e estimámos um custo indireto em Portugal de 10.12 milhões de euros.
ConclusõesEm Portugal, os custos para a sociedade das perdas de produtividade condicionados pelas incapacidades excedem os 10 milhões de euros durante o primeiro ano após EM. Devem ser desenvolvidas estratégias para regresso mais precoce ao trabalho para reduzir os custos.
Chronic non-communicable diseases are the leading cause of death worldwide, including Portugal, where they account for 86% of all deaths.1 Among these, cardiovascular disease is the leading cause, representing 29% of all deaths.1 It also carries a significant burden for the health system, with more than 12 000 admissions for myocardial infarction (MI) per year.2 Cardiovascular disease leads to substantial consumption of health care resources but also to productivity losses. However, the costs to society caused by productivity losses (indirect costs) associated with temporary absence from work have not yet been adequately studied in Portugal. Also, due to important differences both in rates of employment by age and gender and in wages and social contributions across countries, results from one country may not be readily generalizable to others.
The aging of the population, with consequent reductions in the number of economically active individuals, has led to heavy financial demands and to problems with the sustainability of social protection systems, particularly in countries with high unemployment and early retirement, as was the case in Portugal in 2016. The increasing prevalence of chronic and disabling diseases is a significant factor in this major problem. In the near future, there will likely be an increase in the incidence of MI, due to both the aging of the population and increasingly unhealthy lifestyles.3 Although there has been a sustained decrease in mortality due to MI over the years, this is a chronic disease and the associated long-term complications must be dealt with.2,3 These include limitations in quality of life, with disabilities and consequent temporary absences from work.
Our objective in this paper was to quantify the indirect costs of MI due to absenteeism in the first year after admission, including potential differences between patients with ST-elevation MI (STEMI) and non-ST-elevation acute coronary syndrome (NSTE-ACS).
MethodsPopulationAll consecutive patients admitted to the cardiology department of Santa Marta Hospital aged <66 years (official retirement age) between July 2016 and July 2017 with MI and who survived to discharge were included in the present study. Demographic characteristics, clinical variables, treatment and outcome were obtained for each patient. Employment status on admission was assessed in every patient. All those reporting any form of regular paid work were considered employed. In subsequent follow-up contacts, performed at 30 days and one year after admission by telephone interview with a dedicated nursing team, the total duration of absence from work after the MI episode and any change in employment status during this period were assessed. The number of days absent from work for cardiology appointments and exams was also assessed.
To obtain the national numbers of patients with MI, the national Diagnosis-Related Group database was searched and all patients were selected with episodes in which the primary diagnosis was classified as CM-410 in the International Classification of Diseases (ICD)-9 or CM-I21 in the ICD-10 during 2016 (latest available data).4 For the present analysis, only patients aged <66 years were included.
Indirect costsEstimation of indirect costs followed the human capital approach, whereby productivity losses can be proxied by the cost of labor to employers. Monthly wages were estimated from market rates from the Ministry of Labor database (grossed up by social security contributions) according to gender and age in 2016 (Supplementary Table).5 Additional regular wage values were included on top of the base wage. These figures were adjusted for Social Security contributions by multiplying by 1.2375, because the economic value of lost production is based on gross wages and includes employers’ contributions to Social Security (23.75%). Other irregular wage components were also included in the estimates but not grossed up by contributions. Wages estimated on the basis of 2016 data were updated to 2018 using an index published regularly by the Bank of Portugal covering changes in wages reported to Social Security.
A daily cost was calculated to assess the cost of temporary absence from work by multiplying the monthly wage by 14/365. These figures assume weekends and holidays were included in the reporting of sick leave. The total cost of temporary absence from work (sum of the costs for each working patient) was calculated in this sample and the results were applied for the total number of MIs in Portugal during 2016. Indirect costs also included absence from work for cardiology appointments and exams, assuming a half-day absence from work for each. A strict definition of indirect costs was adopted in accordance with the guidelines of the National Authority for Medicines and Health Products (INFARMED).6 Data from the Portuguese Registry on Acute Coronary Syndromes (ProACS) were used to adjust our results for national data.7
Statistical analysisContinuous data are presented as means ± standard deviation if they presented a normal distribution and as medians for data without a normal distribution, as assessed by the Kolmogorov-Smirnov test. Categorical variables are described as frequencies and percentages.
The variable ‘number of days absent from work’ was highly skewed, and so a natural logarithmic transformation (Ln) was performed that was used in the subsequent regression analysis.
Linear regression analysis was performed to identify predictors of ‘Ln absent days from work’. All variables with p<0.10 were included in the multivariate model.
The statistical analysis was performed with IBM SPSS, version 20 and STATA, version 14. A p-value below 0.05 was considered statistically significant.
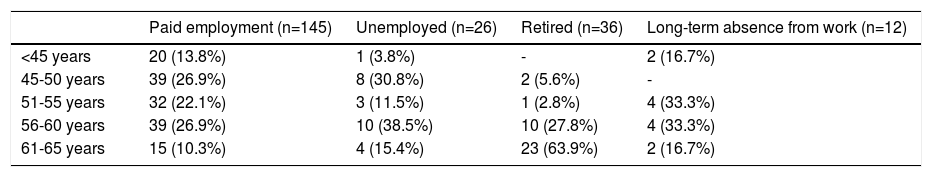
ResultsOverall resultsDuring the study period, 233 patients aged <66 years were admitted to our cardiology department with an acute MI. Fourteen patients who were foreigners passing through Portugal or Portuguese nationals working in other countries were excluded from the present analysis. The final sample included 219 patients, with a mean age of 54±7 years (25-65 years), 83% male, 66.2% actively working, 16.4% early retired, 11.9% unemployed and 5.5% in long-term absence from work due to noncardiac disease (Table 1). A significant proportion of patients had retired before the age of 60. During the one-year follow-up, there were no changes in employment status.
Employment status by age group.
| Paid employment (n=145) | Unemployed (n=26) | Retired (n=36) | Long-term absence from work (n=12) | |
|---|---|---|---|---|
| <45 years | 20 (13.8%) | 1 (3.8%) | - | 2 (16.7%) |
| 45-50 years | 39 (26.9%) | 8 (30.8%) | 2 (5.6%) | - |
| 51-55 years | 32 (22.1%) | 3 (11.5%) | 1 (2.8%) | 4 (33.3%) |
| 56-60 years | 39 (26.9%) | 10 (38.5%) | 10 (27.8%) | 4 (33.3%) |
| 61-65 years | 15 (10.3%) | 4 (15.4%) | 23 (63.9%) | 2 (16.7%) |
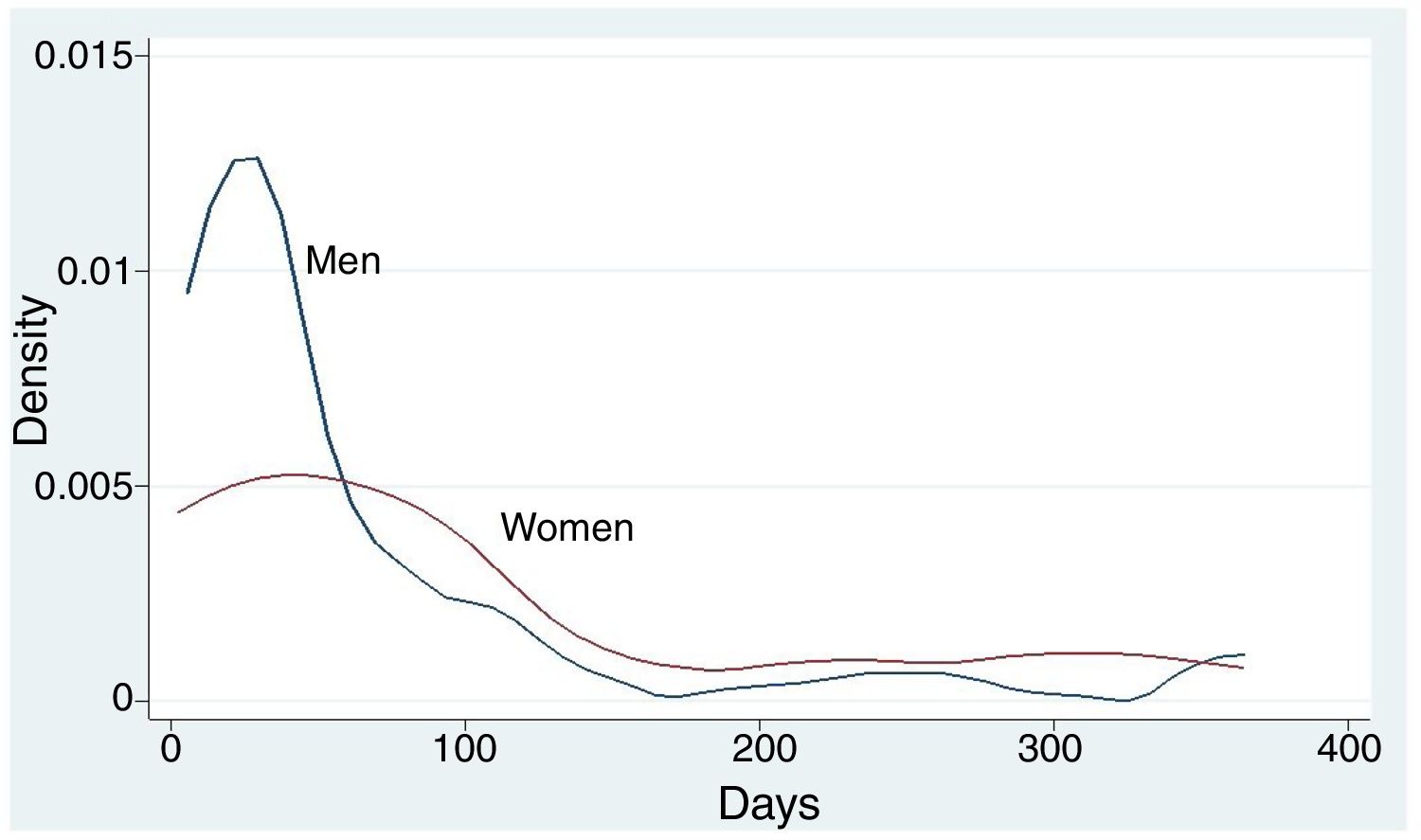
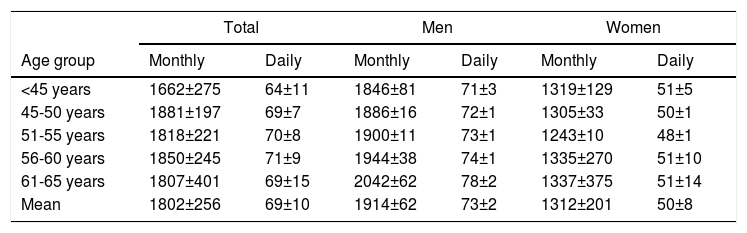
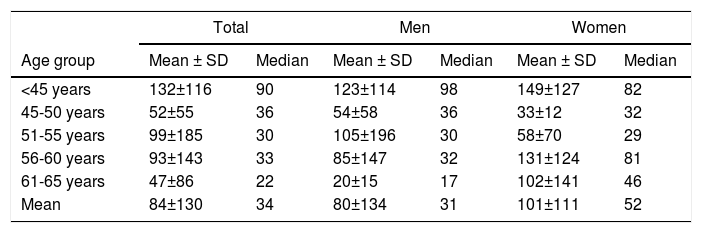
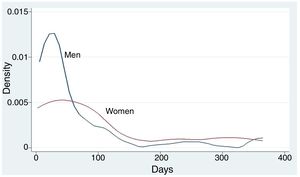
Mean labor costs are presented in Table 2. In our sample, the mean monthly labor cost of working individuals was 1802 euros (69 euros/day), higher in males. The median number of days absent from work was 34 days (31 days in men and 52 days in women) (Figure 1 and Table 3). In total, there were 10 679 days of absence from work in this population and 285 cardiology appointments or exams (median two half-days each), with a total cost of 760 521.55 euros (sum of the costs for each employed patient). The mean indirect annual cost was 5244.97 euros per patient employed. Adjusting for the proportion of working individuals, the mean annual indirect cost was 3472.17 euros per patient.
Mean wages (monthly and daily) in the working population, stratified by age and gender (in euros).
| Total | Men | Women | ||||
|---|---|---|---|---|---|---|
| Age group | Monthly | Daily | Monthly | Daily | Monthly | Daily |
| <45 years | 1662±275 | 64±11 | 1846±81 | 71±3 | 1319±129 | 51±5 |
| 45-50 years | 1881±197 | 69±7 | 1886±16 | 72±1 | 1305±33 | 50±1 |
| 51-55 years | 1818±221 | 70±8 | 1900±11 | 73±1 | 1243±10 | 48±1 |
| 56-60 years | 1850±245 | 71±9 | 1944±38 | 74±1 | 1335±270 | 51±10 |
| 61-65 years | 1807±401 | 69±15 | 2042±62 | 78±2 | 1337±375 | 51±14 |
| Mean | 1802±256 | 69±10 | 1914±62 | 73±2 | 1312±201 | 50±8 |
Mean and median days of absence from work attributable to myocardial infarction in the employed group, stratified by age group and gender.
| Total | Men | Women | ||||
|---|---|---|---|---|---|---|
| Age group | Mean ± SD | Median | Mean ± SD | Median | Mean ± SD | Median |
| <45 years | 132±116 | 90 | 123±114 | 98 | 149±127 | 82 |
| 45-50 years | 52±55 | 36 | 54±58 | 36 | 33±12 | 32 |
| 51-55 years | 99±185 | 30 | 105±196 | 30 | 58±70 | 29 |
| 56-60 years | 93±143 | 33 | 85±147 | 32 | 131±124 | 81 |
| 61-65 years | 47±86 | 22 | 20±15 | 17 | 102±141 | 46 |
| Mean | 84±130 | 34 | 80±134 | 31 | 101±111 | 52 |
SD: standard deviation.
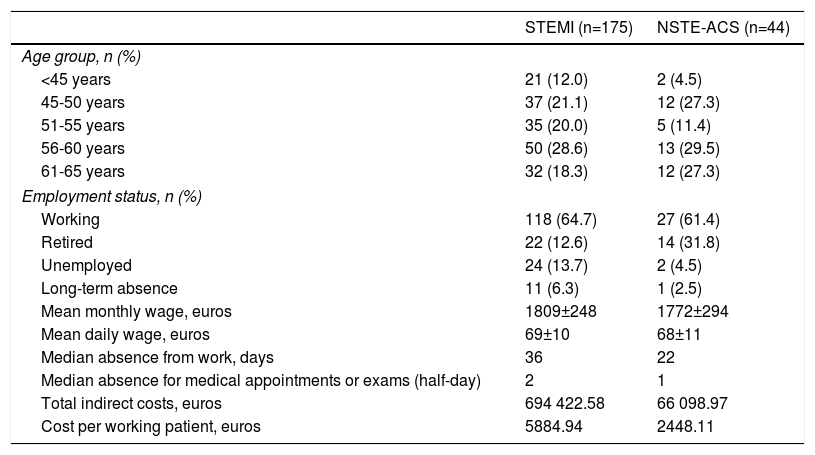
The above estimate of the mean indirect cost per patient does not take into account the large differences between patients with STEMI and those with NSTE-ACS.7 Significantly higher costs were obtained in STEMI patients, despite similar wages in the two groups (Table 4). This results in a mean total cost of absence from work of 5884.94 euros per patient with STEMI and of 2448.11 euros for NSTE-ACS.
Demographic characteristics and costs for ST-elevation myocardial infarction and non-ST-elevation acute coronary syndrome patients.
| STEMI (n=175) | NSTE-ACS (n=44) | |
|---|---|---|
| Age group, n (%) | ||
| <45 years | 21 (12.0) | 2 (4.5) |
| 45-50 years | 37 (21.1) | 12 (27.3) |
| 51-55 years | 35 (20.0) | 5 (11.4) |
| 56-60 years | 50 (28.6) | 13 (29.5) |
| 61-65 years | 32 (18.3) | 12 (27.3) |
| Employment status, n (%) | ||
| Working | 118 (64.7) | 27 (61.4) |
| Retired | 22 (12.6) | 14 (31.8) |
| Unemployed | 24 (13.7) | 2 (4.5) |
| Long-term absence | 11 (6.3) | 1 (2.5) |
| Mean monthly wage, euros | 1809±248 | 1772±294 |
| Mean daily wage, euros | 69±10 | 68±11 |
| Median absence from work, days | 36 | 22 |
| Median absence for medical appointments or exams (half-day) | 2 | 1 |
| Total indirect costs, euros | 694 422.58 | 66 098.97 |
| Cost per working patient, euros | 5884.94 | 2448.11 |
NSTE-ACS: non-ST-elevation acute coronary syndrome; STEMI: ST-elevation myocardial infarction.
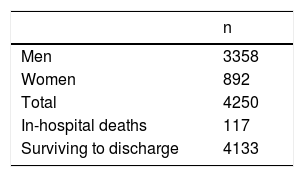
In 2016 in Portugal, 4133 patients aged <66 years were admitted with MI who survived to discharge (Table 5). Based on data from ProACS, the proportion of STEMI vs. NSTE-ACS in the previous five years was 41% vs. 59%.7 In 2016, according to these proportions, 1695 patients would have had STEMI and the other 2438 NSTE-ACS, which would correspond to 1097 working patients in the STEMI group and 1497 working patients in the NSTE-ACS group, according to the proportions obtained in our sample (Table 4). We estimate a total indirect cost of 6 455 779.18 euros for STEMI and 3 664 820.67 euros for NSTE-ACS (total indirect cost of 10 120 599.85 euros).
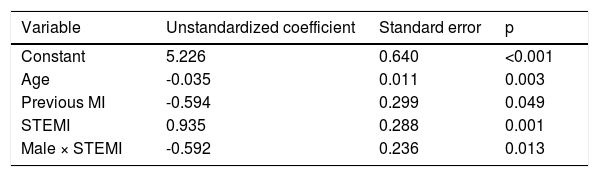
Predictors of absence from workIn univariate analysis of the working population, potential predictors of absence from work were age, previous MI, STEMI and gender. In this preliminary analysis, gender was a significant variable, but in a more detailed analysis, gender was only significant when associated with admission diagnosis, and so an interaction term of ‘gender’ × ‘main diagnosis’ was introduced in the final regression model. In this multivariate linear regression analysis, the most important clinical predictors of the number of days absent from work were age, previous MI, STEMI and male gender in STEMI patients (Table 6).
Multivariate linear regression analysis for ‘Ln number of days absent from work’.
| Variable | Unstandardized coefficient | Standard error | p |
|---|---|---|---|
| Constant | 5.226 | 0.640 | <0.001 |
| Age | -0.035 | 0.011 | 0.003 |
| Previous MI | -0.594 | 0.299 | 0.049 |
| STEMI | 0.935 | 0.288 | 0.001 |
| Male × STEMI | -0.592 | 0.236 | 0.013 |
Ln: natural logarithmic transformation; MI: myocardial infarction; STEMI: ST-elevation myocardial infarction.
This study estimated that MI-related productivity losses in the first year after the event have an annual indirect cost in Portugal of over ten million euros. However, although only patients aged <66 years were analyzed, a substantial proportion of the study population were not employed at the time of admission, which translates into lower costs to society.
Cardiovascular disease has a considerable impact on society, in terms of both direct costs incurred in its management and indirect costs related to absenteeism, lost productivity, and mortality. Total costs exceed those for any other major diagnostic group.3 In Europe, there was a steady increase in incident cases of cardiovascular disease between 1990 and 2015 in both women and men (11% and 17%, respectively) in high-income countries, following increases in life expectancy.3 Despite its relatively low per capita gross domestic product and gross national income, Portugal is included in this high-income group of countries. Consistent declines in cardiovascular disease-related mortality have seen cancer becoming a more common cause of death in some high-income countries, particularly in men.3 In Portugal, the same steady decrease in mortality due to cardiovascular disease is observed, but it is still, in general, the leading cause of death.2 Improvements in the accessibility and affordability of health services and the educational level of the population in these high-income countries may explain this reduction in mortality. However, this could be threatened by the emerging obesity epidemic, which is associated with increasing rates of diabetes in all countries.3 The disease burden is also illustrated by disability-adjusted years (DALYs) lost to ischemic heart disease, which in 2015 represented 11% of all causes of DALYs in females and 14% in males.3
Although cardiovascular disease is more prevalent in older patients, it is also diagnosed in a substantial number of working-age patients. Indirect costs due to lost productivity therefore account for an important part of the total costs of cardiovascular disease.8 In Europe, indirect costs associated with productivity losses make up 21% of the total costs of cardiovascular disease.9
Studies in other countries report an important burden in indirect costs after MI. In South Korea in 2012, US$37 million in productivity losses were reported in 236 339 patients with MI.10 Another study reports indirect costs of US$9.6 billion for 865 000 admissions per year in the US for coronary artery disease in general, not specifically MI.11 In Sweden, indirect costs of 9866 euros per working patient (3453 euros considering the entire sample) were estimated in a 12-month follow-up.12 However, there are substantial differences between countries in wages and social security contributions (or other additional contributions), which makes it difficult to compare results. For this reason, country-specific analysis is necessary to better understand the extent of the problem.
The incidence of MI is higher in men, and the overall indirect costs classified by gender were unbalanced, with a greater overall economic burden in males. However, the number of days absent from work per patient was higher in women, in whom the daily wage is lower and thus the impact is less significant. This however raises some concern, because it can be seen from national data that the wage difference between genders is decreasing in younger people, with a reduction of gender inequalities (Supplementary Table 1).5 Thus, if the incidence of MI in currently young women increases in the future, a rapid increase in costs can be expected. This suggests that not only it is important to implement strategies to promote an earlier return to work at younger ages, but it is also worthwhile doing so in older age groups.
In the subgroup analysis, it can be seen that although daily wages are similar in the two groups, the mean total indirect cost per working patient is much higher in STEMI patients than in NSTE-ACS patients, mainly due to longer absence from work. Despite the lower prevalence of STEMI patients, the final aggregate cost is substantially higher. If the epidemiology of MI is tending to change in terms of proportions, favoring STEMI, the associated costs will inevitably increase.
Our results show a surprisingly low value for indirect costs in the first year after MI. This result can be interpreted as another important aspect of improvements in health care in this domain. There have been improvements not only in mortality but also in terms of indirect costs due to absenteeism. However, additional improvements can be achieved. Cardiovascular disease is still undervalued in health policies. Action should be taken to address this issue, including possible interventions to further reduce absenteeism after MI, particularly in women. Premature retirement associated with MI, although not seen in this sample, should also be addressed. In this regard, cardiac rehabilitation is an important strategy that should be extended to a larger population of patients with MI, as recommended in international guidelines.13 Measures to adapt working conditions to patients’ situation are another possible approach. Both are modifiable factors that should be addressed. These measures are probably cost-effective by providing productivity gains, but this warrants further study.
One important finding in our study is that the median absence from work is substantially longer in the group aged <45 years of age, in both genders. This may be related to the fact that work is usually more demanding and intense in this age group, which could lead to a delay in return to work. This highlights the importance of measures, such as cardiac rehabilitation, particularly in younger patients, to promote an earlier return to work.
LimitationsUnit values of production, relying on wages, were estimated through official statistics and were based on gender and age group. This methodology provides only a rough estimate of individual values. Nevertheless, of all available options, to our knowledge this approach is the most appropriate.
In the present study, it was not possible to assess whether return to work was complete or whether productivity on return was somewhat reduced, which could have increased indirect costs further.
Although the retirement age is 66 years, some individuals remain in the labor force for longer periods. Our analysis only studied patients aged <66 years. Had we included older age groups, more indirect costs would probably have to be considered.
In addition, no indirect costs were calculated resulting from premature death in individuals at active ages or from productivity losses in individuals working in jobs outside the formal market but with social value (such as housewives).
Due to the relatively short follow-up, our data were also not suitable to study the influence of MI on early retirement.
Indirect costs were estimated on the basis of a single urban center. However, this is a tertiary hospital, and patients from peripheral hospitals who were referred to our hospital for coronary angiography were also included in the analysis. For this reason, the data are to some extent representative of the national situation. It has also been shown that in high-income countries such as Portugal, rates of major cardiovascular events and death are similar in urban and rural areas, particularly in countries with universal coverage, ensuring good health services access and treatment in both urban and rural areas.14 This is expected to be the case in Portugal, with possible exceptions in a few regions.
ConclusionsIn Portugal, the burden of indirect costs for the first year after MI is over ten million euros. Strategies to promote an earlier return to work are needed to lower these costs. Prioritization of investment in health and social protection policies should also target patients with MI.
Conflicts of interestsThe authors have no conflicts of interests to declare.
We thank Professor Julian Perelman for providing information about the number of hospital admissions with MI during 2016.