Kounis syndrome (KS) is the coincidental occurrence of acute coronary syndrome (ACS) and anaphylactic or allergic insult. It results from mast cell degranulation with subsequent release of numerous inflammatory mediators, leading to coronary vasospasm or atheromatous plaque rupture. Diagnosis is clinical and based on the temporal relationship between the two events. Despite the growing number of reported cases, especially in southern Europe, the lack of awareness of this association may lead to under-reporting in Portugal. Recognition of KS, even if retrospective, has clinical implications since individual atopy must be investigated and desensitization measures should be employed, if possible, to prevent future events. We report the case of a 70-year-old man who was admitted to hospital because of generalized exanthema and itching and onset of chest pain while under observation. Coronary angiography confirmed coronary artery disease and ACS and he was diagnosed as having type II KS.
A síndrome de Kounis (SK) define-se como a ocorrência simultânea de uma síndrome coronária aguda (SCA) e de um insulto anafilático ou alérgico. Resulta da desgranulação de mastócitos e subsequente libertação de mediadores inflamatórios, responsáveis pelo vasospasmo coronário ou rutura da placa de ateroma. O diagnóstico é clínico e baseia-se na relação temporal entre os dois eventos. Apesar do número crescente de casos descritos, principalmente nos países do sul da Europa, o desconhecimento médico pode levar ao subdiagnóstico em Portugal. O reconhecimento da SK, mesmo realizado a posteriori, tem implicações clínicas, nomeadamente na investigação da atopia e medidas de dessensibilização, se possíveis, com vista à prevenção de novos eventos. Os autores relatam o caso clínico de um doente de 70 anos, que recorreu ao serviço de urgência por exantema generalizado e pruriginoso e iniciou dor torácica enquanto estava em observação. A angiografia confirmou SCA com evidência de doença coronária e subsequente diagnóstico de SK tipo II.
Kounis syndrome (KS), first described in 1991 by Kounis and Zavras,1 is defined as the coincidental occurrence of acute coronary syndrome (ACS) and anaphylactic or allergic insult. It results from mast cell degranulation with subsequent release of numerous inflammatory mediators, leading to coronary vasospasm or atheromatous plaque rupture. Diagnosis is clinical and is based on symptoms and signs of an acute allergic reaction – cutaneous (rash, itching, hives, angioedema), respiratory (dyspnea, wheezing, stridor) or gastrointestinal (abdominal pain, nausea, vomiting) – simultaneously with a setting suggestive of ACS. According to Cepeda et al.,2 the clinical history is essential for establishing a cause-effect relationship in time with the possible triggering factor, and so the patient's allergic history should be investigated, including allergy to latex, nuts or drugs, insect stings or bites, or recent use of new medications.
As KS represents a cluster of cardiovascular symptoms that result from an allergic insult, in most cases the clinical diagnosis is made retrospectively. There is no diagnostic test pathognomonic of KS, but there are some studies that suggest measuring levels of tryptase (at onset of symptoms and after two and 24 hours), histamine, complement, eosinophils and total immunoglobulin E (IgE). However, normal values of these parameters do not rule out the possibility of a previous allergic reaction.2 At the same time, given the suspicion of an ACS, an electrocardiogram (ECG) and serial measurement of cardiac enzymes should be performed.
There are currently no specific clinical guidelines for the treatment of KS, which should consist of treating the ACS and the allergic reaction in accordance with the type and severity of each. Although the two conditions should be treated appropriately, accurate diagnosis of the syndrome, even after the event, has clinical implications. The patient's atopy should be assessed and desensitization measures should be taken if necessary, given the risk of future allergic reactions that could trigger an ACS.3
The authors present a case of KS following a probable insect sting.
Case reportJ. H. B. C., male, 70 years, went to the emergency department due to exanthema and generalized itching. His symptoms had begun after a bicycle ride. He reported two previous episodes of generalized maculopapular erythema and itching after insect stings in the outer ear, five and two years before, which improved with medication. In the present episode, he had not detected an insect sting, and reported consuming no unusual foods or taking new drugs. He reported a personal history of hypertension and dyslipidemia, medicated with ramipril 5 mg daily and simvastatin 20 mg daily, respectively.
On arrival at the emergency department, around 30 min after symptom onset, he began to experience constricting chest pain radiating to the left arm, with no relieving or aggravating factors and not improved by sublingual nitroglycerin. He also reported general malaise but no fever, dyspnea, cough, expectoration, nausea, vomiting or other symptoms.
On physical examination the patient was apyretic and hemodynamically stable, with blood pressure 140/70 mmHg and heart rate 65 bpm. He presented generalized maculopapular erythema (Figure 1) and itching that spared the palms, soles and face. Cardiac auscultation revealed rhythmic heart sounds and no murmurs, while pulmonary auscultation detected normal breath sounds with no adventitious sounds. His abdomen was painless on palpation and there was no edema or other alterations in the lower limbs.
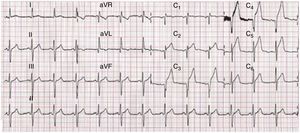
The ECG showed sinus rhythm with heart rate 72 bpm and ST-segment elevation of around 2 mm in V2-V6, DI and aVL (Figure 2). A provisional diagnosis was made of anterolateral ST-elevation myocardial infarction.
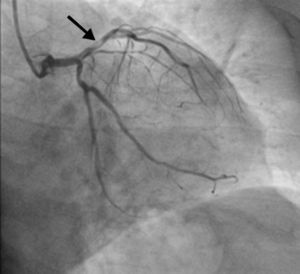
The hemodynamic team was activated and medication was begun with a loading dose of aspirin 300 mg, ticagrelor 180 mg and unfractionated heparin (5000 units). Emergency catheterization was performed (less than one hour after the onset of chest pain), which revealed a subocclusive lesion in the proximal left anterior descending (LAD) artery, severely calcified and with the appearance of a thrombus (Figure 3). A 50% ostial lesion in the intermediate branch and a <50% lesion in the mid right coronary artery were also visualized; the circumflex artery had no lesions. Primary angioplasty of the proximal LAD was performed, including thrombectomy and removal of thrombotic material, balloon predilatation and placement of a drug-eluting stent (DES) in the proximal LAD covering the origin of the first diagonal branch.
On laboratory testing, the first measurement of troponin I, 15 min after pain onset, was 0.01 ng/ml and peak level was 1.07 ng/ml. Blood tests showed no alterations; eosinophils were 8/μl (0.1% of white cells) and C-reactive protein was 0.20 mg/dl. Levels of tryptase, histamine, total IgE and complement were not measured. The patient's lipid profile revealed total cholesterol 138mg/dl, high-density lipoprotein cholesterol 44 mg/dl, low-density lipoprotein cholesterol 76 mg/dl, and triglycerides 89 mg/dl; hemoglobin A1c was 5.3%.
The patient's clinical course was favorable, with no recurrence of symptoms, and echocardiography showed preserved systolic function and no wall motion abnormalities, pericardial effusion or valve disease. The maculopapular erythema and itching regressed after a few hours with no treatment being required. The patient was discharged four days after admission and was referred for angioplasty follow-up and allergy consultations for study of atopy and possible allergen-specific immunotherapy (SIT).
Skin prick testing with Hymenoptera venom extract (1 μg/ml) and intradermal testing with bee and wasp venom were subsequently performed in immunoallergy consultations, which were positive for wasp venom. Screening for IgE specific to molecular allergens showed positivity for Ves v 1 and Ves v 5, and so the patient was referred for wasp venom SIT following an ultra-rush protocol in the allergy outpatient clinic, which was uneventful. He was prescribed aspirin 10 mg daily, ticagrelor 90 mg twice daily, atorvastatin 20 mg daily and ramipril 50 mg daily, together with antihistamine and oral steroids as required. He was also advised to carry a epinephrine auto-injector as a life-saver in case of an anaphylactic reaction and to avoid places likely to harbor wasps, and is due to continue monthly SIT for 3-5 years. He has been asymptomatic since the acute event.
DiscussionKS has mainly been described in southern Europe, especially in Spain, Italy, Greece and Turkey. This geographical variation may be due to greater knowledge of the syndrome among physicians, climatic and environmental conditions that lead to greater cross-reactivity with pollen and/or exposure to insects, excessive use of medications, and inadequate preventive measures.3 Despite Portugal's similarities and proximity to these countries, few cases have been reported in this country.4 It may be under-reported because of lack of awareness of the condition among physicians, even though it was first described a quarter of a century ago.
Most of the information on the syndrome is based on case reports. Multiple causes have been described, including environmental exposure (insect bites or stings, latex, plants), diseases (angioedema, asthma, hives, exercise-related anaphylaxis, Churg-Strauss syndrome), and drugs (analgesics, antibiotics, non-steroidal anti-inflammatory drugs, steroids, contrast media and others).2 The allergic insult is followed by mast cell degranulation and release of inflammatory mediators such as histamine, proteases, arachidonic acid products, platelet-activating factor and cytokines and chemokines,5 which can induce coronary spasm and erosion or rupture of atheromatous plaque or stented areas.
In the case described, although the triggering factor was not initially identified, the patient reported two similar previous episodes associated with insect stings, and as he had been in an environment likely to harbor insects, it was assumed that this situation had the same cause. The patient's subsequent clinical presentation while in hospital, suggestive of an ACS, meant he could immediately be assessed by a cardiologist and the hemodynamic team was activated. This prompt diagnosis and treatment led to a favorable clinical course. The time between the allergic reaction and the onset of the ACS was similar to that in other cases in the literature.6
There are three subtypes of KS:
Type I – without coronary artery disease (CAD): chest pain occurs during an acute allergic reaction in patients with no risk factors or coronary lesions, in whom the allergic reaction induces coronary spasm, leading to chest pain and ECG changes secondary to ischemia. The proposed mechanism is the release of vasoactive mediators following mast cell degranulation.3
Type II – with CAD: chest pain occurs during an acute allergic reaction in patients with pre-existing known or unknown atherosclerotic disease. The release of acute mediators can induce plaque rupture or erosion, resulting in myocardial infarction. According to Constantinides,7 even ordinary allergic reactions could promote plaque disruption.
Type III – associated with late DES thrombosis, in which mast cells and eosinophils have been identified in aspirated thrombus.8,9
In the case presented, a diagnosis of type II KS was made, in view of the occurrence of an allergic reaction (subsequently confirmed as being to wasp venom), together with ACS, with documented CAD (subocclusive lesion of the proximal LAD). Levels of tryptase, histamine, total IgE and complement were not measured, but these neither exclude nor confirm the diagnosis, which is basically clinical.
Since the allergic reaction was not severe, treatment was directed toward the ACS and there was no specific treatment for the allergy, which facilitated the patient's management. Treatment becomes a challenge when the allergic reaction is more severe, since drugs used separately for the two conditions may be contraindicated when used simultaneously in the same patient. This is particularly important for epinephrine, the treatment of choice in cases of a severe anaphylactic reaction, since in ACS epinephrine can aggravate ischemia, prolong the QT interval and induce coronary vasospasm or arrhythmias. There are currently no guidelines for the management of such cases. With regard to steroids, although they may delay scarring and cause alterations in the myocardial wall, they appear to be safe and effective, but further studies are needed.2 Treatment for the ACS consists of percutaneous coronary intervention for types II and III, while treating the allergic reaction may be sufficient in type I.
Even when diagnosis is retrospective and in the absence of definitive markers, the authors consider it essential to identify patients who may have KS. The allergic component should be identified in order to apply measures such as desensitization and avoidance of the trigger, to prevent such events in the future. If the patient's clinical history is relevant, as in the present case, a diagnosis of hypersensitivity (such as to insect stings) should be confirmed by skin prick testing and/or intradermal testing with venom followed by screening for specific IgEs, since in such cases SIT is indicated and has a high success rate (up to 98%).10 Thus, despite the lack of specific guidelines, the authors recommend referral for allergy consultations for all patients with KS, to prevent recurrence.
Some studies have reported that mast cell stabilizers like sodium cromoglycate, ketotifen, sodium nedocromil and lodoxamide could potentially suppress degranulation of mast cells but more exploration is needed to used them as prevention strategies.11
ConclusionSince it was first described, the number of cases of KS has risen steadily, although its true incidence is hard to determine. Further studies are needed to understand its epidemiology, clinical and diagnostic characteristics and therapeutic and preventive measures. The increasing number of cases means that more attention should be paid to this syndrome in order to prevent its occurrence in atopic individuals, since ACS has serious prognostic implications.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Marinheiro R, Amador P, Semedo F, Sá C, Duarte T, Gonçalves S, et al. Enfarte agudo do miocárdio intra-hospitalar: um caso de síndrome de Kounis tipo II. Rev Port Cardiol. 2017;36:391.e1–391.e5.